History
Two phases of the disease process exist: the active phase and the scarring (cicatricial) phase. As implied above, though, these phases are not stages along a linear pathway of disease pathogenesis; both phases may coexist in the same patient.
The active phase resembles many other diseases in which follicular conjunctivitis is a feature. Without laboratory facilities, the diagnosis is solely based on the clinical appearance of active trachoma in someone living in a community where trachoma is endemic or suspected to be endemic.
Most patients with active trachoma are relatively asymptomatic.
The cicatricial phase has unique clinical features, which lead to definitive diagnosis in most cases.
Determine the amount of time that the patient has spent in a trachoma-endemic community and/or near a pool of infection.
Conjunctival scarring alone tends to be asymptomatic, though the associated disturbance of the architecture of the tear film (due to scarring and destruction of mucous and serous glands) often leads to dry eye.
Trichiasis causes an intensely irritating foreign body sensation, as well as blepharospasm. Ultimately, it leads to corneal scarring.
Many patients self-epilate before their presentation.
Corneal opacities or scars that cover any part of the pupil impair the patient's vision.
Physical
Active trachoma is characterized by a mucopurulent keratoconjunctivitis. The conjunctival surface of the upper eyelid shows a follicular and inflammatory response. The cornea may have limbal follicles, superior neovascularization (pannus), and punctate keratitis. Infection with C trachomatis concurrently occurs in other extraocular mucous membranes, commonly the nasopharynx, leading to a nasal discharge.
Follicular trachoma
Follicular trachoma (designated TF in the WHO simplified trachoma grading scheme) is seen in the image below.
 Trachomatous inflammation, follicular (TF), is the presence of 5 or more follicles (each at least 0.5 mm in diameter) on the central part of the upper tarsal conjunctiva. Images from the Slides/Text Teaching Series, No. 7, Trachoma, published by The International Centre for Eye Health, Institute of Ophthalmology, 11-43 Bath St, London EC1V 9EL, United Kingdom. Photograph courtesy of John D. C. Anderson, MD.
Trachomatous inflammation, follicular (TF), is the presence of 5 or more follicles (each at least 0.5 mm in diameter) on the central part of the upper tarsal conjunctiva. Images from the Slides/Text Teaching Series, No. 7, Trachoma, published by The International Centre for Eye Health, Institute of Ophthalmology, 11-43 Bath St, London EC1V 9EL, United Kingdom. Photograph courtesy of John D. C. Anderson, MD.
Follicular trachoma is defined as the presence of 5 or more follicles at least 0.5 mm in diameter in the central part of the upper tarsal conjunctiva.
Follicular trachoma indicates active disease.
This form is most commonly found in children, with a peak prevalence in those aged 3-5 years. The prevalence rapidly decreases in school-aged children as they leave the pool of re-infection (ie, their family childcare group).
Follicles are germinal centers that primarily consist of lymphocytes and monocytes.
The presence and involution of follicles at the limbus (corneoscleral border) give rise to the pathognomonic lesion of past active trachoma, Herbert pits.
Intense inflammatory trachoma
Intense inflammatory trachoma (designated TI in the WHO simplified trachoma grading scheme) is seen in the image below.
 Trachomatous inflammation, intense (TI) is pronounced inflammatory thickening of the upper tarsal conjunctiva that obscures more than one half the normal deep tarsal vessels. Photograph courtesy of Allen Foster, MD.
Trachomatous inflammation, intense (TI) is pronounced inflammatory thickening of the upper tarsal conjunctiva that obscures more than one half the normal deep tarsal vessels. Photograph courtesy of Allen Foster, MD.
Intense inflammatory trachoma is defined as pronounced inflammatory thickening of the upper tarsal conjunctiva that obscures more than one half of the normal deep tarsal vessels.
The cause is an intense inflammatory response. Like follicular trachoma, intense inflammatory trachoma indicates active disease.
The normally thin tarsal conjunctiva develops a velvety thickening.
Papillae are visible under slit lamp examination.
Intense inflammatory trachoma indicates an increased potential for significant conjunctival scarring and, hence, a higher ultimate risk of blinding disease.
Surveying the prevalence of intense inflammatory trachoma in children can help in predicting the risk of future blinding trachoma in that cohort of children.
Trachomatous scarring
Trachomatous scarring (designated TS in the WHO simplified trachoma grading scheme) is seen in the image below.
