Abstract
Background:
The identification of different factors affecting anesthesia and physiological changes during anesthesia can be effective in improving the quality of anesthesia. Midazolam is a benzodiazepine that has been used for many years for sedation under anesthesia. Stress is also an important factor affecting memory and other physiological changes, such as blood pressure and heart rate.Objectives:
his study aimed to investigate the effects of stress on retrograde and anterograde amnesia among patients undergoing general anesthesia.Methods:
This multi-center, parallel, stratified, randomized controlled trial was performed on patients undergoing non-emergency abdominal laparotomy. The patients were divided into high- and low-stress groups according to the Amsterdam Preoperative Anxiety and Information Scale. Then, both groups were randomly divided into three subgroups receiving 0, 0.02, or 0.04 mg/kg of midazolam. Recall cards were shown to patients at 4 minutes, 2 minutes, and immediately before injection to determine retrograde amnesia and at 2 minutes, 4 minutes, and 6 minutes after injection to determine anterograde amnesia. Hemodynamic changes were recorded during intubation. The chi-square and multiple regression tests were used to analyze the data.Results:
Midazolam injection was associated with the development of anterograde amnesia in all groups (P < 0.05); however, it had no effect on the development of retrograde amnesia (P < 0.05). Midazolam could decrease the systolic and diastolic blood pressure and heart rate during intubation (P < 0.05). Stress also caused retrograde amnesia in patients (P < 0.05); nevertheless, it had no effect on anterograde amnesia (P > 0.05). Stress and midazolam injection could not affect the oxygen levels during intubation.Conclusions:
The results showed that midazolam injection could induce anterograde amnesia, hypotension, and heart rate; nonetheless, it had no effect on retrograde amnesia. Stress was associated with retrograde amnesia and increased heart rate; however, it was not associated with anterograde amnesia.Keywords
Retrograde Amnesia Anterograde Amnesia Midazolam Stress General Anesthesia
1. Background
Amnesia is one of the four basic components of balanced anesthesia, introduced by Lundy in 1962 (1, 2). The concept of amnesia was introduced in order to prevent psychological stimuli caused by intraoperative events during local anesthesia. Low doses of various anesthetic agents are used for this purpose; however, there is not yet a definite quantitative scale (3). Since the main goal of adequate depth of anesthesia is amnesia, it can be concluded that patients who are fully sedated should also have adequate amnesia around events during surgery.
Awareness is defined as the spontaneous recollection of events and is also known as explicit memory (4). Awareness under anesthesia occurs in 0.1 to 0.2% of patients, and these patients are able to recall events during surgery. This incident causes various problems, such as postoperative dissatisfaction and post-traumatic stress disorder (PTSD). If the consciousness is not suppressed enough, a clear memory of events might occur during general anesthesia (5, 6). An increasing body of evidence suggests that the choice of anesthetic drug can greatly affect the quality of anesthesia.
The body’s stress response to surgery was first noted in the 1920s when David Cuthbertson observed that operated patients had a large increase in postoperative metabolites. Since then, studies have examined the details of the stress response and its modification in favor of the patient. Choices of anesthesia can also have far-reaching implications for cancer cell biology and its progression to metastasis and invasion (7).
Since the introduction of midazolam (Versed) as an intravenous sedation drug, there have been numerous reports of its ability to produce amnesia. Amnesia occurs in two forms, including retrograde amnesia and anterograde amnesia. Anterograde amnesia is the failure to create new memories after an amnesia-inducing event, and retrograde amnesia refers to the loss of memory access to events before drug injection. Anterograde amnesia is an accepted pharmacological effect of several commonly used intravenous sedatives, in particular benzodiazepines, diazepam, and anticholinergic scopolamine (8).
Reports have shown that the duration of midazolam-induced anterograde amnesia might be longer than the duration induced by diazepam. This is usually considered helpful because it can induce a feeling of anesthesia (i.e., inability to remember what happened during an operation) without the additional risks of general anesthesia. The possibility of midazolam-induced retrograde amnesia has also been suggested in case reports and animal studies with possible mechanisms. This is usually considered helpful because it can induce a feeling of anesthesia (i.e., inability to remember what happened during an operation) without the additional risks of general anesthesia. However, limited studies of retrograde amnesia by midazolam have been reported (9).
2. Objectives
This study aimed to investigate the effects of stress on retrograde and anterograde amnesia among patients undergoing general anesthesia.
