Munro DD. Multiple active junctional naevi with family history of malignant melanoma. Proc R Soc Med. 1974 Jun. 67(7):594-5. [QxMD MEDLINE Link].
Clark WH Jr, Reimer RR, Greene M, Ainsworth AM, Mastrangelo MJ. Origin of familial malignant melanomas from heritable melanocytic lesions. 'The B-K mole syndrome'. Arch Dermatol. 1978 May. 114(5):732-8. [QxMD MEDLINE Link].
Clark WH Jr, Elder DE, Guerry D 4th, Epstein MN, Greene MH, Van Horn M. A study of tumor progression: the precursor lesions of superficial spreading and nodular melanoma. Hum Pathol. 1984 Dec. 15(12):1147-65. [QxMD MEDLINE Link].
Duffy K, Grossman D. The dysplastic nevus: from historical perspective to management in the modern era: part I. Historical, histologic, and clinical aspects. J Am Acad Dermatol. 2012 Jul. 67 (1):1.e1-16; quiz 17-8. [QxMD MEDLINE Link].
Elder DE, Goldman LI, Goldman SC, Greene MH, Clark WH Jr. Dysplastic nevus syndrome: a phenotypic association of sporadic cutaneous melanoma. Cancer. 1980 Oct 15. 46(8):1787-94. [QxMD MEDLINE Link].
Lynch HT, Frichot BC 3rd, Lynch JF. Familial atypical multiple mole-melanoma syndrome. J Med Genet. 1978 Oct. 15 (5):352-6. [QxMD MEDLINE Link].
Reed RJ. A classification of melanocytic dysplasias and malignant melanomas. Am J Dermatopathol. 1984 Summer. 6 Suppl:195-206. [QxMD MEDLINE Link].
Rhodes AR, Mihm MC Jr, Weinstock MA. Dysplastic melanocytic nevi: a reproducible histologic definition emphasizing cellular morphology. Mod Pathol. 1989 Jul. 2 (4):306-19. [QxMD MEDLINE Link].
Ackerman AB. What naevus is dysplastic, a syndrome and the commonest precursor of malignant melanoma? A riddle and an answer. Histopathology. 1988 Sep. 13 (3):241-56. [QxMD MEDLINE Link].
Annessi G, Cattaruzza MS, Abeni D, Baliva G, Laurenza M, Macchini V, et al. Correlation between clinical atypia and histologic dysplasia in acquired melanocytic nevi. J Am Acad Dermatol. 2001 Jul. 45(1):77-85. [QxMD MEDLINE Link].
Clemente C, Cochran AJ, Elder DE, Levene A, MacKie RM, Mihm MC, et al. Histopathologic diagnosis of dysplastic nevi: concordance among pathologists convened by the World Health Organization Melanoma Programme. Hum Pathol. 1991 Apr. 22(4):313-9. [QxMD MEDLINE Link].
Klein LJ, Barr RJ. Histologic atypia in clinically benign nevi. A prospective study. J Am Acad Dermatol. 1990 Feb. 22(2 Pt 1):275-82. [QxMD MEDLINE Link].
Lebe B, Pabuççuoglu U, Ozer E. The significance of Ki-67 proliferative index and cyclin D1 expression of dysplastic nevi in the biologic spectrum of melanocytic lesions. Appl Immunohistochem Mol Morphol. 2007 Jun. 15(2):160-4. [QxMD MEDLINE Link].
Massi D, Naldini A, Ardinghi C, Carraro F, Franchi A, Paglierani M, et al. Expression of protease-activated receptors 1 and 2 in melanocytic nevi and malignant melanoma. Hum Pathol. 2005 Jun. 36(6):676-85. [QxMD MEDLINE Link].
Clarke LE. Dysplastic nevi. Clin Lab Med. 2011 Jun. 31(2):255-65. [QxMD MEDLINE Link].
Reddy KK, Farber MJ, Bhawan J, Geronemus RG, Rogers GS. Atypical (dysplastic) nevi: outcomes of surgical excision and association with melanoma. JAMA Dermatol. 2013 Aug. 149(8):928-34. [QxMD MEDLINE Link].
NIH Consensus Conference. Diagnosis and treatment of early melanoma. JAMA. 1992 Sep 9. 268(10):1314-9. [QxMD MEDLINE Link].
Cannon-Albright LA, Goldgar DE, Meyer LJ, Lewis CM, Anderson DE, Fountain JW, et al. Assignment of a locus for familial melanoma, MLM, to chromosome 9p13-p22. Science. 1992 Nov 13. 258(5085):1148-52. [QxMD MEDLINE Link].
