Approach Considerations
Pituitary apoplexy can present in a variery of different ways, and if one is not familiar with the diagnosis, it can be missed with devastating consequences. Thus, laboratory studies and neuro-imaging are key to the diagnosis.
Laboratory Studies
At least one anterior pituitary deficiency always is present at the onset of pituitary apoplexy, with corticotropic deficiency being the most common and most life-threatening, affecting 60%-80% of patients. [26] Electrolytes, glucose, pituitary hormones, and plasma/urine osmolality should be evaluated.
Imaging Studies
CT scanning and MRI are radiologic tests used to evaluate the pituitary.
CT scanning generally is the initial imaging study of choice in the emergency department for patients who present with sudden-onset severe headache, visual loss, and/or ophthalmoplegia suggestive of SAH. CT scanning can help to exclude SAH from an aneurysm by showing an intrasellar mass with hemorrhagic components, seen in 80% of pituitary apoplexy cases. [26]
Binning and colleagues reported 6 patients with Rathke cleft cyst apoplexy presenting with the clinical and imaging features of both hemorrhagic and nonhemorrhagic pituitary apoplexy. [27]
Kaplun and colleagues reported the MRI evolution of pituitary changes in 2 patients with Sheehan syndrome. [28] The first case initially had the pituitary ring sign, although MRI later showed an empty sella with shrinkage of the pituitary.
Liu et al reported spontaneous partial or complete radiological disappearance of adenoma following pituitary apoplexy without the use of dopaminergic agonists (which may result in regression of pituitary adenoma). [29]
MRI, as seen in the images below, is the most sensitive imaging study for evaluating the pituitary gland, possibly visualizing hemorrhage not seen on CT scan.
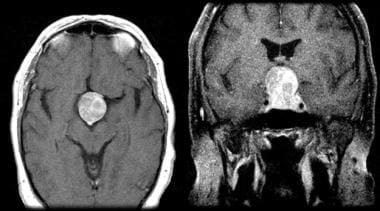 Enhanced axial and coronal T1-weighted MRI of a typical large pituitary tumor with a "snowman" configuration (coronal) and marked enhancement with contrast. This tumor has not undergone apoplexy.
Enhanced axial and coronal T1-weighted MRI of a typical large pituitary tumor with a "snowman" configuration (coronal) and marked enhancement with contrast. This tumor has not undergone apoplexy.
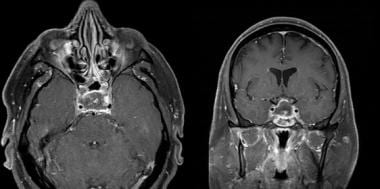 Enhanced T1-weighted axial and coronal MRI showing a large pituitary tumor that has recently undergone ischemic apoplexy showing a necrotic (hypointense) center and ring of gadolinium enhancement (hyperintense), ie, the "pituitary ring sign." There is a small area of hemorrhagic blush in the center of the necrosis.
Enhanced T1-weighted axial and coronal MRI showing a large pituitary tumor that has recently undergone ischemic apoplexy showing a necrotic (hypointense) center and ring of gadolinium enhancement (hyperintense), ie, the "pituitary ring sign." There is a small area of hemorrhagic blush in the center of the necrosis.
In the first 3-5 days, hemorrhage within the sella is isointense or hypointense on T1-weighted images. On T2-weighted sequences, the blood appears hypointense.
A characteristic MRI finding in ischemic (nonhemorrhagic) pituitary apoplexy is an enlarged pituitary gland bulging under the optic chiasm with peripheral enhancement surrounding a hypointense gland. Vaphiades coined the phrase "pituitary ring sign" to denote this MRI appearance. [18] Vaphiades retrospectively reviewed the cranial MRIs of 3 patients with ischemic (nonhemorrhagic) pituitary apoplexy; all 3 patients displayed the "pituitary ring sign." [18]
This MRI appearance of the “pituitary ring” was first noted in 1995 by Lavalee et al in a patient with Sheehan syndrome on a contrast-enhanced CT scan and on a T1-weighted contrast-enhanced MRI and thought to be unique to ischemic apoplexy in patients with Sheehan syndrome. [30]
In 1998, Kleinschmidt-Demasters and Lillehei reported the pathological and MRI features of 15 patients with pituitary adenomas presenting with apoplexy. On T1-weighted contrast-enhanced MRI, they observed a peripheral rim of enhancement with gadolinium in 10 cases. [31]
Subsequent reports corroborated this MRI finding in patients with ischemic pituitary apoplexy. [32, 33]
The presumed etiology of the hypointense center in the pituitary gland is necrosis, which does not enhance with gadolinium on T1-weighted MRI. The enhancing part of the tumor is the outer-most portion of the infarcted pituitary or its “skin.” This was found to correspond to the presence of granulation tissue and lymphocytosis at histologic examination. [31]