3. Methods
3.1. Trial Design and Population
This multi-center, three-arm, parallel design, blinded, stratified randomized controlled trial was conducted at FIROOZGAR and RASOUL AKRAM university hospitals in Tehran, Iran. Patients undergoing non-emergency abdominal laparotomy who received general anesthesia were screened for eligibility. The inclusion criteria included patients aged 20 - 60 years, American Society of Anesthesiologists classification I-II, and the expected duration of the operation less than 3 hours. The exclusion criteria were the presence of hepatic or renal impairment, visual or auditory impairment, psychiatric or mental disorders, prior use of benzodiazepines, receiving sedatives or antipsychotics, pregnancy, and refusal or inability to give informed consent. Psychiatric problems, severe learning disorders, and mental problems were examined in the preoperative visit, and suspected cases were excluded from the study.
3.2. Interventions
In this trial, the patients were stratified based on the results of the Amsterdam Preoperative Anxiety and Information Scale (APAIS) into high-stress and low-stress groups. The high-stress level was defined as preoperative APAIS above 13. Each stratum was designed to enroll 60 participants for a total of 120 patients in the trial.
The high-stress and low-stress were separately randomized with a 1:1:1 ratio to receive 0.02 or 0.04 mg/kg of midazolam or not receive midazolam for general anesthesia (i.e., the control group). The randomization sequence was generated centrally by a computer in permuted block sizes of three and six. All three study groups were injected with premedication, including fentanyl (3 µg/kg) and lidocaine (0.5 mg/kg). The patients underwent routine monitoring, including oxygen saturation (SpO2), blood pressure, electrocardiogram, and pulse rate monitoring. from the beginning of entry to the operation room. The study participants, the physician injecting the medications, and the outcome assessors were blinded to the randomized intervention.
3.3. Evaluation of Outcomes
The primary outcomes of the study were retrograde and anterograde amnesia. Three cards with photos of three types of fruits were used to check retrograde amnesia before drug injection, and three cards with photos of three types of animals were used to check anterograde amnesia after drug injection. For the evaluation of retrograde amnesia, three simple photo cards were shown at minutes of 0 (4 minutes before premedication injection), 2 (2 minutes before premedication injection), and 4 (immediately before premedication injection) over 30 seconds. At this stage, premedication was injected into three randomized groups by the above-mentioned method. Again, three more simple photo cards were shown to check anterograde amnesia in 6 (2 minutes after premedication injection), 8 (4 minutes after premedication injection), and 10 (6 minutes after premedication injection) minutes each time for 30 seconds. The patients were then injected with propofol (5.1 mg) and atracurium (0.5 mg/kg) 6 minutes after the premedication injection. Four minutes after induction, female and male patients were intubated with tubes number 7 and 7.5, respectively.
Secondary outcomes were hemodynamic measurements, including blood pressure, heart rate, and SpO2. These variables were recorded 1, 2, and 5 minutes after intubation. Intraoperative hemodynamic changes, intraoperative hemorrhage, and the need for intraoperative blood transfusion were recorded. All patients were explained about the cards before entering the operating room and remembering those 4 hours after leaving the recovery, and the information was recorded 4 hours after leaving the recovery.
3.4. Data Analysis
Descriptive statistics were used to report the variables. The chi-square test was used to evaluate the effect of stress and midazolam dose on amnesia. The multiple regression test was also used to evaluate the effect of stress and midazolam dose on hemodynamic changes. The data were entered into Excel and analyzed using Stata software (version 14.0).
3.5. Ethical Considerations and Trial Registration
Written consent was obtained from all participants. The data were anonymized, and personal information was kept confidential. This study was approved by the Research Council of the Faculty of Medicine, Iran University of Sciences and Medicine (ethics approval code: 98-3-4-16050) and complied with the Declaration of Helsinki. The protocol of this clinical trial has been registered in the Iranian Registry of Clinical Trials (IRCT20200213046484N1).
4. Results
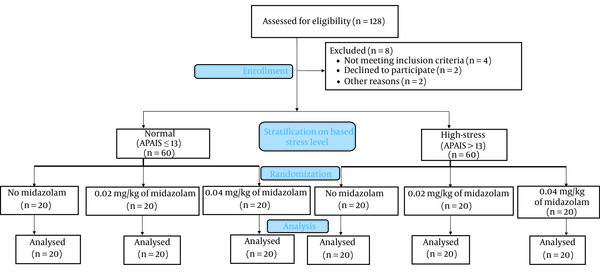
Within August 2020 to December 2021, a total of 62 male and 58 female subjects were included in this study, with mean age values of 48.19 and 48.37 years for males and females, respectively. In this study population, the participants had heart diseases (18 males and 11 females), followed by diabetes (7 males and 4 females) and other diseases (1 male and 2 females). Figure 1 illustrates the flow diagram of screening, enrollment, and randomization.
