Preprocedural Planning
Laboratory studies
Laboratory studies should include the following:
-
Complete blood count (CBC) with differential – This often reveals leukocytosis with a left shift
-
Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) level – These are helpful in monitoring the course of treatment
-
Blood cultures – These may be positive in as many as 50% of S aureus infections, though they are very poor at detecting Neisseria gonorrhoeae (~10% of cases prove positive)
-
Urethral, cervical, pharyngeal, and rectal cultures – These have a much higher yield for N gonorrhoeae than blood cultures do
-
Synovial fluid analysis [33] (see Table 1 below) – This should include Gram stain, culture, cell counts, and crystal analysis
Table 1. Synovial Fluid Classification* (Open Table in a new window)
Quality |
Reference Range |
Noninflammatory |
Inflammatory |
Septic |
Volume |
< 3.5 mL |
>3.5 mL |
>3.5 mL |
>3.5 mL |
Viscosity |
High |
High |
Low |
Variable |
Color |
Clear |
Straw-yellow |
Yellow |
Variable |
Clarity |
Transparent |
Transparent |
Translucent |
Opaque |
WBCs |
< 200/µL |
200-2000/µL |
2000-75,000/µL |
Often >100,000/µL |
PMNs |
< 25% |
< 25% |
>50% |
>75% |
Culture result |
Negative |
Negative |
Negative |
Often positive† |
Mucin clot |
Firm |
Firm |
Friable |
Friable |
Glucose |
~Blood |
~Blood |
Decreased |
Very decreased |
PMN = polymorphonuclear leukocyte; WBC = white blood cell. *Modified from Schumacher. [33] †Synovial fluid culture results are positive in 85-95% of nongonococcal arthritis cases and in ~25% of gonococcal arthritis cases. |
||||
Imaging studies
Plain radiography may be performed with anteroposterior and lateral views. Findings are often normal. Radiography may be particularly helpful when considering hip involvement in young children.
Look for soft-tissue swelling around the joint, widening of the joint space, and displacement of tissue planes. In later stages of progression, look for bony erosions (see the first image below) and joint-space narrowing (see the second image below).
 Anteroposterior view of knee demonstrates patchy demineralization of tibia and femur and joint-space narrowing caused by tuberculoid infection of joint.
Anteroposterior view of knee demonstrates patchy demineralization of tibia and femur and joint-space narrowing caused by tuberculoid infection of joint.
Ultrasonography (US) is very sensitive in detecting joint effusions generated by septic arthritis. [34] It can be used to define the extent of septic arthritis and help guide treatment. In addition, US helps differentiate septic arthritis from other conditions (eg, soft-tissue abscesses, tenosynovitis) for which treatment may differ.
Several authors recommend including magnetic resonance imaging (MRI) in the diagnostic evaluation to rule out the presence of periarticular abscess (see the first image below), osteomyelitis (see the second image below), and septic bursitis, all of which may complicate conservative treatment and necessitate operative debridement.
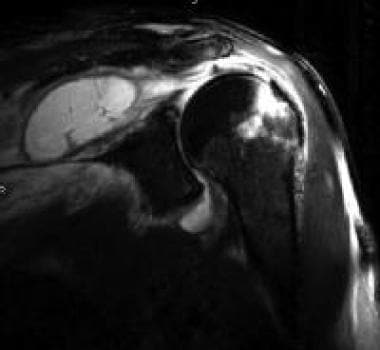 Septic arthritis with associated soft tissue abscess. Coronal T2-weighted fat-saturated magnetic resonance imaging of shoulder demonstrates joint effusion, bone marrow edema, and marked adjacent soft tissue inflammation with fluid collection in infraspinatus.
Septic arthritis with associated soft tissue abscess. Coronal T2-weighted fat-saturated magnetic resonance imaging of shoulder demonstrates joint effusion, bone marrow edema, and marked adjacent soft tissue inflammation with fluid collection in infraspinatus.
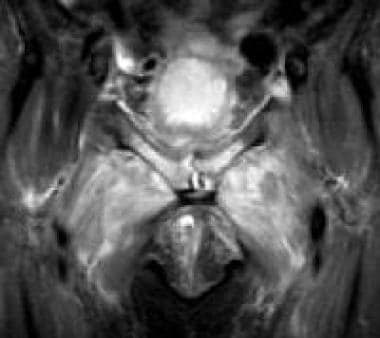 Hyperintense joint effusion and increased signal intensity in bone marrow of pubic rami shown in septic arthritis with associated osteomyelitis and inflammatory changes in soft tissues.
Hyperintense joint effusion and increased signal intensity in bone marrow of pubic rami shown in septic arthritis with associated osteomyelitis and inflammatory changes in soft tissues.
Nuclear scanning may be helpful to differentiate transient synovitis from septic arthritis.
Needle aspiration
In the vast majority of cases, needle aspiration may be the best initial diagnostic and therapeutic procedure. It may allow thorough decompression of the joint, and it can be repeated serially to achieve relief of symptoms, decrease joint effusion, and clear bacteria and synovial white blood cells (WBCs). However, needle aspiration is a poor choice in joints with loculations.
-
Anteroposterior view of knee demonstrates patchy demineralization of tibia and femur and joint-space narrowing caused by tuberculoid infection of joint.
-
Hyperintense joint effusion and increased signal intensity in bone marrow of pubic rami shown in septic arthritis with associated osteomyelitis and inflammatory changes in soft tissues.
-
Anteroposterior view of shoulder demonstrates subchondral erosions and sclerosis in humeral head.
-
Septic arthritis with associated soft tissue abscess. Coronal T2-weighted fat-saturated magnetic resonance imaging of shoulder demonstrates joint effusion, bone marrow edema, and marked adjacent soft tissue inflammation with fluid collection in infraspinatus.










