Are My Joints Hypermobile?
Can you straighten your elbow past neutral? Can it hyperextend?
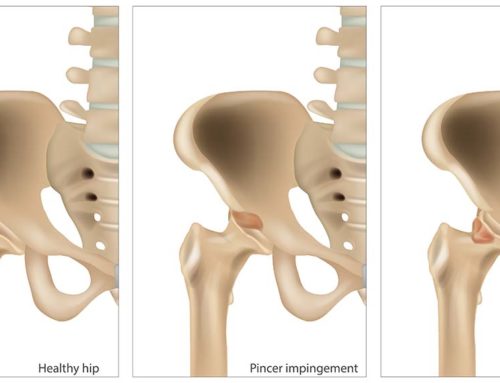
Some people have more laxity in their joint structures and can move their joints quite far. Contrary to popular belief, they are not double-jointed. There is no such thing. They just have more laxity or “looseness” in their joints so they can move them to a greater range. It’s not necessarily good or bad. It’s just their genes that have predisposed them to that type of joint integrity. That being said, there are examples of where laxity or hypermobility can occur in a single joint, but this is a different situation. This is usually attributed to a previous injury. A common example of this is a shoulder dislocation. After a joint dislocation, the stabilizing structures (ligaments) are damaged. The joint is then unstable and can be prone to another dislocation. For the purpose of this blog, we’re going to focus on generalized hypermobility conditions.
Joint Hypermobility
Joint hypermobility is not a diagnosis. It’s a clinical finding that a practitioner needs to detect and then make sense of. Is the hypermobility related to a previous injury? Is it generally occurring in many different joints? Is it relevant to this patient’s overall pain and function? Although it’s common for surrounding muscles to tighten around a hypermobile joint (which can lead to pain), joint hypermobility isn’t inherently painful. In my experience, in most cases, it isn’t too clinically relevant. In other words, it is good to detect it but it doesn’t usually have a large bearing on the recommendations for treatment. For most patients, generalized joint hypermobility does not affect the prognosis.
As mentioned above, generalized joint hypermobility can be entirely normal and is not necessarily good or bad. However, although relatively rare, it can be part of a larger diagnostic picture for some individuals. It can be linked to some general connective tissue disorders. Hypermobile Ehlers-Danlos Syndrome (hEDS) or the more general term hypermobility spectrum disorder (HSD) are recognized conditions in which a person’s connective tissues are different. Both of these conditions have a collection of signs and symptoms that are characteristic for the diagnosis. They can involve different body systems and aren’t just related to the musculoskeletal system. As mentioned above, generalized joint laxity can be a clue to the bigger picture. Fatigue, dysautonomia and co-ordination deficits are common with both hEDS and HSD. Dysautonomia is an umbrella term that is related to the autonomic nervous system. An easy way to think of it is dysfunction in many of the automatic things our body does for us. Examples include heart rate, digestion, vision and temperature regulation. Kids may experience fatigue, gastrointestinal symptoms and poor co-ordination. Adults more typically experience musculoskeletal pain, sleep dysfunction and urogenital symptoms. Obviously, given the difficulty with the musculoskeletal system, pain can be exacerbated with too much activity or too much rest. Other common characteristics are postural orthostatic tachycardia (POTS) and mast cell activation syndrome (MCAS). Mast cell activation syndrome relates to an abnormal immune response and is related to dysfunction in many different systems, such as our cardiovascular, dermatological, gastrointestinal, neurological and respiratory systems. As mentioned above with dysautonomia, POTS refers to the difficulty of some of our automatic bodily functions. In this case, it specifically refers to difficulty related to heart rate and blood pressure when changing from lying to standing.
Identifying Abnormal Joint Mobility
So how is this relevant to our clinic and why are we posting a blog on it? In health care, there are experts in different areas. Cardiologists know hearts, dentists know teeth and optometrists know the eyes. Chiropractors and physiotherapists are experts in the musculoskeletal system and joints. We can identify those with abnormal joint mobility and can help detect one part of the elaborate puzzle in these relatively rare connective tissue disorders. We are not experts in the other bodily systems involved in hypermobile ehlers-danlos syndrome (hEDS) or hypermobility spectrum disorder (HSD). For example, consider a hypothetical patient who presents to a clinic like Burlington Sports Therapy. Following their examination, we have identified that they have generalized joint hypermobility. We have learned from their history that they have a rather complex and long history of pain and dysfunction and they have been to many different practitioners over the years. In this case, perhaps nobody has considered looking at the bigger picture. Perhaps there is a general connective tissue disorder and this is why they have persistent pain and many different health conditions affecting various systems within the body. Relevant questions would include…
- Do any family members or relatives have a connective tissue disorder?
- Have you had any hernias or prolapsed organs?
- Have you ever dislocated any joints?
- Is your skin “stretchy”?
- Have you been diagnosed with any conditions relating to your cardiovascular system, such as mitral valve prolapse or aortic dilatation?
- Do you have unexplained stretch marks or small bumps in the skin of your heel visible on weight-bearing?
- Do you regularly feel tired?
Keep in mind that these connective tissue disorders are relatively rare. It’s important to always consider the bigger picture with our health and sometimes diagnosing a rare condition requires a keen eye to all the small pieces of the puzzle. Chiropractors and physiotherapists are experts in the musculoskeletal system. If you’re injured, in pain or have questions about whether your joints are “normal” please don’t hesitate to give us a call, we can help!
References
Russek LN, Stott P & Simmonds J. Recognizing and Effectively Managing Hypermobility-related Conditions. Physical Therapy 2019; 99: 1189–1200.
Palmer S, Terry R, Rimes KA, Clark C, Simmonds J, Horwood J. Physiotherapy management of joint hypermobility syndrome: a focus group study of patient and health professional perspectives. Physiotherapy 2016; 102: 93–102.