CONSORT flow diagram of screening, enrollment, and randomization. Abbreviation: APAIS, the Amsterdam Preoperative Anxiety, and Information Scale
4.1. Association of Preoperative Stress Level with Amnesia
According to the results of the chi-square test, stress had a significant relationship with retrograde amnesia in the first and second groups, and more stress indicated a lower chance of recalling the cards. However, in the third group, no significant relationship was observed. Table 1 shows the results of the chi-square test.
Effect of Stress on Retrograde Amnesia
| Card Recall | Stress Group | Yes | No | P-Value |
|---|---|---|---|---|
| 4 minutes before injection | Stressed | 53 | 7 | 0.006 |
| Low stress | 60 | 0 | ||
| 2 minutes before injection | Stressed | 52 | 8 | 0.003 |
| Low stress | 60 | 0 | ||
| Immediately before injection | Stressed | 53 | 7 | 0.083 |
| Low stress | 58 | 2 |
The data on recall cards after post-midazolam injection were used to evaluate the effect of stress on anterograde amnesia. According to the results of the chi-square test, stress was not significantly associated with anterograde amnesia in any group, which is shown in Table 2.
Effect of Stress on Anterograde Amnesia
| Card Recall | Stress Group | Yes | No | P-Value |
|---|---|---|---|---|
| 2 minutes after injection | Stressed | 19 | 0.699 | 41 |
| Low stress | 21 | 39 | ||
| 4 minutes after injection | Stressed | 17 | 0.69 | 43 |
| Low stress | 19 | 41 | ||
| 6 minutes after injection | Stressed | 17 | 0.69 | 43 |
| Low stress | 19 | 41 |
4.2. Effect of Midazolam on Amnesia
The data on different doses of midazolam were compared to controls that did not receive any doses of midazolam. According to the results of this test, no significant relationship was observed between different doses of midazolam and retrograde amnesia in any of the groups. The results of this comparison can be observed in Table 3. Although no significant relationship was observed between different doses of midazolam and retrograde amnesia, two patients in the low-stress group could not remember the cards before the midazolam injection. In the study of recall of preoperative events, this amnesia was also evident, which is worth reporting on a case-by-case basis.
Effect of Different Doses of Midazolam on Retrograde Amnesia
| Dose of Midazolam | Card Recall | Groups | Yes | No | P-Value |
|---|---|---|---|---|---|
| Dose 0.02 mg/kg | 4 minutes before injection | Control | 38 | 2 | 1.0 |
| Intervention | 38 | 2 | |||
| 2 minutes before injection | Control | 37 | 3 | 1.0 | |
| Intervention | 37 | 3 | |||
| Immediately before injection | Control | 37 | 3 | 1.0 | |
| Intervention | 37 | 3 | |||
| Dose 0.04 mg/kg | 4 minutes before injection | Control | 38 | 2 | 0.64 |
| Intervention | 37 | 3 | |||
| 2 minutes before injection | Control | 37 | 3 | 0.64 | |
| Intervention | 38 | 2 | |||
| Immediately before injection | Control | 37 | 3 | 1.0 | |
| Intervention | 37 | 3 |
According to the results of the chi-square test, a significant relationship was observed between different doses of midazolam and card recall in all groups, and midazolam injection increased the likelihood of anterograde amnesia in these patients. Table 4 shows the results of the chi-square test.
Effect of Different Doses of Midazolam on Anterograde Amnesia
| Dose of Midazolam | Card Recall | Groups | Yes | No | P-Value |
|---|---|---|---|---|---|
| Dose 0.02 mg/kg | 2 minutes after injection | Control | 37 | 3 | 0.0001 |
| Intervention | 3 | 37 | |||
| 4 minutes after injection | Control | 36 | 4 | 0.0001 | |
| Intervention | 0 | 40 | |||
| 6 minutes after injection | Control | 36 | 4 | 0.0001 | |
| Intervention | 0 | 40 | |||
| Dose 0.04 mg/kg | 2 minutes after injection | Control | 37 | 3 | 0.0001 |
| Intervention | 0 | 40 | |||
| 4 minutes after injection | Control | 36 | 4 | 0.0001 | |
| Intervention | 0 | 40 | |||
| 6 minutes after injection | Control | 36 | 4 | 0.0001 | |
| Intervention | 0 | 40 |
4.3. Secondary Outcomes
For the evaluation of the effect of stress on hemodynamic changes, this study used data on changes in systolic and diastolic blood pressure, heart rate, oxygen level, midazolam intake, and stress based on the APAIS score. According to the results of this test, changes in systolic blood pressure were significantly associated with midazolam injection (P = 0.0001); however, the changes were not significantly associated with stress. Each 0.01 unit increase in midazolam intake decreased systolic blood pressure by 1.14 units.
