Nail Bed Laceration
History:
24-year-old right hand dominant male with no significant past medical history presented with a lacerated right index finger nail bed and distal fingertip with a minimally displaced distal phalanx tuft fracture after sticking his hand in a fan blade at a cattle show earlier that day.

Fig.1. Right hand, laceration of 2nd finger

Fig.2. Xray of right hand. Minimally displaced tuft fracture of 2nd distal phalanx
Findings:
The nail and nail bed were lacerated with exposed distal phalanx. The nail plate was lacerated transversely, completely. It appeared the soft tissue could cover the bone. Xray indicated minimally displaced tuft fracture of distal phalanx. The patient could demonstrate extension and flexion of the distal interphalangeal joint indicating intact motor (FDP, FDS, and EDC). Sensation from radial and ulnar digital nerves was also intact. The distal fingertip was warm with intact capillary refill.
Diagnosis:
Right index finger distal phalanx minimally displaced tuft fracture with nail bed and soft tissue lacerations.
Differential Diagnoses:
- Nail plate laceration without underlying nail bed laceration
- Germinal matrix laceration
- Matrix loss
- Seymour Fracture (in pediatrics)
- Partial amputation with or without devascularized tip
- Bony mallet finger
Workup Required:
PA, lateral, and oblique radiographs of the hand to assess for phalanx fracture.
Plan:
Removal of nail plate for repair of the nail bed and soft tissue of distal phalanx. Cover the exposed bone by repairing soft tissue. Cap splint for tuft fracture.
Expertise Needed:
Plastic Surgeon or hand surgeon. Emergency Physician trained in nail bed repairs, if simple nail bed laceration.
Treatment:
Local anesthesia with 1% lidocaine with epinephrine provided a digital block. The hand was prepped with betadine and draped using sterile towels. A portion of a sterile glove was used as a digital tourniquet for the right index finger. Once the digit was anesthetized, a freer elevator was used to lift the two fragments of the nail plate from the nail bed using an upward force to peel the nail plate away from the underlying nail bed incision. The entire laceration of the nail bed was visualized and then copiously irrigated with sterile saline. Non-viable skin edges were trimmed. Laceration of the perionychium was repaired with 5-0 chromic suture in a simple interrupted fashion. The nail bed laceration was repaired with 6-0 chromic gut suture in a simple interrupted fashion. Bacitracin ointment was applied to the laceration repair. The nail was too fragmented to be used as a stent for the eponychial fold, so a portion of aluminum from the suture pack was used. The digit was dressed with xeroform, dry gauze, 4-prong cage splint, and cling wrap. Five days of Keflex were prescribed, given the mechanism of injury.
Follow Up:
The dressings remained occlusive for 48 hours. After this, the patient was told to gently clean with warm soapy water and perform daily dressing changes with bacitracin, xeroform, gauze, and kerlix. The patient was also allow the xeroform to soak to make it easier to remove. The cage splint was used for comfort with a tuft fracture. Arm elevation was encouraged to minimize pain and swelling –any swelling in the fingers causes a great increase in throbbing pain. Tylenol and ibuprofen was be used to pain control. Showers were allowed, but no submerging or soaking in water for two weeks. No lifting for over 10lbs for two weeks.
The patient was seen two weeks later in clinic. At the time, the digit was demonstrating appropriate healing. Recommended continuing bacitracin and dressings to protect from outside environment and cap splint for comfort. He was released to his manual job per his abilities.

Fig.3. Two week follow up
‘
He was seen once again one month after the initial visit. New nail growth was seen. There was minimal pain to the distal fingertip and the wound was healed. He was able to work without limitations. Discussed the growth cycles of the nail and that it would take about one year to fully know what the nail will look like.
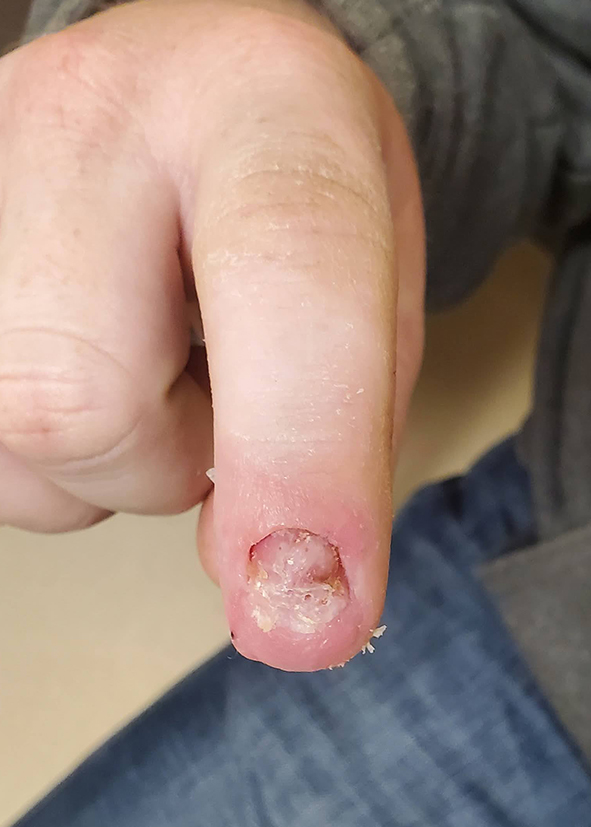
Fig.4. Six week follow up
–

