Causes
The exact cause of brief psychotic disorder is unknown. However, it often appears after major stressors or traumatic events such as death of a loved one, natural disasters, or physical trauma. These events can lead to a heightened state of emotional turmoil or stress, which might trigger the onset of psychotic symptoms.
Risk Factors
Understanding risk factors is crucial, as it helps in early identification and management of potential cases. The risk factors for brief psychotic disorder can be multifaceted and include both internal and external influences. While the presence of risk factors does not guarantee the development of the disorder, they do increase the likelihood. Here's a more detailed look:
1. Previous Traumatic Events:
• Description: Experiencing a traumatic event can act as a trigger for brief psychotic disorder. This can include events such as physical assault, witnessing violence, or experiencing a significant natural disaster.
• Mechanism: Traumatic events can lead to heightened emotional and psychological stress, potentially overwhelming the individual's coping mechanisms and leading to the onset of psychotic symptoms.
2. Family History: •
Description: Having close family members (such as parents or siblings) with a history of psychotic or mood disorders might increase the risk of developing brief psychotic disorder.
• Mechanism: Genetic predispositions combined with environmental factors might enhance vulnerability to the disorder.
3. Personality Disorders:
• Description: Individuals diagnosed with certain personality disorders, particularly borderline or dependent personality disorders, may be at a higher risk.
• Mechanism: The emotional instability and interpersonal challenges associated with some personality disorders might make these individuals more susceptible to stress-induced psychological disruptions.
4. Major Life Stressors:
• Description: Events like losing a job, sudden financial troubles, divorce, or the death of a loved one can act as catalysts.
• Mechanism: These situations can produce intense emotional turmoil or stress, potentially acting as triggers for brief psychotic episodes. 5. Postpartum Period:
• Description: Some women might experience brief psychotic disorder shortly after giving birth.
• Mechanism: Hormonal changes, combined with the stress and possible trauma of childbirth, might contribute to the onset in predisposed individuals.
6. Substance Abuse:
• Description: Even though substance-induced psychosis is a separate condition, abuse of drugs or alcohol can be a risk factor for brief psychotic disorder.
• Mechanism: Substances might amplify underlying vulnerabilities or act as triggers, especially during withdrawal or when used in large amounts.
7. Travel or Migration:
• Description: Immigrants or individuals who have recently relocated might be at increased risk, particularly if the move was stressful or traumatic.
• Mechanism: The stress of adapting to a new environment, combined with potential isolation or cultural dislocation, might contribute to onset.
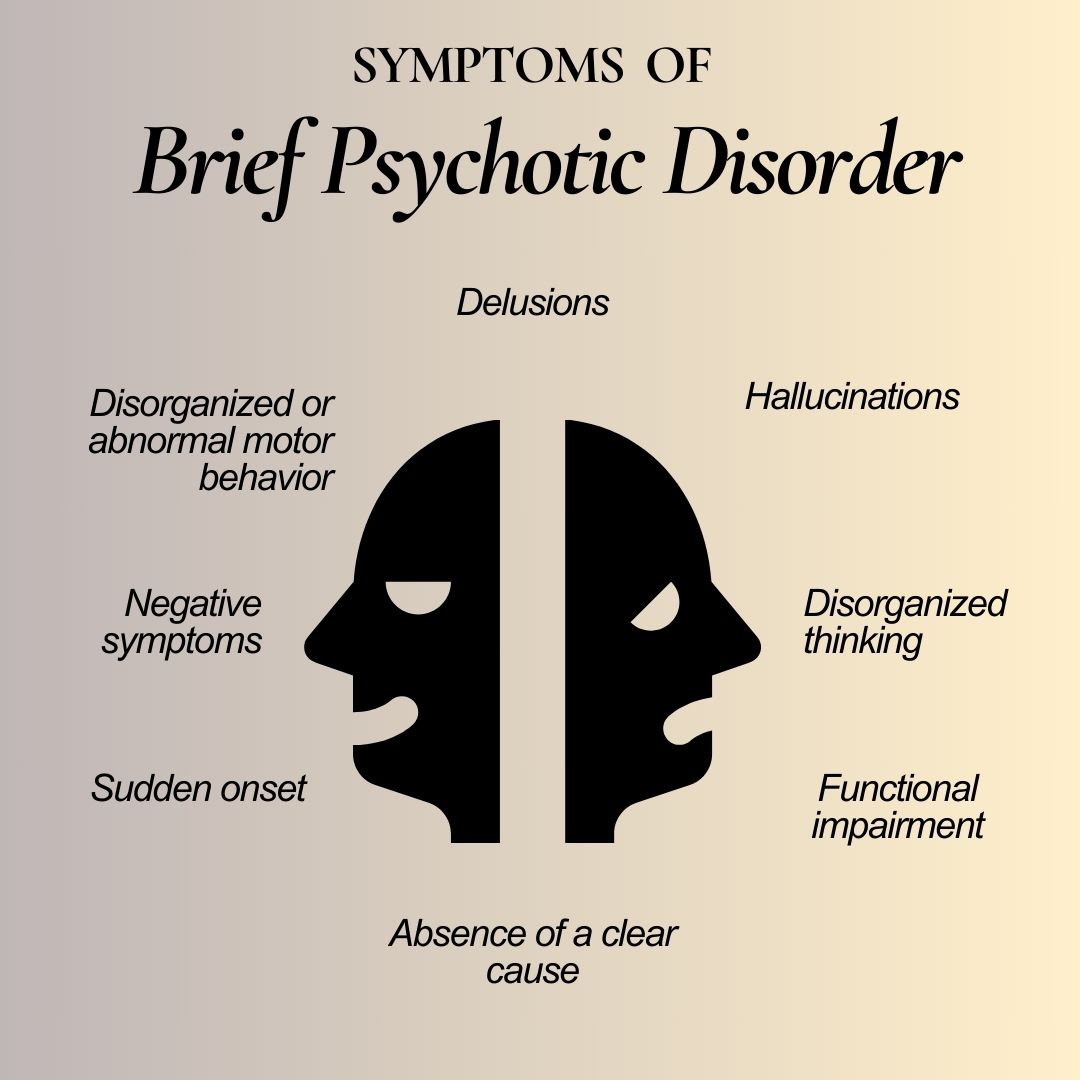
Symptoms
Common symptoms include:
