.webp)
Causes
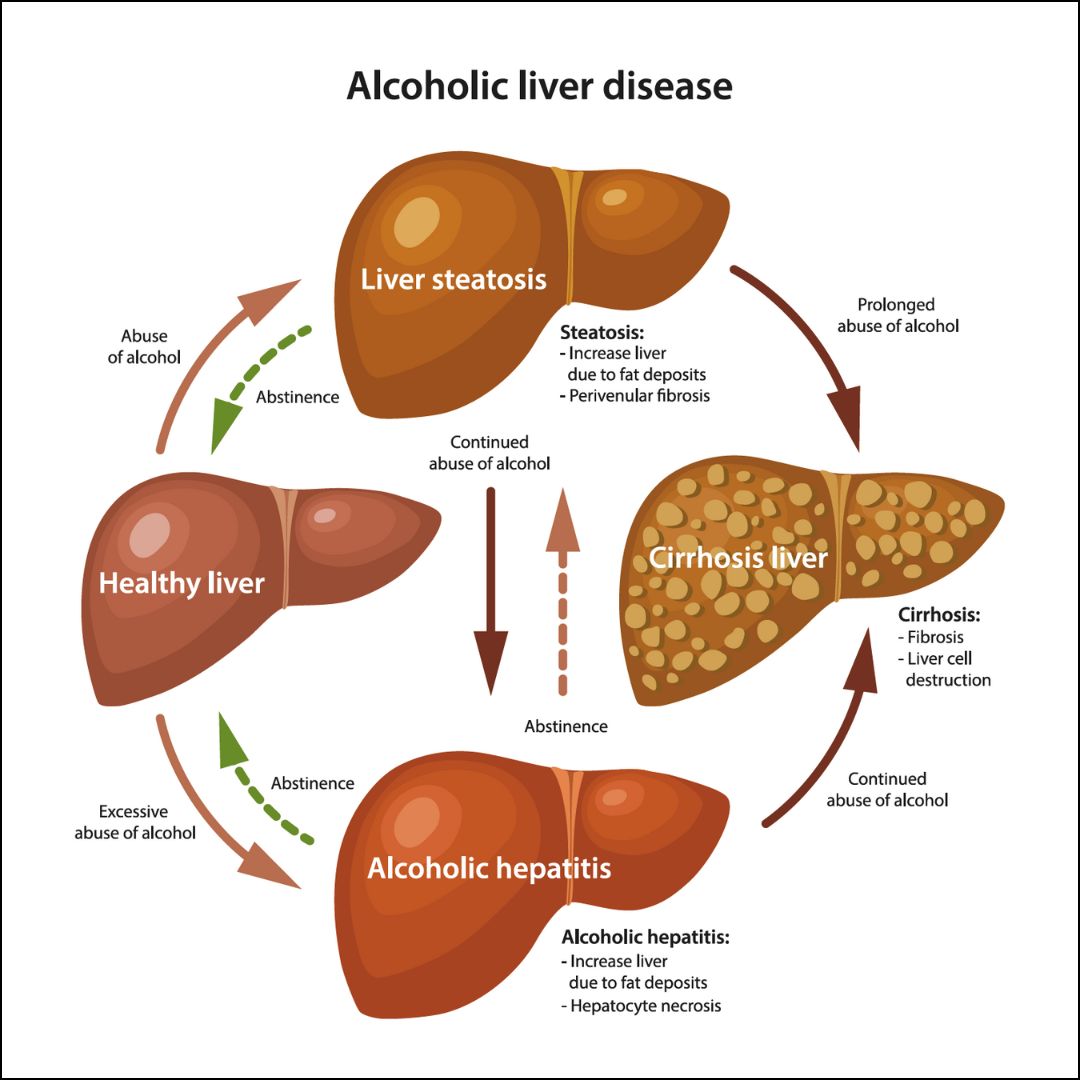
The primary cause of alcoholic liver disease is, alcohol abuse. When consumed in excess, alcohol can have detrimental effects on the liver, which is responsible for filtering toxins from our bloodstream. Over time, excessive alcohol intake can lead to inflammation and scarring of the liver tissue, impairing its ability to function properly. It's worth noting that not everyone who consumes alcohol excessively will develop alcoholic liver disease. Factors such as genetic predisposition, overall health status, and even gender can play a role in determining an individual's susceptibility to this condition. Also, it's important to recognize that the quantity and frequency of alcohol consumption are significant factors contributing to alcoholic liver disease. Heavy drinking over an extended period poses a greater risk than occasional or moderate drinking. Other lifestyle factors such as poor nutrition and obesity can also contribute to the development and progression of alcoholic liver disease. These factors exacerbate the damage caused by alcohol consumption and further strain an already compromised liver.