 Trachomatous conjunctival scarring (TS) is the presence of easily visible scars in the tarsal conjunctiva.
Trachomatous conjunctival scarring (TS) is the presence of easily visible scars in the tarsal conjunctiva.
Trachomatous scarring is defined as the presence of easily visible scars in the tarsal conjunctiva.
Trachomatous scarring indicates past inflammatory disease and a risk of future trichiasis. The more severe the scarring, the higher the risk of subsequent trichiasis.
This form may be associated with the development of dry eye syndrome, but chronic, low-grade bacterial conjunctivitis and dacryocystitis may also lead to a weeping eye.
Trichiasis
Trichiasis (designated TT in the WHO simplified trachoma grading scheme) is seen in the image below.
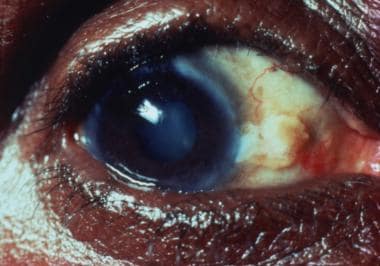 Trachomatous trichiasis (TT) is defined as the presence of at least 1 eyelash rubbing on the eyeball or evidence of recent removal of in-turned lashes. Photograph courtesy of John D. C. Anderson, MD.
Trachomatous trichiasis (TT) is defined as the presence of at least 1 eyelash rubbing on the eyeball or evidence of recent removal of in-turned lashes. Photograph courtesy of John D. C. Anderson, MD.
Trichiasis is defined as at least 1 eyelash rubs on the eyeball or evidence of recent removal of in-turned eyelashes.
This is a potentially blinding lesion that can lead to corneal opacification.
Trichiasis is due to subconjunctival fibrosis over the tarsal plate that leads to lid distortion.
Some vision can be restored with the successful correction of trichiasis.
Corneal opacity
Corneal opacity (designated CO in the WHO simplified trachoma grading scheme) is seen in the image below.
 Easily visible corneal opacity over the pupil; it is so dense that at least part of the pupil margin is blurred when viewed through the opacity. Photograph courtesy of John D. C. Anderson, MD.
Easily visible corneal opacity over the pupil; it is so dense that at least part of the pupil margin is blurred when viewed through the opacity. Photograph courtesy of John D. C. Anderson, MD.
Corneal opacity is defined as easily visible corneal opacity over the pupil that is so dense that it blurs at least part of the pupillary margin when it is viewed through the opacity.
Corneal opacity or scarring reflects the prevalence of vision loss and blindness resulting from trachoma.
This condition includes pannus, epithelial vascularization, and infiltration only if it involves the central cornea.
Causes
Trachoma is caused by repeated conjunctival infection with C trachomatis. Important individual-level risk factors for active trachoma include having siblings with active disease, having a dirty face, and crowded sleeping arrangements. At the community level, adequate water access for personal hygiene, sanitation, and fly control determine the risk of endemic trachoma.
-
Trachomatous inflammation, follicular (TF), is the presence of 5 or more follicles (each at least 0.5 mm in diameter) on the central part of the upper tarsal conjunctiva. Images from the Slides/Text Teaching Series, No. 7, Trachoma, published by The International Centre for Eye Health, Institute of Ophthalmology, 11-43 Bath St, London EC1V 9EL, United Kingdom. Photograph courtesy of John D. C. Anderson, MD.
-
Trachomatous inflammation, intense (TI) is pronounced inflammatory thickening of the upper tarsal conjunctiva that obscures more than one half the normal deep tarsal vessels. Photograph courtesy of Allen Foster, MD.
-
Trachomatous conjunctival scarring (TS) is the presence of easily visible scars in the tarsal conjunctiva.
-
Trachomatous trichiasis (TT) is defined as the presence of at least 1 eyelash rubbing on the eyeball or evidence of recent removal of in-turned lashes. Photograph courtesy of John D. C. Anderson, MD.
-
Easily visible corneal opacity over the pupil; it is so dense that at least part of the pupil margin is blurred when viewed through the opacity. Photograph courtesy of John D. C. Anderson, MD.
-
The image on the left shows intense inflammatory trachoma, and the image on the right shows allergic conjunctivitis with the typical cobblestone papillae. Courtesy of John D. C. Anderson, MD, and Murray McGavin, MD.