Nobori T, Miura K, Wu DJ, Lois A, Takabayashi K, Carson DA. Deletions of the cyclin-dependent kinase-4 inhibitor gene in multiple human cancers. Nature. 1994 Apr 21. 368(6473):753-6. [QxMD MEDLINE Link].
Bale SJ, Dracopoli NC, Tucker MA, Clark WH Jr, Fraser MC, Stanger BZ, et al. Mapping the gene for hereditary cutaneous malignant melanoma-dysplastic nevus to chromosome 1p. N Engl J Med. 1989 May 25. 320(21):1367-72. [QxMD MEDLINE Link].
Celebi JT, Ward KM, Wanner M, Polsky D, Kopf AW. Evaluation of germline CDKN2A, ARF, CDK4, PTEN, and BRAF alterations in atypical mole syndrome. Clin Exp Dermatol. 2005 Jan. 30(1):68-70. [QxMD MEDLINE Link].
Chaudru V, Laud K, Avril MF, Minière A, Chompret A, Bressac-de Paillerets B, et al. Melanocortin-1 receptor (MC1R) gene variants and dysplastic nevi modify penetrance of CDKN2A mutations in French melanoma-prone pedigrees. Cancer Epidemiol Biomarkers Prev. 2005 Oct. 14(10):2384-90. [QxMD MEDLINE Link].
Celebi JT, Ward KM, Wanner M, Polsky D, Kopf AW. Evaluation of germline CDKN2A, ARF, CDK4, PTEN, and BRAF alterations in atypical mole syndrome. Clin Exp Dermatol. 2005 Jan. 30 (1):68-70. [QxMD MEDLINE Link].
Uribe P, Wistuba II, Gonzalez S. Allelotyping, microsatellite instability, and BRAF mutation analyses in common and atypical melanocytic nevi and primary cutaneous melanomas. Am J Dermatopathol. 2009 Jun. 31(4):354-63. [QxMD MEDLINE Link].
Ardakani NM. Dysplastic/Clark naevus in the era of molecular pathology. Australas J Dermatol. 2019 Aug. 60 (3):186-191. [QxMD MEDLINE Link].
Melamed RD, Aydin IT, Rajan GS, Phelps R, Silvers DN, Emmett KJ, et al. Genomic Characterization of Dysplastic Nevi Unveils Implications for Diagnosis of Melanoma. J Invest Dermatol. 2017 Apr. 137 (4):905-909. [QxMD MEDLINE Link].
[Guideline] IARC Working Group. Special Report: Policy A Review of human carcinogens- Part D: radiation. The Lancet. 2009/08. 10:751-752. [Full Text].
IARC Working Group. The association of use of sunbeds with cutaneous malignant melanoma and other skin cancers: a systematic review. Int J Cancer. 2006. 120:1116-22.
Tsao H, Sober AJ. Atypical melanocytic nevi. Freedburg IM, ed. Fitzpatrick's Dermatology in General Medicine. 6th ed. New York, NY: McGraw-Hill; 2003. Vol 1: 906-16.
Kraemer KH, Greene MH, Tarone R, Elder DE, Clark WH Jr, Guerry D 4th. Dysplastic naevi and cutaneous melanoma risk. Lancet. 1983 Nov 5. 2(8358):1076-7. [QxMD MEDLINE Link].
Cooke KR et al. Dysplastic naevi in a population-based survey. Cancer. 1989. 63:1240.
Goldstein AM, Chan M, Harland M, et al. Features associated with germline CDKN2A mutations: a GenoMEL study of melanoma-prone families from three continents. J Med Genet. 2007 Feb. 44 (2):99-106. [QxMD MEDLINE Link].
Banky JP, Kelly JW, English DR, Yeatman JM, Dowling JP. Incidence of new and changed nevi and melanomas detected using baseline images and dermoscopy in patients at high risk for melanoma. Arch Dermatol. 2005 Aug. 141(8):998-1006. [QxMD MEDLINE Link].
Halpern AC, Guerry D 4th, Elder DE, Trock B, Synnestvedt M, Humphreys T. Natural history of dysplastic nevi. J Am Acad Dermatol. 1993 Jul. 29 (1):51-7. [QxMD MEDLINE Link].
Salopek TG. The dilemma of the dysplastic nevus. Dermatol Clin. 2002 Oct. 20(4):617-28, viii. [QxMD MEDLINE Link].
Bevona C, Goggins W, Quinn T, Fullerton J, Tsao H. Cutaneous melanomas associated with nevi. Arch Dermatol. 2003 Dec. 139(12):1620-4; discussion 1624. [QxMD MEDLINE Link].
Geller AC, Swetter SM, Brooks K, Demierre MF, Yaroch AL. Screening, early detection, and trends for melanoma: current status (2000-2006) and future directions. J Am Acad Dermatol. 2007 Oct. 57(4):555-72; quiz 573-6. [QxMD MEDLINE Link].