• Hallucinations: Perceiving things (like hearing voices) that aren’t there.
• Delusions: Strong false beliefs.
• Disorganized Speech: Incoherent or nonsensical talk.
• Disorganized Behaviour: Acting inappropriately or unpredictably.
• Catatonic Behaviour: Lack of movement or speech.
Diagnosis
Accurately diagnosing brief psychotic disorder is vital for providing the right treatment and care. Since the symptoms are transient and can overlap with other conditions, the diagnostic process involves a thorough evaluation. Here’s a deeper dive into the diagnostic steps:
1. Clinical Interview:
• Description: This is often the first step. A mental health professional will gather a comprehensive history, including the onset and duration of symptoms, any preceding events or triggers, and any family history of mental illness.
• Purpose: To obtain a clear picture of the individual's mental state, life circumstances, and any potential stressors or triggers that might have contributed to the onset of symptoms.
2. Physical Exam:
• Description: This involves a standard medical examination to assess the individual's overall health.
• Purpose: To rule out any medical conditions or issues that might be causing or contributing to the symptoms. Some medical illnesses can manifest with psychotic-like symptoms.
3. Laboratory Tests:
• Description: These can include blood tests, urine tests, or other relevant lab investigations.
• Purpose: To check for substances or medical conditions that might induce psychotic symptoms. For instance, a thyroid function test might be ordered to rule out thyroid disorders, which can sometimes present with psychiatric symptoms.
4. Psychiatric Evaluation:
• Description: A psychiatrist or psychologist will conduct a detailed assessment, which might involve structured clinical interviews or standardized questionnaires.
• Purpose: To understand the individual's mental state better, ascertain the presence of any core psychotic symptoms, and evaluate the individual's mood, thought processes, and potential risk factors.
5. Brain Imaging:
• Description: Tests like Magnetic Resonance Imaging (MRI) or Computed Tomography (CT) scan might sometimes be used.
• Purpose: While not commonly employed solely for the diagnosis of brief psychotic disorder, these tests can help rule out other neurological conditions, such as tumours or infections, which might present with psychotic symptoms.
6. Duration of Symptoms:
• Description: For a diagnosis of brief psychotic disorder, symptoms must last for at least a day but no longer than a month.
• Purpose: This criterion helps differentiate brief psychotic disorder from other related disorders. For instance, schizophreniform disorder has similar symptoms but lasts for one to six months, while schizophrenia has a duration of six months or more.
7. Exclusion of Other Disorders:
• Description: It's essential to ensure that the symptoms aren't better explained by another psychiatric disorder, a substance-induced psychotic disorder, or a medical condition.
• Purpose: Many disorders and conditions can present with psychotic symptoms. By ruling them out, clinicians can ensure an accurate diagnosis and appropriate treatment.
