# 5094
Note: This is an update to of one my preparedness columns that has been very popular in the past. Instructions on how to set up a simple solar charging system for your home.
I re-run it about once a year.
As former live-aboard boater, I lived off the grid – using a solar system like I describe in this essay – for many months at a time.
During my 10 years living in Rural Missouri, we had several storm related power outages that lasted more than 24 hours, and were grateful for the 12 volt backup system I maintained.
Earthquakes, tornadoes, hurricanes, and other localized disasters can disrupt power supplies for hours or even days.
A little bit of preparedness now, can make things a whole lot easier to deal with later.
I’ve had several requests for information on how to construct a down and dirty (read : Cheap) solar power system for those with light duty requirements. If you are looking for a system to run power tools, a microwave oven, refrigerator, freezer, or your desktop computer . . . the system described below will be woefully inadequate.
However, if what you want is something cheap, easy to built, and that will allow you to recharge Ni-cad batteries and cell phones, run LED lights or 12 volt fans, and maybe give you a few hours a day on your laptop computer . . . then I present an inexpensive and easy to put together alternative.
With a bit of judicious shopping, a simple solar power setup can be had for a little over $200, and can be put together in an afternoon or two.
Increase your budget to $300 and you can more than double your capacity.
The price of solar panels continues to come down, with newer panels providing more watts per dollar. Deals can often be found by looking in surplus stores, by buying discontinued models, or by purchasing panels with cosmetic blemishes.
Is Solar for Me?
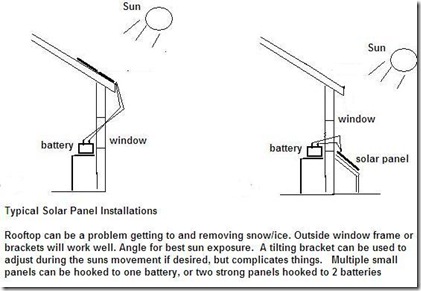
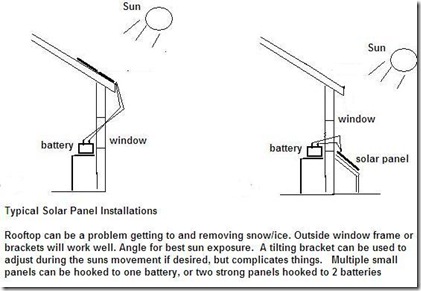
Solar power, of course, requires a good exposure to sunlight. The more sunlight you can access, the more efficient the output from your panels. If you live somewhere that has few sunny days, or you have no place to mount a solar panel that will catch good direct sunlight for 5 or 6 hours each day, the odds are that solar is not a good investment.
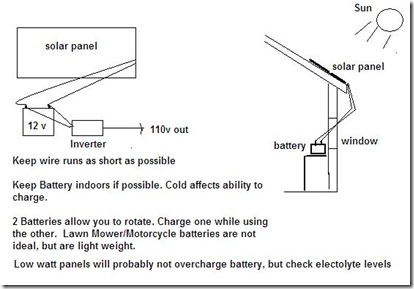
Simply put, solar panels generate small amounts of electricity from direct exposure of the cells to sunlight. Most solar panels generate 14 to 17 volts, enough to charge a 12 volt battery, and their ability to charge is rated in watts. A 15-watt panel generates 15 watts of electricity at roughly 15 volts each hour. This is roughly the equivalent of 1 amp of charging per hour into your battery.
Larger (more expensive) panels may produce 30, 40, 80, 120 watts of power (or more). For each 15 watts, think (roughly) 1 additional amp/hr. A 60-watt panel would therefore generate about 4 amps per hour during prime sunlight hours.
Of course, the electricity generated from a solar panel only is available when the sun is shining. At night, or when clouds obscure the sun, the power output stops. This is not very handy for those who would like to have lights at night. So to our solar panel we must add a storage device, a 12-volt battery or quite often, a bank of batteries. This allows us to bank electricity during the day, and draw it out, as needed, even during the night.
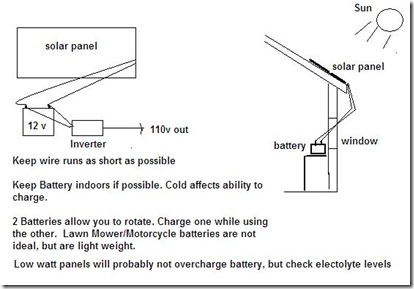
When we draw electricity from the battery bank, we can do so either as 12 volt or, with the aid of a device called an inverter, as 110 volt house current.