Stress also increased systolic blood pressure by 0.5 units, which was not observed to be statistically significant. The effect of stress and midazolam on diastolic blood pressure was similar to systolic blood pressure, and the decrease in diastolic blood pressure was significantly associated with midazolam injection (P = 0.0001); however, no significant difference was observed in terms of stress. Each 0.01 unit increase in midazolam intake decreased diastolic blood pressure by 1.2 units. In addition, having stress increased diastolic blood pressure by 0.9 units, with no significant difference.
There was a significant relationship between stress and increased heart rate. Being stressed increases heart rate by 2.51 units. There was a significant relationship between midazolam intake and heart rate decrease; accordingly, every 0.01 unit increase in midazolam intake caused a decrease of 0.87 units in heart rate. Unlike other comparisons, no significant relationship was observed between stress and midazolam intake and changes in oxygen levels.
5. Discussion
In addition to trauma and stress-related disorders, stressful experiences can cause a range of mental illnesses known as dissociative disorders. These disorders are thought to be related to disturbances in the normal functioning of consciousness, such as memory, perception, and identity awareness, through stressful experiences. These disorders have a prevalence of about 10% of the total population (10).
In addition, the symptoms of dissociative disorders are similar to most psychiatric disorders, including PTSD and schizophrenia (11). These symptoms, which are often debilitating, include partial or complete forgetfulness, anxiety, depression, suicide, and severely compromised social functioning. At a fundamental level, dissociative amnesia is thought to be rooted in state-dependent learning, in which memories formed under a particular emotional state, stress, or drugs are better recovered under similar circumstances (12). Based on the data presented in the present study, stress had a significant effect on retrograde amnesia. Individuals in the high-stress group remembered fewer cards than those in the low-stress group. However, stress did not have a significant effect on anterograde amnesia. Although stressed individuals recalled fewer cards in all groups, this difference was not significant according to the chi-square test.
The first theoretical reports of such memory impairment show that stressful condition prevents the proper integration of unpleasant and normal experiences and causes a state of disruption. Importantly, amnesia was also observed to reflect only the inability to recall memories, not to encode memories (13).
Patients also recall these types of memories when they are in a similar physiological or traumatic situation; however, they have not been able to recall them before. This phenomenon indicates a different mechanism that is situation-dependent (14). Therefore, it can be concluded that individuals who were not able to remember the cards in this study due to high stress might be able to recall the card memories if they are in this situation again, for example, returning to the hospital for surgery. A literature review shows that patients with retrograde amnesia, under the influence of high stress, lose access to memories of past events. Patients with anterograde amnesia cannot recall very emotional experiences.
If anterograde amnesia is experienced repeatedly in daily life, something in everyday life becomes a trigger for fear. Fear conditioning in amnesia is often related to memories of child abuse that are not recallable due to dissociative forgetfulness (15). Although there is ample evidence for the effect of stress on anterograde amnesia, there are no robust studies on preoperative stress and anterograde amnesia. Most of the population studied in the studies were mentally ill and highly stressed individuals; therefore, comparing the findings of those studies with the results of the present study is not logical.
The findings of the present study revealed that midazolam injection had no association with retrograde amnesia in either group. However, midazolam injection caused anterograde amnesia in the subjects of this study, and a significant difference was observed between midazolam injection and card recall in all groups. These results are consistent with the results of other studies that have been conducted on this subject. In a study by Yakubu 80 patients were scheduled for no major elective surgical procedures under general anesthesia and divided into four groups, including 2, 5, and 7 mg midazolam or normal saline. Patients receiving midazolam showed a significant difference in card recall after injecting midazolam (anterograde amnesia), compared to the control group. No significant relationship was observed between retrograde amnesia and midazolam injection in these patients (8).
