Anatomy
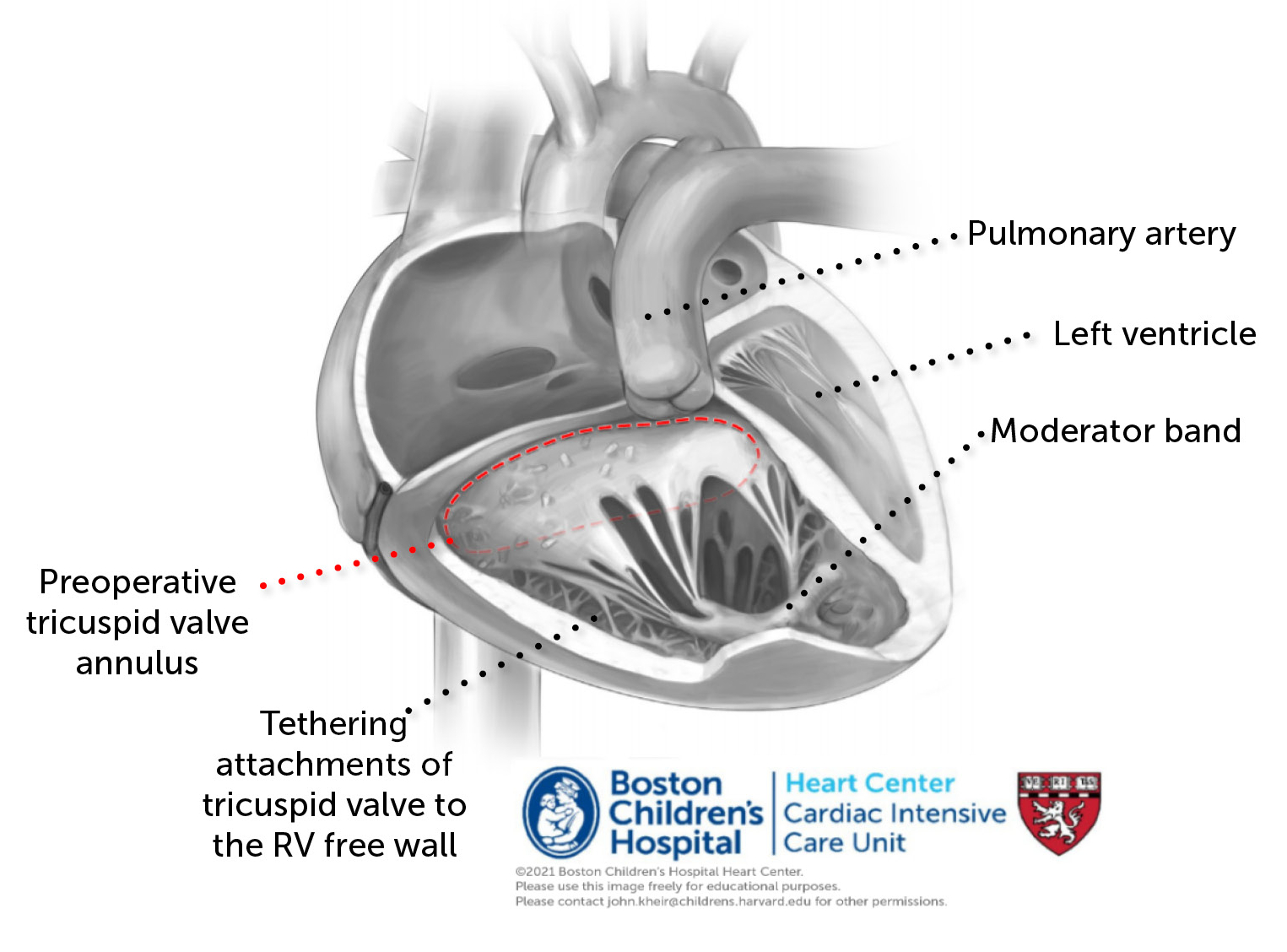
- The primary pathology of Ebstein’s anomaly is a spiral displacement of the tricuspid valve annulus towards the ventricular apex. Posterior and septal TV leaflets are often adherent to the ventricular septum, tethering the valve to the endocardium, limiting coaptation and causing TR. Because of this displacement, a significant portion of the RV is on the atrial side of the TV, chronically exposed to low pressure (because the atrium is very compliant, RAP is typically quite low). Thus, a significant portion of the RV is ‘atrialized’ and does not thicken normally; this causes major problems in the sickest infants. When TR is severe, the RA becomes profoundly dilated (can comprise the majority of the chest cavity). Importantly, this creates a pathologically compliant chamber which functionally ‘absorbs’ the kinetic energy of systemic venous return. In the most severe cases, this diminishes RA to LA shunting and causes the LV to be underfilled (appearing ‘compressed’ by the atrialized RV). Diminished antegrade RV stroke volume may cause the pulmonary valve to be hypoplastic or even atretic. In some cases, a dilated RV (specifically infundibulum) may create pulmonary regurgitation. In the most severe cases, profound RA dilation may cause pulmonary compression and hypoplasia.