Think of a fully charged battery like a bucket filled with water. When you run LED lights, or convert power to 110v with the inverter, you are removing water. Sometimes, like with the LED's you take little sips, other times, when using the inverter, you take massive gulps. Either way, the amount of the water in the bucket goes down until it is empty.

The solar panel adds very small amounts of water to your bucket every hour the sun shines on it. The amount of water it adds is determined by the amount of direct sunshine and the watt rating of the solar panel.
As long as you add as much back to your bucket each day as you draw out, the battery remains fully charged. If you draw out too much, the battery is partially discharged, and you will have to wait several days for the solar panel to catch up.
The Solar Triad +1
To create a Solar Power system, you need basic components. The solar panel, a battery, and an inverter. You could get by without an inverter and only draw out 12 volt power from your batteries, but that is very limited, and as you will find, small inverters are very inexpensive. I would also add a 4th item, an inexpensive battery charger, for those times when the grid is up, so you can quickly recharge your batteries.
A 15 watt solar panel can often be purchased for around $100. A suitable battery, for less than $60. And a 400watt inverter will run you about $22. All totaled, you can be in business for roughly $200. Not bad.
If your solar panel is larger than 15 watts, you'll probably want to add a solar panel charge controller. These run around $30, and can prevent overcharging of your batteries. If you use a small solar panel, they are not necessary.
To that, I would recommend an automotive battery charger, which will run about $25, although they can often be found for much less in yard sales. A 6/2 amp charger is fine. This will allow you to top off your battery during those times the grid is functioning. And by adding a 2nd battery, you can be using one battery while charging another. Total cost? Right at $300.

Most batteries will tell you how many amp/hrs they are rated for. This is not the same thing as cranking amps. Those are for short duration, and are for turning a starter on a car or engine. The best batteries are called deep cycle, or marine batteries, and typically can hold 105 amps or more. But they are heavy. Smaller batteries may only hold 10 or 20 amps. As long as your daily energy needs never exceed that, they could be used.
An LED light array will draw very little from the battery. Probably .1 amps an hour. 1 amp every 10 hours. You could go a long time without recharging.
But the inverter, which provides 110v, draws amps from the battery at an astounding rate. A 100 watt light bulb will pull 10-12 amps out of your battery in an hour. Using an appliance that uses the full 400 watt output would pull 40+ amps out in an hour. It would take days for the solar panel to replenish that much power.
The best use for the inverter is for running battery chargers for ni-cad batteries, or very occasionally to run a small portable tv, radio, or laptop computer. You will not be able to run a microwave, or a toaster, or power tools.
Of course, bigger solar panels and bigger batteries, and a bigger inverter would allow you to do these things. But based on what you are likely to have, you need to have low expectations.
A good investment are Ni-cad or Nickle-Hydrate (expensive, but better) rechargeable AA and AAA batteries, with a charging stand. This will allow you to have rechargeable batteries (using the inverter) to run cell phones, radios, even walkie-talkies.
Where possible, you should use the battery for the lowest possible power consumption. LED lighting, or charging AA and AAA batteries. A windup radio will take a burden off of your system.
Warning: Batteries can offgas Hydrogen gas, which can be explosive, and should be kept in a ventilated area. You will also need to check the electrolyte levels of the batteries and keep the plates covered with distilled water.
Solar panels, batteries, and inverters produce electrical currents and (even at low voltages) can be a dangerous shock hazard. Always read and follow the instructions that come with your solar panels, batteries, chargers, and inverters.
If you are unsure of how to safely deal with these components, have someone who knows how give you instruction.