Treatments
The primary goal of treating brief psychotic disorder is to alleviate acute symptoms, ensure the safety of the individual and those around them, and prevent potential recurrence. Here's a detailed exploration of the treatment modalities:
1. Hospitalization:
• Description: In many cases, especially if the individual is deemed a risk to themselves or others, brief hospitalization may be necessary.
• Purpose: The controlled environment of a hospital provides a safe space, ensures the individual receives appropriate care and monitoring, addresses immediate needs like nutrition and sleep, and stabilizes the patient before transitioning to outpatient care.
2. Antipsychotic Medications:
• Description: These are the primary pharmacological treatments used to manage psychotic symptoms.
• Typical Antipsychotics: Such as haloperidol (Haldol) or chlorpromazine. • Atypical Antipsychotics: Such as risperidone (Risperdal), olanzapine (Zyprexa), quetiapine (Seroquel), or aripiprazole (Abilify).
• Purpose: Antipsychotic drugs can help reduce or eliminate symptoms such as hallucinations, delusions, and disorganized thinking. They work by affecting the balance of neurotransmitters in the brain.
3. Psychotherapy (Talk Therapy):
• Description: Individual sessions with a therapist can be beneficial once acute symptoms have subsided.
• Purpose: Psychotherapy helps the individual understand the episode, develop coping strategies, address any underlying issues or stressors, and reduce the risk of recurrence. Cognitive-behavioural therapy (CBT) can be particularly effective.
4. Group Therapy or Support Groups:
• Description: These are structured sessions where individuals with similar experiences come together to share and learn.
• Purpose: They offer a platform for individuals to share experiences, gain insight, find mutual support, and learn coping mechanisms. Realizing that they're not alone in their experience can be immensely therapeutic.
5. Family Therapy:
• Description: Given that family dynamics can be a factor or can be affected by an individual's episode, involving the family in therapy can be beneficial.
• Purpose: This helps family members understand the disorder, equips them with strategies to offer support, and may address potential familial stressors. 6. Short-Term Benzodiazepines: • Description: Benzodiazepines, like lorazepam (Ativan) or diazepam (Valium), are sometimes used in conjunction with antipsychotics.
• Purpose: They can help with extreme agitation or insomnia associated with the psychotic episode. However, they are typically used short-term due to concerns about dependency. 7. Electroconvulsive Therapy (ECT):
• Description: While less common, ECT is sometimes considered for severe cases or when other treatments don't yield results.
• Purpose: ECT involves passing controlled electric currents through the brain to alleviate severe psychiatric symptoms. It can be especially useful if depressive symptoms are present alongside psychosis.
8. Maintenance and Follow-up:
• Description: Once the acute episode resolves, follow-up appointments are essential.
• Purpose: Regular check-ins with a psychiatrist or therapist ensure ongoing recovery, monitor for any signs of relapse, and adjust treatment plans as necessary. This phase might also involve tapering off medications under medical supervision.
Preventive Measures
Preventive measures for Brief Psychotic Disorder (BPD) primarily focus on identifying and managing underlying risk factors. Early intervention for individuals experiencing significant stress, trauma, or emotional turmoil can be crucial. Promoting mental health awareness, stress reduction techniques, and providing support systems are essential preventive strategies. Timely access to mental health services, psychoeducation about coping mechanisms, stress management, and healthy lifestyle choices such as regular exercise, balanced nutrition, and adequate sleep can potentially mitigate the risk of BPD. Additionally, creating a supportive and understanding environment, reducing substance use, and managing psychiatric conditions or stressors promptly can significantly lower the likelihood of BPD occurrences.
Do's & Don’t's
| Do's | Don't |
| Do: Remain calm and composed. | Don't: React with fear or panic. |
| Do: Listen actively and empathetically. | Don't: Invalidate their experiences or feelings. |
| Do: Encourage seeking professional help. | Don't: Attempt to diagnose or treat on your own. |
| Do: Offer reassurance and support. | Don't: Minimize their distress or symptoms. |
| Do: Create a safe and supportive environment. | Don't: Argue or try to reason with delusions. |
| Do: Respect their need for personal space. | Don't: Ignore or dismiss their behavior changes. |
| Do: Communicate calmly and clearly. | Don't: Confront or challenge their beliefs directly. |
| Do: Seek guidance from mental health experts. | Don't: Share their private information without consent. |
If you suspect you or someone else is experiencing Brief Psychotic Disorder, it is crucial to seek immediate medical attention by calling emergency services or consult with a Psychologist.
.webp)


 040 6700 0000
040 6700 0000  040 6700 0111
040 6700 0111