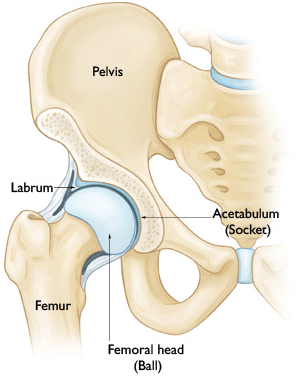
Definition
The acetabular labrum of the hip is a fibrocartilaginous structure that surrounds the rim of the acetabulum. It is contiguous with the transverse acetabular ligament (TAL) across the acetabular notch in inferomedially. The labrum is widest in the anterior hat and thickest in the superior half. It is contiguous with the articular highland cartilage that lines the socket of the acetabulum and asked to cushion the hip joint. It is attached to the edge of the bony acetabulum via a fin segment of bone that extends into the tissue via a zone of calcified cartilage and it inheres directly to the outer surface of this bony extension without a zone of calcified cartilage. Importantly, the labrum is separated from the hip joint capsule by a narrow synovial-lined recess.
The labrum functions to enhance the stability of the hip joint by maintaining the negative intra-articular pressure within the joint as well as by increasing congruity between the femoral head and the acetabular socket. It has also been shown that the labrum functions to decrease contact pressures within the hip and to decrease cartilage surface consolidation. Via its “joint sealing” effect, the labrum acts to maintain articular fluid in contact with the weight-bearing cartilage to help protect the cartilage and dissipate pressure during weight bearing exercises and activity. Tears of the labrum have been shown to closely correlate with cartilage disease (chondral delamination) of the hip, potentially leading to progressive osteoarthritis.
Diagnosis Of Labral Tears Of The Hip
Presentation
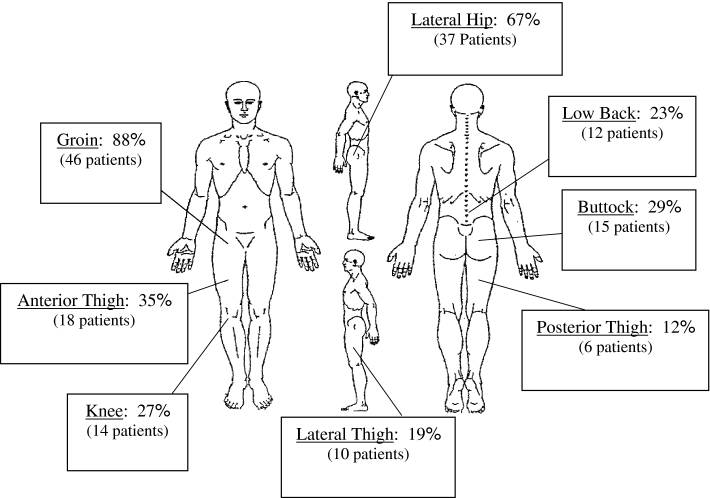
The clinical presentation of patients with an acetabular labral tear is often variable and as a result of the diagnosis is often missed initially. Patients commonly state that they have been treated by a number of previous physicians for other diagnoses, including an adductor tendon strain (groin strain), athletic pubalgia (sports hernia), or back pain. This study by Burkett et al (JBJS 2006) looked at the clinical presentation of 66 patients with an arthroscopy-confirmed acetabular labral tear. The initial presentation was insidious in 40 patients, was associated with a low-energy acute injury in 20, and was associated with major trauma in 6. Moderate to severe pain was reported by 86% of patients, with groin pain predominating (61 patients; 92%). 91% of patients had activity-related pain and 71% of patients had night pain. On examination, 39% of patients had a limp, 38% had a positive Trendelenburg sign, and sixty-three (95%) had a positive impingement sign. The mean time from the onset of symptoms to the diagnosis of a labral tear was twenty-one months. A mean of 3.3 health-care providers had been seen by the patients prior to the definitive diagnosis. Surgery on another anatomic site had been recommended for eleven patients (17%), and 4 had undergone an unsuccessful operative procedure prior to the diagnosis of the labral tear.
Imaging And Diagnostic Studies
A series of standard radiographs are critical as part of the initial assessment to evaluate the patient for osteoarthritis, femoroacetabular impingement (FAI), and hip dysplasia. The imaging modality most commonly used to confirm a labral tear is an MRI or MR-Arthrogram (an MRI with intra-articular contrast/dye). Multiple studies have demonstrated the superior accuracy of MR-arthrography as compared with standard magnetic resonance imaging for the diagnosis of labral tear. Intra-articular gadolinium has been shown to improve the sensitivity of diagnosing labral pathology. However, recent advances in standard magnetic resonance imaging, including the use of 3-Tesla magnets, has improved the accuracy in diagnosing acetabular labral tears with standard non-contrast MRIs.
In cases where the diagnosis of a labral tear is equivocal or in which a tear has been diagnosed by MRI but it is uncertain whether the patient’s symptoms are related to the tear, an intra-articular injection of local anaesthetic (lidocaine) combined with corticosteroid can be a useful diagnostic tool. If the patient’s symptoms improve with this injection, it can be assumed that the intra-articular pathology (ie. the labral tear) is responsible for the patient’s pain and symptoms.

Surgical Indications
The primary indication for elective surgery is ALWAYS based around patient symptomatology and a failure of conservative modalities. In most cases, patients presenting with labral pathology have tried various forms of conservative treatment, including physical therapy, NSAID medications, activity modification, and rest, and have failed to improve. Furthermore, their hip symptoms have started to affect their ability to take part in activities they enjoy and might be starting to affect their day-to-day lives including their ability to sleep at night.
Indications include:
-
Persistent pain in the groin with weight bearing exercises and activities that has failed conservative management.
-
Mechanical symptoms with rotational activities
-
Concomitant femoral acetabular impingement (FAI) with a repairable acetabular labral tear.
Surgical Technique
Dr. Dold performs hip arthroscopy through 2 to 3 keyhole size incisions around the hip. He is one of the first physicians in Texas to utilize a post-free hip table for arthroscopy. Previously, a post was placed between the patient’s legs to distract the hip from the joint – this was associated with increased post-operative pain and a risk of nerve injury and post-operative numbness in the groin.
Arthroscopic instruments are used to remove the pathologic bone responsible for the impingement, re-contouring the acetabular rim and femoral head-neck junction to restore normal anatomy and repair the torn labral tissue. A video of an acetabular labral repair can be found here.
Recovery from hip arthroscopy ranges from patient to patient. Typically, patients reach a clinical improvement between 3 and 6 months post-surgery. However, clinical improvement can continue up to two years post-surgery.
Paper: When Do Patients Improve After Hip Arthroscopy for Femoroacetabular Impingement? A Prospective Cohort Analysis (AJSM 2018).