Risk Factors
One of the primary risk factors for alcoholic liver disease is the quantity and duration of alcohol consumption. Heavy, long-term drinking significantly increases the likelihood of developing this condition. Additionally, gender plays a role, as women tend to be more susceptible to alcohol-related liver damage than men due to differences in metabolism and body composition. Genetics also play a significant role in determining an individual's vulnerability to alcoholic liver disease. Certain genetic variations can make some people more prone to developing liver damage even with lower levels of alcohol consumption. Other contributing factors include poor nutrition, specifically deficiencies in vitamins such as folate and vitamin B complex, as well as obesity and co-existing conditions such as hepatitis C infection. These factors can compound the negative impact of alcohol on the liver, accelerating disease progression. Recognizing these risk factors empowers individuals to make informed decisions about their alcohol consumption habits and seek appropriate medical guidance if needed. It also highlights the importance of public health initiatives aimed at raising awareness about responsible drinking practices and providing support for those struggling with alcohol misuse.
Symptoms
One of the most common symptoms of Alcoholic Liver Disease is abdominal pain and tenderness. This discomfort may be accompanied by swelling or bloating in the abdominal area. Fatigue and weakness are also prevalent symptoms, as the liver's ability to function properly becomes compromised. Another indicator of Alcoholic Liver Disease is jaundice, which presents as yellowing of the skin and eyes. This occurs when the liver fails to effectively process bilirubin, resulting in its accumulation in the body. Individuals with Alcoholic Liver Disease may experience unexplained weight loss due to a decrease in appetite or malnutrition caused by alcohol's interference with nutrient absorption. Additionally, nausea and vomiting are often reported. In more advanced stages of Alcoholic Liver Disease, individuals may exhibit signs of cognitive impairment such as confusion or difficulty concentrating. Swelling in the legs and ankles can occur due to fluid retention caused by liver dysfunction. It is important to note that these symptoms can vary in severity depending on the stage of Alcoholic Liver Disease and individual factors such as overall health and alcohol consumption patterns. If you or someone you know is experiencing any combination of these symptoms, it is crucial to seek medical attention promptly for proper diagnosis and treatment options.
Diagnosis
One of the primary diagnostic tools used is a comprehensive medical history and physical examination. The healthcare provider will inquire about the patient's alcohol consumption patterns, duration, and any associated symptoms. They will also conduct a thorough physical examination to check for signs of liver damage such as jaundice, enlarged liver, or abdominal tenderness. Laboratory tests play a vital role in diagnosing alcoholic liver disease. Blood tests are conducted to evaluate liver function by measuring levels of enzymes such as alanine aminotransferase (ALT) and aspartate aminotransferase (AST). Elevated levels of these enzymes indicate liver damage. Imaging studies like ultrasound, computed tomography (CT) scan, or magnetic resonance imaging (MRI) may be performed to visualize the liver's structure and detect any abnormalities or signs of cirrhosis. In some cases, a liver biopsy may be recommended to confirm the diagnosis. This procedure involves removing a small sample of liver tissue for microscopic examination. It provides valuable information about the extent of liver damage and helps determine appropriate treatment options. Early diagnosis of alcoholic liver disease is crucial in preventing further complications and improving patient outcomes. Therefore, if you experience symptoms related to alcohol abuse or have concerns about your alcohol consumption, it is important to seek medical attention promptly for proper diagnosis and guidance on managing this condition effectively.