Silva JH, Sá BC, Avila AL, Landman G, Duprat Neto JP. Atypical mole syndrome and dysplastic nevi: identification of populations at risk for developing melanoma - review article. Clinics (Sao Paulo). 2011. 66(3):493-9. [QxMD MEDLINE Link]. [Full Text].
Marinkovic M, Janjic Z, Nikolic J. Dysplastic nevus--a risk factor of developing skin melanoma clinical and epidemiological study with retrospective review of literature. Med Pregl. 2011 May-Jun. 64(5-6):315-8. [QxMD MEDLINE Link].
Gandini S, Sera F, Cattaruzza MS, Pasquini P, Abeni D, Boyle P, et al. Meta-analysis of risk factors for cutaneous melanoma: I. Common and atypical naevi. Eur J Cancer. 2005 Jan. 41 (1):28-44. [QxMD MEDLINE Link].
Alendar T, Kittler H. Morphologic characteristics of nevi associated with melanoma: a clinical, dermatoscopic and histopathologic analysis. Dermatol Pract Concept. 2018 Apr. 8 (2):104-108. [QxMD MEDLINE Link]. [Full Text].
Pampena R, Kyrgidis A, Lallas A, et al. A meta-analysis of nevus-associated melanoma: Prevalence and practical implications. J Am Acad Dermatol. 2017 Nov. 77 (5):938-945.e4. [QxMD MEDLINE Link].
Kanzler MH, Swetter SM. Malignant melanoma. J Am Acad Dermatol. 2003 May. 48(5):780-3. [QxMD MEDLINE Link].
de Snoo FA, Kroon MW, Bergman W, ter Huurne JE, Houwing-Duistermaat JJ, van Mourik L, et al. From sporadic atypical nevi to familial melanoma: risk analysis for melanoma in sporadic atypical nevus patients. J Am Acad Dermatol. May 2007. 56:748-52. [QxMD MEDLINE Link].
Popa LG, Giurcaneanu C, Nitipir C, et al. Dysplastic nevus syndrome and pancreatic cancer: A case report. Exp Ther Med. 2022 Jan. 23 (1):31. [QxMD MEDLINE Link]. [Full Text].
Leachman SA, Carucci J, Kohlmann W, Banks KC, Asgari MM, Bergman W. Selection criteria for genetic assessment of patients with familial melanoma. J Am Acad Dermatol. 2009 Oct. 61(4):677.e1-14. [QxMD MEDLINE Link].
Singh AD, Damato B, Howard P, Harbour JW. Uveal melanoma: genetic aspects. Ophthalmol Clin North Am. 2005 Mar. 18(1):85-97, viii. [QxMD MEDLINE Link].
Lynch HT, Fusaro RM, Lynch JF. Hereditary cancer syndrome diagnosis: molecular genetic clues and cancer control. Future Oncol. 2007 Apr. 3(2):169-81. [QxMD MEDLINE Link].
Bronsnick T, Kazi N, Kirkorian AY, Rao BK. Outcomes of biopsies and excisions of dysplastic acral nevi: a study of 187 lesions. Dermatol Surg. 2014 Apr. 40(4):455-9. [QxMD MEDLINE Link].
Tchernev G, Patterson JW. Telmisartan/hydrochlorothiazide-induced nevus-associated cutaneous melanoma: first report in the medical literature. Expert Rev Clin Pharmacol. 2021 Mar. 14 (3):289-293. [QxMD MEDLINE Link].
Roesch A, Burgdorf W, Stolz W, Landthaler M, Vogt T. Dermatoscopy of "dysplastic nevi": a beacon in diagnostic darkness. Eur J Dermatol. 2006 Sep-Oct. 16(5):479-93. [QxMD MEDLINE Link].
Pellacani G, Farnetani F, Gonzalez S, Longo C, Cesinaro AM, Casari A, et al. In vivo confocal microscopy for detection and grading of dysplastic nevi: a pilot study. J Am Acad Dermatol. MAR/2012. 66:e109-21. [QxMD MEDLINE Link].
Balu M, Kelly KM, Zachary CB, Harris RM, Krasieva TB, König K, et al. Distinguishing between benign and malignant melanocytic nevi by in vivo multiphoton microscopy. Cancer Res. 2014 May 15. 74 (10):2688-97. [QxMD MEDLINE Link].
Babacan A, Lebe B. Grade of Atypia in Dysplastic Nevi and Relationship with Dermal Fibroplasia. Turk Patoloji Derg. 2012. 28(1):17-23. [QxMD MEDLINE Link].