Ebstein’s Anomaly of TV
Physiologic phenotypes of Ebstein’s anomaly
The spectrum of Ebsteins is highly variable, with the following general phenotypes.
- Babies with severe TR may be preterm and may exhibit hydrops, hypoplastic lungs, wall-to-wall heart, and shock state. Among the factors to pay attention to, the RV pressure (estimated by TR velocity jet, a marker of tricuspid valve competence) and the presence of PR (or functional pulmonary atresia) are the most significant; the presence of severe PR and/or an RVP<15 mmHg are significant risk factors. In the presence of pulmonary regurgitation, a circular shunt may cause a severe shock state (low BP, low UOP, high serum lactic acid) in which a fraction of blood flows: LV- >Ao->PDA->retrograde PA flow into RV-> RA-> LA-> LV. This may improve with PDA ligation if the RV generates sufficient PBF once the PA pressure is subsystemic (by ligating PDA and use of iNO). However, in some patients the circulation is acutely insufficient following PDA ligation, in which cases it may be necessary to support with ECMO and perform an emergency RV exclusion procedure. Repair or replacement of the TV in this situation is unlikely to be successful due to failure of the atrialized RV, which fails to fill the LV and dominates the clinical phenotype.
- In acutely ill newborns, severe TR may cause symptoms by limiting PBF, causing increased dead space ventilation and a shock state. While hypoxemia can occur via atrial shunting, shock is more common as the RA and RV form a highly capacitant energy sink which leads to a deficiency of LV preload; this causes the septum to shift into the LV. In some cases, this may improve with therapies to decrease PVR (e.g. ventilation, hyperoxia, iNO, and surfactant if indicated).
- In other infants, TR may be mild-moderate and well tolerated. Such infants may have a less compliant atrium and more well developed lungs, and therefore may exhibit only mild hypoxemia or respiratory insufficiency, may have mild feeding intolerance, or may be asymptomatic. Such infants may be managed expectantly until a definitive indication for surgery arises. Many infants with Ebsteins anomaly are asymptomatic and do not require CICU admission.