Another study conducted by Gupta et al. in 2017 examined 80 patients who were candidates for face and neck surgery. The patients were divided into two groups, in which group 1 received 0.02 mg/kg and group 2 received 0.06 mg/kg midazolam intravenously as premedication. Recall of events was significantly lower in group 2 than in group 1 (anterograde amnesia), and no difference was observed in the pre-injection recall of events (retrograde amnesia) (16).
In a clinical trial performed by Bulach et al. on 40 candidates undergoing surgery and general anesthesia, patients were divided into four groups, including midazolam 2, 5, and 10 mg or control. Recognition and recall rates were observed to be similar between groups until the drug administration, where no evidence of retrograde amnesia was observed. However, the recall rates after injection in all three groups receiving midazolam were significantly observed to be lower than in the control group. Furthermore, patients who received higher doses of midazolam had lower card recall rates (17), which is consistent with the results of the present study. However, a study reported the development of retrograde amnesia after midazolam injection. This study was a case report and reported its occurrence only in two patients. Except in this case, the available evidence suggests that midazolam injection could not induce retrograde amnesia (18).
According to the results of this study, midazolam injection was significantly associated with a decrease in systolic and diastolic blood pressure and a decrease in heart rate. Being stressed was only significantly associated with increased heart rate. Oxygen levels (SpO2) were not significantly associated with midazolam injection and stress. In a similar study, consistent with the results of this study, midazolam injection could reduce diastolic blood pressure but had no effect on other variables, including oxygen levels (16).
Another study showed that midazolam significantly reduced heart rate and blood pressure (19). Two different studies reported different effects of midazolam on oxygen levels. Although one study reported a significant effect of midazolam on oxygen depletion 10 minutes after injection (20), another study did not report a significant difference, similar to the results of this study, between the midazolam-receiving group and the control group (21). Another study demonstrated that patients who experienced more stress before surgery had higher heart rates during surgery (22). Another study on the effects of stress and anxiety on patients undergoing surgery showed that having a higher stress score was associated with increased heart rate (23).
5.1. Conclusions
This trial showed that midazolam had a significant relationship with anterograde amnesia; nevertheless, no significant effect of midazolam injection was observed regarding retrograde amnesia. Midazolam injection was noticed to be associated with lower blood pressure and heart rate. Stress had a significant relationship with retrograde amnesia; however, no significant association was observed between stress and anterograde amnesia. Stress was also associated with increased heart rate during intubation. Moreover, stress and midazolam injection was not significantly associated with changes in oxygen levels during intubation.
References
-
1.
Lundy JS. Balanced anaesthesia. Minn Med. 1926;9:399.
-
2.
Shim JH. Multimodal analgesia or balanced analgesia: the better choice? Korean J Anesthesiol. 2020;73(5):361-2. [PubMed ID: 32951409]. [PubMed Central ID: PMC7533177]. https://doi.org/10.4097/kja.20505.
-
3.
Sanders RD, Tononi G, Laureys S, Sleigh JW. Unresponsiveness not equal unconsciousness. Anesthesiology. 2012;116(4):946-59. [PubMed ID: 22314293]. [PubMed Central ID: PMC3311716]. https://doi.org/10.1097/ALN.0b013e318249d0a7.
-
4.
Sultana A. Anthony Absalom and Keira Mason (eds), Total intravenous anesthesia and target controlled infusions: A comprehensive global anthology, 1st ed., Springer: Basel, Switzerland, 2017; 827 pp.: ISBN 9783319476070 (hbk), ISBN 9783319476094 (ebook). Anaesth Intensive Care. 2019;47(5):483-4. https://doi.org/10.1177/0310057x19873002.
-
5.
Tasbihgou SR, Vogels MF, Absalom AR. Accidental awareness during general anaesthesia - a narrative review. Anaesthesia. 2018;73(1):112-22. [PubMed ID: 29210043]. https://doi.org/10.1111/anae.14124.
-
6.
Pandit JJ. Acceptably aware during general anaesthesia: 'dysanaesthesia'--the uncoupling of perception from sensory inputs. Conscious Cogn. 2014;27:194-212. [PubMed ID: 24927512]. https://doi.org/10.1016/j.concog.2014.05.007.
-
7.
Wilmore DW. From Cuthbertson to fast-track surgery: 70 years of progress in reducing stress in surgical patients. Ann Surg. 2002;236(5):643-8. [PubMed ID: 12409671]. [PubMed Central ID: PMC1422623]. https://doi.org/10.1097/00000658-200211000-00015.
-
8.
Yakubu S. Does midazolam produce retrograde amnesia in surgical patients? Arch Int Surg. 2017;7(1):7-12. https://doi.org/10.4103/ais.ais_6_17.