Campoli M, Fitzpatrick JE, High W, Ferrone S. HLA antigen expression in melanocytic lesions: Is acquisition of HLA antigen expression a biomarker of atypical (dysplastic) melanocytes?. J Am Acad Dermatol. 2012 Jun. 66(6):911-916.e8. [QxMD MEDLINE Link].
Valdebran M, Bandino J, Elbendary A, et al. Nuclear and cytoplasmic features in the diagnosis of Clark's nevi. J Cutan Pathol. 2018 Mar. 45 (3):204-207. [QxMD MEDLINE Link]. [Full Text].
Farrahi F, Egbert BM, Swetter SM. Histologic similarities between lentigo maligna and dysplastic nevus: importance of clinicopathologic distinction. J Cutan Pathol. 2005 Jul. 32(6):405-12. [QxMD MEDLINE Link].
Strazzula L, Vedak P, Hoang MP, Sober A, Tsao H, Kroshinsky D. The utility of re-excising mildly and moderately dysplastic nevi: A retrospective analysis. J Am Acad Dermatol. 2014 Dec. 71(6):1071-6. [QxMD MEDLINE Link].
Mendese G, Maloney M, Bordeaux J. To scoop or not to scoop: the diagnostic and therapeutic utility of the scoop-shave biopsy for pigmented lesions. Dermatol Surg. 2014 Oct. 40(10):1077-83. [QxMD MEDLINE Link].
Comfere NI, Chakraborty R, Peters MS. Margin comments in dermatopathology reports on dysplastic nevi influence re-excision rates. J Am Acad Dermatol. 2013 Nov. 69(5):687-92. [QxMD MEDLINE Link].
Reddy KK, Farber MJ, Bhawan J, Geronemus RG, Rogers GS. Atypical (dysplastic) nevi: outcomes of surgical excision and association with melanoma. JAMA Dermatol. 2013 Aug. 149(8):928-34. [QxMD MEDLINE Link].
Duffy KL, Mann DJ, Petronic-Rosic V, Shea CR. Clinical decision making based on histopathologic grading and margin status of dysplastic nevi. Arch Dermatol. 2012 Feb. 148(2):259-60. [QxMD MEDLINE Link].
Somani N, Martinka M, Crawford RI, Dutz JP, Rivers JK. Treatment of atypical nevi with imiquimod 5% cream. Arch Dermatol. 2007 Mar. 143(3):379-85. [QxMD MEDLINE Link].
Francis SO, Mahlberg MJ, Johnson KR, Ming ME, Dellavalle RP. Melanoma chemoprevention. J Am Acad Dermatol. 2006 Nov. 55(5):849-61. [QxMD MEDLINE Link].
Tripp JM, Kopf AW, Marghoob AA, Bart RS. Management of dysplastic nevi: a survey of fellows of the American Academy of Dermatology. J Am Acad Dermatol. 2002 May. 46(5):674-82. [QxMD MEDLINE Link].
 This mole has a characteristic “fried-egg” appearance. The eccentric papule is an ordinary nevus. The diagnostic histologic features are found in the macular portion of the mole, particularly at the shoulder (ie, where the papule meets the macule). Courtesy of the National Cancer Institute, via Wikimedia Commons.
This mole has a characteristic “fried-egg” appearance. The eccentric papule is an ordinary nevus. The diagnostic histologic features are found in the macular portion of the mole, particularly at the shoulder (ie, where the papule meets the macule). Courtesy of the National Cancer Institute, via Wikimedia Commons.
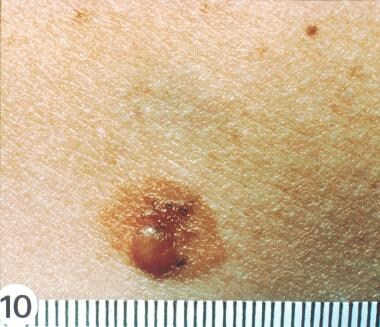
 Atypical nevus. The delicate, hazy, tan, macular rim of this lesion, although not clinically dramatic, represents persistent melanocytic proliferation beyond the lateral limits of the common mole at its center. Courtesy of the National Cancer Institute, via Wikimedia Commons.
Atypical nevus. The delicate, hazy, tan, macular rim of this lesion, although not clinically dramatic, represents persistent melanocytic proliferation beyond the lateral limits of the common mole at its center. Courtesy of the National Cancer Institute, via Wikimedia Commons.
 Atypical nevus. The central portion of this mole is a complex papule. The periphery of the lesion is macular, indistinct, slightly pink. Courtesy of the National Cancer Institute, via Wikimedia Commons.
Atypical nevus. The central portion of this mole is a complex papule. The periphery of the lesion is macular, indistinct, slightly pink. Courtesy of the National Cancer Institute, via Wikimedia Commons.