- As patients grow, TR may worsen as the RV becomes progressively more volume loaded which worsens TR (because of TV tethering to the septum. In older children, adolescents, and adults, the Cone procedure provides a durable and effective repair of the TV. Older patients often present with either signs of heart failure or exercise intolerance due to RV volume overload or hypoxemia, or due to re-entrant arrhythmia. Arrhythmias are quite common in Ebstein’s anomaly due to accessory pathways between the atrium and ventricle. In some patients, off-loading RV volume via atrial shunt or BDG may improve hemodynamics.
Repairs
- Cone Repair
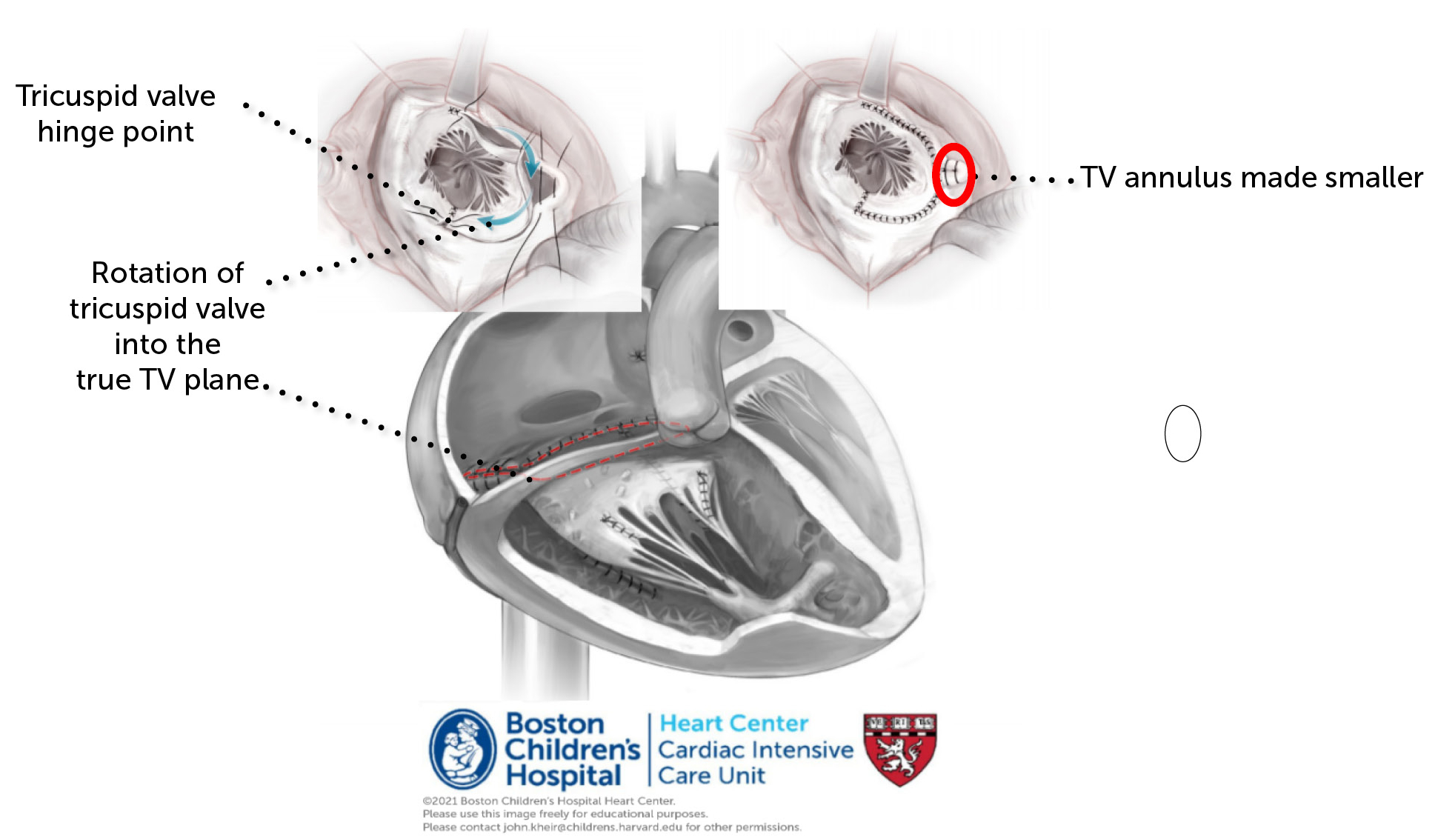
- The Cone repair involves the following steps: (1) takedown of the tricuspid valve along a portion of the anterior leaflet and all of the posterior leaflet, as well as delamination of the leaflets off of the endocardial surface to mobilize TV tissue. (2) The medial aspect of the freed posterior leaflet is rotated clockwise (surgeon’s view) and sutured to the free anterior septal edge. The remainder of the valve is then sutured to the true tricuspid annnulus (TTA). (3) The TTA is aggressively plicated circumferentially around the valve. The free wall of the RV may be also plicated down to decrease RV dilation and afterload. (4) The ASD is usually subtotally closed to allow for right to left atrial shunting. Rarely, a BDG may be performed to diminish RV work.
- Postoperative considerations
- The Cone repair has extensive suture lines that are at risk for dehiscence. Major tenets of care include: (1) Prevent rapid volume boluses, which may cause RA stretch. Venoconstrictors (e.g. NE) and inotropes may stabilize the circulation. (2) Consider maintaining sedation and NMB in complex repairs for several days; the highest risk time is during coughing and valsalva which increase atrial pressure acutely. (3) Minimize RV afterload by preventing atelectasis, iNO when concerned. Monitor RA pressure.