Sphenoid sinus mucosal thickening in the setting of pituitary apoplexy was first described by Arita et al in 2001. They retrospectively evaluated 14 patients with pituitary apoplexy. The mucosa of the sphenoid sinus on MRI had thickened the compartment just beneath the sella turcica in 9 of 11 patients when performed within 7 days after the onset of apoplectic symptoms. Controls consisted of MRIs obtained in 100 consecutive patients with pituitary adenomas but without apoplectic symptoms. Included in this group were 58 functioning and 42 nonfunctioning pituitary adenomas. Fifteen patients experienced thickening of the sphenoid sinus mucosa, including 5 with some apparent pansinusitis. The incidence of mucosal thickening of the sphenoid sinus in patients with apoplexy was significantly greater than that in the patients without apoplexy. [34] On histopathological specimens in patents with apoplexy, the thickened sphenoid sinus mucosa demonstrates a swollen subepithelial layer presumably responsible for the rim of MRI gadolinium enhancement. [34]
In 2006, Liu et al performed a retrospective review of 28 patients with pituitary apoplexy. Thickening of sphenoid sinus mucosa was found in 22 (79%) of these patients. They also noted that patients with thickened sphenoid sinus mucosa had larger tumors, a higher rate of cranial nerve deficits at presentation than those without mucosal thickening, and a higher rate of hypopituitarism and subsequent long-term hormone replacement therapy compared to patients without thickened mucosa. [35]
In 2011, Agrawal et al concluded that there is a temporal association with the radiographic finding of sphenoid sinus mucosal thickening and pituitary apoplexy and that sphenoid sinus mucosal thickening may precede an apoplectic event. [36]
In 2017, Vaphiades reviewed twelve cases of ischemic pituitary apoplexy, all of which showed both the "pituitary ring sign" and "sphenoid sinus mucosal thickening" signs on MRI. The twelve cases were composed of ten cases from the literature (3 of which were published by this author) and two cases recently evaluated in the author’s hospital. Thus, five of the twelve cases were evaluated by this author. Five of the twelve patients had both headache and visual loss, five had headache alone, and two had no initial symptoms (nonfunctioning pituitary adenomas were incidentally found on MRI). These findings indicate that each sign ("pituitary ring sign" and "sphenoid sinus mucosal thickening") may exist alone with or without pituitary apoplexy, yet both signs together in the appropriate clinical context is a strong predictor of pituitary apoplexy. This is important because timely diagnosis treatment of pituitary apoplexy may be vision- and life-saving in this disorder. [37]
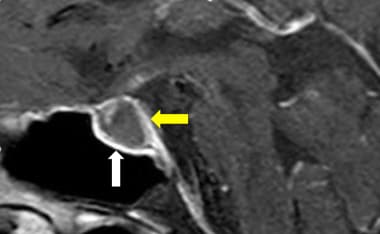 Post-contrast sagittal T1-weighted scan shows sphenoid sinus roof mucosal thickening. The yellow arrow shows the “pituitary ring sign,” while the white arrow shows sphenoid sinus roof mucosal thickening. Courtesy of Taylor & Francis (Vaphiades MS. Pituitary Ring Sign Plus Sphenoid Sinus Mucosal Thickening: Neuroimaging Signs of Pituitary Apoplexy. Neuroophthalmology. 2017 Dec. 41 (6):306-309. Online at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5764063/.).
Post-contrast sagittal T1-weighted scan shows sphenoid sinus roof mucosal thickening. The yellow arrow shows the “pituitary ring sign,” while the white arrow shows sphenoid sinus roof mucosal thickening. Courtesy of Taylor & Francis (Vaphiades MS. Pituitary Ring Sign Plus Sphenoid Sinus Mucosal Thickening: Neuroimaging Signs of Pituitary Apoplexy. Neuroophthalmology. 2017 Dec. 41 (6):306-309. Online at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5764063/.).
Histologic Findings
Histologically, many of these tumors display hemorrhagic necrosis in their substance. This has been postulated to result from unrecognized episodes of focal hemorrhage. Bills reviewed histories of 37 patients with symptomatic pituitary apoplexy. [38] By immunostaining criteria, null-cell adenomas were the most frequent tumor type found.
-
Enhanced coronal CT showing large pituitary tumor with a "snowman" configuration and heterogeneous density (mixed signal) within the tumor indicative of pituitary apoplexy. Hemorrhage was confirmed at surgery.
-
Enhanced axial and coronal T1-weighted MRI of a typical large pituitary tumor with a "snowman" configuration (coronal) and marked enhancement with contrast. This tumor has not undergone apoplexy.
-
Enhanced T1-weighted axial and coronal MRI showing a large pituitary tumor that has recently undergone ischemic apoplexy showing a necrotic (hypointense) center and ring of gadolinium enhancement (hyperintense), ie, the "pituitary ring sign." There is a small area of hemorrhagic blush in the center of the necrosis.
-
Automated visual field showing a bitemporal field defect due to compression of the optic chiasm from below.
-
Post-contrast sagittal T1-weighted scan shows sphenoid sinus roof mucosal thickening. The yellow arrow shows the “pituitary ring sign,” while the white arrow shows sphenoid sinus roof mucosal thickening. Courtesy of Taylor & Francis (Vaphiades MS. Pituitary Ring Sign Plus Sphenoid Sinus Mucosal Thickening: Neuroimaging Signs of Pituitary Apoplexy. Neuroophthalmology. 2017 Dec. 41 (6):306-309. Online at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5764063/.).