Treatments
One of the key elements in treating alcoholic liver disease is achieving and maintaining sobriety. This often involves a combination of behavioral therapy, counseling, support groups, and sometimes even medications to help manage cravings and withdrawal symptoms. It's essential for individuals with this condition to seek professional help and guidance throughout their journey towards recovery. In addition to addressing alcohol addiction, medical interventions are often necessary to manage the various complications associated with alcoholic liver disease. Medications may be prescribed to reduce inflammation in the liver, improve liver function, or prevent further damage. In some cases, surgical interventions such as a liver transplant may be considered for individuals with advanced stages of the disease. Also, adopting a healthy lifestyle plays a significant role in supporting liver health and aiding in the recovery process. This includes following a well-balanced diet that is low in fat and sodium while being rich in fruits, vegetables, whole grains, and lean proteins. Regular exercise can also contribute positively by improving overall cardiovascular health and reducing excess weight. It is important for individuals diagnosed with alcoholic liver disease to work closely with healthcare professionals who specialize in hepatology or gastroenterology. These specialists can provide personalized treatment plans tailored to each individual's specific needs.
Preventive Measures
One of the most important steps in prevention is to limit alcohol consumption. It is essential to follow recommended guidelines for moderate drinking or, in some cases, abstain from alcohol altogether. This means no more than one drink per day for women and two drinks per day for men. Maintaining a healthy diet is also crucial in preventing alcoholic liver disease. Consuming a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help support liver health and reduce the risk of damage caused by excessive alcohol intake. Regular exercise plays a vital role as well. Engaging in physical activity not only helps maintain a healthy weight but also promotes liver function by improving blood flow and reducing inflammation. Additionally, seeking professional help for alcohol addiction or dependence is essential for prevention. Support groups, counseling services, and treatment programs can provide the necessary tools and guidance to overcome alcohol abuse and prevent further damage to the liver.
Do's & Don’t's
When it comes to managing alcoholic liver disease, knowing the do's and don'ts is crucial for a successful treatment journey. By following the right guidelines, individuals can take control of their health and improve their overall well-being.
| Do's | Don't |
| Seek medical help and follow the prescribed treatment plan. | Don't ignore symptoms or delay seeking medical advice. |
| Abstain from alcohol completely. | Don't continue to consume alcohol. Even small amounts can worsen the condition. |
| Follow a balanced and healthy diet rich in fruits, vegetables, and whole grains. | Don't consume high-fat, processed, or fried foods that can aggravate liver damage. |
| Stay hydrated by drinking plenty of water. | Don't consume excessive amounts of sugary or caffeinated beverages. |
| Engage in regular physical activity as advised by your healthcare provider. | Don't lead a sedentary lifestyle. Regular exercise can improve overall health. |
| Take prescribed medications and supplements as directed by your doctor. | Don't take over-the-counter medications or supplements without consulting your healthcare provider. Some substances can harm the liver. |
| Get vaccinated against hepatitis A and B to protect your liver. | Don't neglect vaccination or other preventive measures against liver infections. |
| Follow up with regular check-ups and screenings as recommended by your healthcare provider. | Don't skip medical appointments or ignore recommended tests. Early detection can be crucial. |
| Manage stress through relaxation techniques or counseling if necessary. | Don't neglect mental health. Stress can worsen the condition. Seek support if needed. |
| Educate yourself about alcoholic liver disease and its management. | Don't rely on unreliable sources for information or ignore the importance of understanding your condition. |
If you suspect you or someone else is experiencing Alcoholic Liver Disease, it is crucial to seek immediate medical attention by calling emergency services or consult with a Gastroenterologist.


 040 6700 0000
040 6700 0000  040 6700 0111
040 6700 0111