- RV Exclusion Procedure
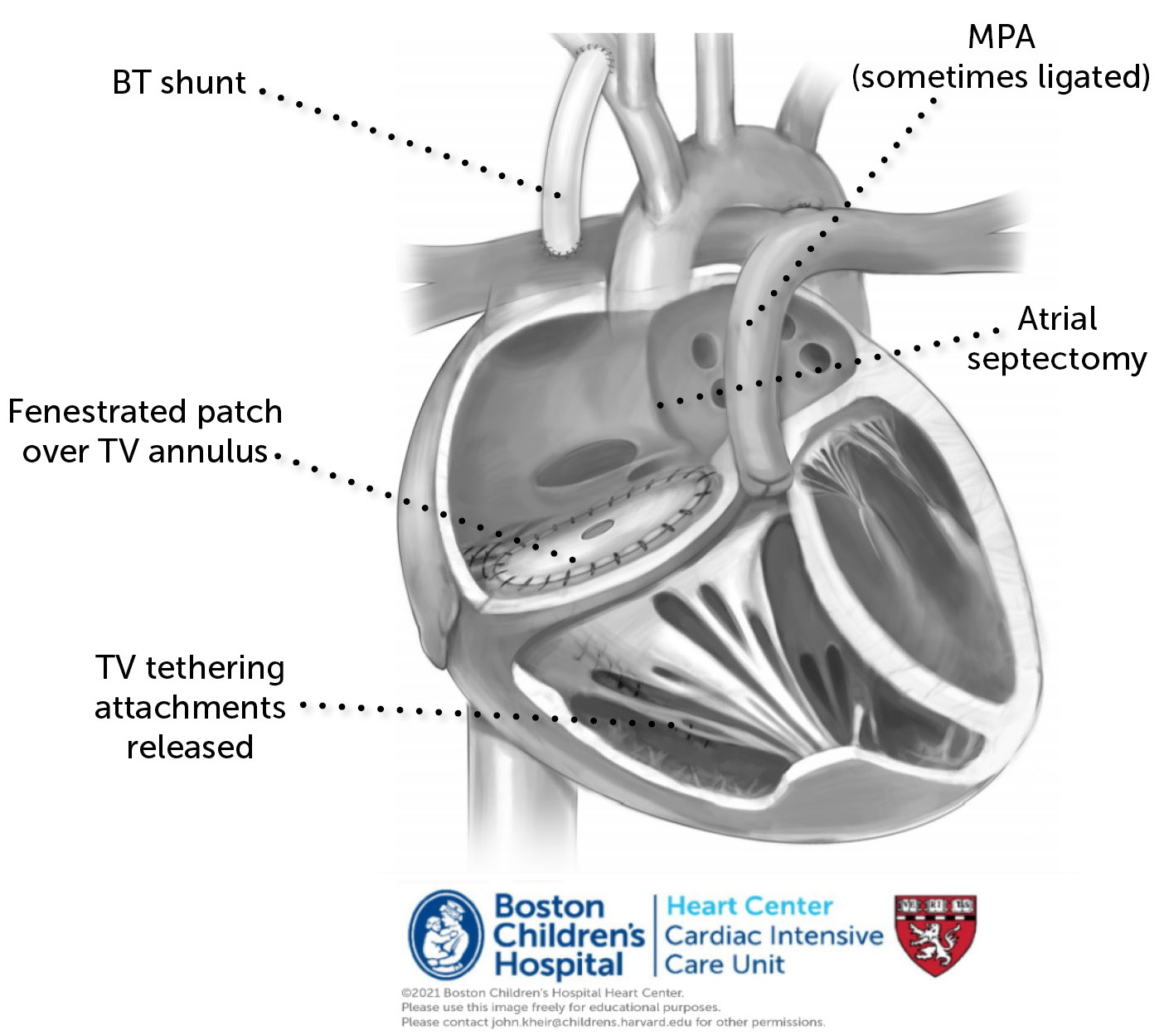
- The RV exclusion procedure (aka Starnes procedure) is useful in cases in which the RV is not able to support a portion of the cardiac output, and instead creates an energy sink due to its pathologically elevated capacitance. The procedure involves a fenestrated patch sewn over the true TV annulus, RA reduction plasty, and atrial septectomy, which together decrease the compliance of the RA and significantly improve LV preload. The MPA may be oversewn in cases of PR. A BTS or PDA stent may be provided for PBF.
- Postoperative considerations
- Often patients return with an open sternum. Postoperatively, the primary tenets of care will be the management of any bleeding and the maintenance of LV preload; maintaining LV preload can be more challenging when there is postoperative bleeding or if the RV has not been sufficiently plicated. Minimization of systemic vascular resistance (as tolerated by BP) is important to optimize systemic blood flow and minimize PBF. Following hemostasis, anticoagulation is often started for the BTS.
References
Arrhythmia in Ebstein
Sherwin ED, et al.; Card Elevtrophysiol Clin 2017.
Preoperative physiology, imaging and management of Ebstein’s anomaly of the TV
Morray B; Semin Cardiothorac Vasc Anesth 2016.
1950, Circulation – Taussig describes 3 neonates with Ebstein’s [PDF]
2018, ATS – STS experience with Ebstein’s [PDF]
2017, Ann Thor Surg – Taiwan experience with7 neonates undergoing biV repair [PDF]
2016, Circulation – UCLA experience with Starnes in neonates [PDF]