-
9.
Rinehart JB, Baker B, Raphael D. Postoperative global amnesia reversed with flumazenil. Neurologist. 2012;18(4):216-8. [PubMed ID: 22735251]. https://doi.org/10.1097/NRL.0b013e31825bbef4.
-
10.
Sar V. Developmental trauma, complex PTSD, and the current proposal of DSM-5. Eur J Psychotraumatol. 2011;2. [PubMed ID: 22893823]. [PubMed Central ID: PMC3402152]. https://doi.org/10.3402/ejpt.v2i0.5622.
-
11.
Lanius RA, Vermetten E, Loewenstein RJ, Brand B, Schmahl C, Bremner JD, et al. Emotion modulation in PTSD: Clinical and neurobiological evidence for a dissociative subtype. Am J Psychiatry. 2010;167(6):640-7. [PubMed ID: 20360318]. [PubMed Central ID: PMC3226703]. https://doi.org/10.1176/appi.ajp.2009.09081168.
-
12.
Krammer S, Kleim B, Simmen-Janevska K, Maercker A. Childhood trauma and complex posttraumatic stress disorder symptoms in older adults: A study of direct effects and social-interpersonal factors as potential mediators. J Trauma Dissociation. 2016;17(5):593-607. [PubMed ID: 26011396]. https://doi.org/10.1080/15299732.2014.991861.
-
13.
Breuer J, Freud S. Studies on hysteria. Hachette: The New York Times; 2009.
-
14.
Schmidt GN, Muller J, Bischoff P. [Measurement of the depth of anaesthesia]. Anaesthesist. 2008;57(1):9-30. 32-6. [PubMed ID: 18209969]. https://doi.org/10.1007/s00101-007-1294-6.
-
15.
Yoshimasu H, Yasuda T, Kurihara A. Psychogenic retrograde and anterograde amnesia. Brain Nerve. 2018;70(7):803-12.
-
16.
Gupta R, Santha N, Upadya M, Manissery JJ. Effect of Different Dosages of Intravenous Midazolam Premedication on Patients Undergoing Head and Neck Surgeries- A Double Blinded Randomized Controlled Study. J Clin Diagn Res. 2017;11(8):UC01-4. [PubMed ID: 28969245]. [PubMed Central ID: PMC5620886]. https://doi.org/10.7860/JCDR/2017/26414.10381.
-
17.
Bulach R, Myles PS, Russnak M. Double-blind randomized controlled trial to determine extent of amnesia with midazolam given immediately before general anaesthesia. Br J Anaesth. 2005;94(3):300-5. [PubMed ID: 15567810]. https://doi.org/10.1093/bja/aei040.
-
18.
Aulakh G, Shokouhi B, Beneng K. Retrograde amnesia after intravenous sedation and general anaesthesia in a dental hospital. Br J Oral Maxillofac Surg. 2018;56(7):632-5. [PubMed ID: 30029983]. https://doi.org/10.1016/j.bjoms.2018.06.017.
-
19.
Sultan S, Hegazy N. Utilizing heart rate variability: Midazolam prevents the sympathovagal imbalance caused by fentanyl/propofol induction. Ain Shams J Anesthesiol. 2015;8(1):31. https://doi.org/10.4103/1687-7934.153935.
-
20.
Roelofse JA, van der Bijl P, Joubert JJ, Breytenbach HS. Blood oxygen saturation levels during conscious sedation with midazolam. A report of 16 cases. S Afr Med J. 1986;70(13):801-2. [PubMed ID: 3798264].
-
21.
Rodrigo MR, Rosenquist JB. Effect of conscious sedation with midazolam on oxygen saturation. J Oral Maxillofac Surg. 1988;46(9):746-50. [PubMed ID: 3166044]. https://doi.org/10.1016/0278-2391(88)90184-x.
-
22.
Huiku M, Uutela K, van Gils M, Korhonen I, Kymalainen M, Merilainen P, et al. Assessment of surgical stress during general anaesthesia. Br J Anaesth. 2007;98(4):447-55. [PubMed ID: 17329347]. https://doi.org/10.1093/bja/aem004.
-
23.
Wetsch WA, Pircher I, Lederer W, Kinzl JF, Traweger C, Heinz-Erian P, et al. Preoperative stress and anxiety in day-care patients and inpatients undergoing fast-track surgery. Br J Anaesth. 2009;103(2):199-205. [PubMed ID: 19483203]. https://doi.org/10.1093/bja/aep136.