Background
Atrioventricular nodal reentry tachycardia (AVNRT) is the most common type of reentrant supraventricular tachycardia (SVT). The substrate for AVNRT is the presence of dual AV nodal pathways that are bounded by Koch’s triangle – generally a slow and a fast pathway but sometimes two slow pathways. [1, 2] (See Etiology.)
Because of the abrupt onset and termination of the reentrant SVT, the nonspecific term paroxysmal supraventricular tachycardia (or even the misleading term paroxysmal atrial tachycardia [PAT]) has been used to refer to these tachyarrhythmias. With improved knowledge of the electrophysiology of reentrant SVT, greater specificity in nomenclature, based on the mechanism of reentry, has been possible. Such improved classification aids in the choice of appropriate therapies. (See Etiology, Prognosis, Treatment, and Medication.)
AVNRT is usually well tolerated, often occurring in patients with no structural heart disease. [3] (See Prognosis, Presentation, and Workup.)
Patient education
Patients should be instructed on vagal maneuvers (Valsalva, diving reflex). These are used to try to terminate an episode of AVNRT. Patients with hemodynamic compromise or syncope should be instructed on avoiding activities that could be dangerous to them or to others (eg, driving, swimming) while the risk of an episode remains. Ablation obviates the need for long-term restriction.
For patient education information, see the Heart Health Center, as well as Supraventricular Tachycardia (SVT, PSVT).
Etiology
The substrate for atrioventricular (AV) nodal reentry tachycardia (AVNRT) is anatomic. AVNRT occurs in young, healthy patients but also in those with chronic heart disease.
In patients with AVNRT, two pathways connect into the AV node and help form part of the reentrant circuit. [4] In the majority of patients with AVNRT, antegrade conduction occurs over the slow pathway, and retrograde conduction occurs over the fast pathway during AVNRT. (See the image below.)
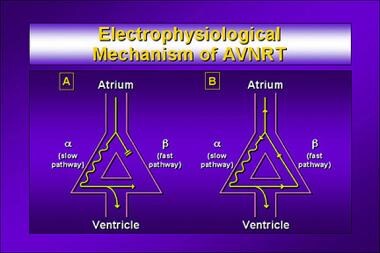 Atrioventricular Nodal Reentry Tachycardia. Electrophysiologic mechanism of atrioventricular nodal reentry tachycardia (AVNRT).
Atrioventricular Nodal Reentry Tachycardia. Electrophysiologic mechanism of atrioventricular nodal reentry tachycardia (AVNRT).
In most patients with AVNRT, the tachycardia is initiated when an atrial premature complex is blocked in the fast pathway but can conduct via the slow pathway. Although many patients may have a dual pathway physiology, for AVNRT to occur, the fast pathway must have a longer refractory period antegrade than the slow conducting pathway.
In approximately 10% of patients, AVNRT is induced by premature ventricular stimulation. In addition to the typical mechanism of AV nodal reentry described above, atypical AV nodal reentry can occur in the opposite direction, with antegrade conduction in the fast pathway and retrograde conduction in the slow pathway. Less commonly, the reentrant circuit can be over two slow pathways, the so-called slow-slow AV nodal reentry. (See the images below.)
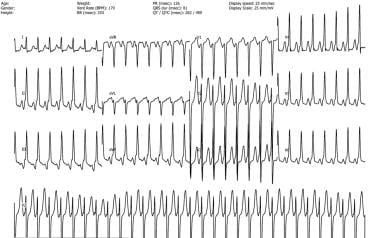 Atrioventricular Nodal Reentry Tachycardia. Atypical atrioventricular nodal (AV) reentry tachycardia. Often, an inverted P wave is seen just before the QRS complex in leads II, III, aVF. This represents activation of the posterior septum due to antegrade conduction via the fast pathway and retrograde conduction via the slow pathway of the AV node.
Atrioventricular Nodal Reentry Tachycardia. Atypical atrioventricular nodal (AV) reentry tachycardia. Often, an inverted P wave is seen just before the QRS complex in leads II, III, aVF. This represents activation of the posterior septum due to antegrade conduction via the fast pathway and retrograde conduction via the slow pathway of the AV node.
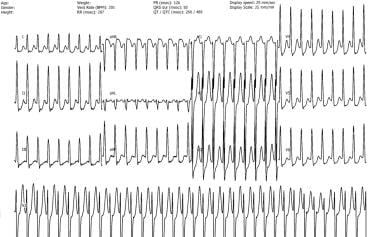 Atrioventricular Nodal Reentry Tachycardia. Typical atrioventricular nodal (AV) reentry tachycardia. In this electrocardiogram, the P wave appears immediately after or just within the QRS complex. Often a “pseudo R wave" is seen in lead V1 and a “pseudo S wave" in leads II, III, aVF. The retrograde P wave represents retrograde activation via the fast pathway, which is anterior septal and superior to the AV node.
Atrioventricular Nodal Reentry Tachycardia. Typical atrioventricular nodal (AV) reentry tachycardia. In this electrocardiogram, the P wave appears immediately after or just within the QRS complex. Often a “pseudo R wave" is seen in lead V1 and a “pseudo S wave" in leads II, III, aVF. The retrograde P wave represents retrograde activation via the fast pathway, which is anterior septal and superior to the AV node.
Epidemiology
In the United States, atrioventricular nodal reentry tachycardia (AVNRT) occurs in 60% of patients (with a female predominance) presenting with paroxysmal supraventricular tachycardia (SVT), the other major types being bypass-mediated tachycardias and atrial tachycardias. [5] SVT has a prevalence of 2.25 cases per 1000 in the general population and an incidence of 35 per 100,000 patients. [6] Internationally, the occurrence of AVNRT is similar to that in the United States.
AVNRT may occur in persons of any age. It is common in young adults, but some patients do not present until their seventh or eighth decade or later.
Prognosis
The prognosis for patients with atrioventricular nodal reentry tachycardia (AVNRT) is usually good in the absence of structural heart disease. Most patients respond acutely to vagal maneuvers or adenosine and long term to medications to prevent recurrence or to radiofrequency ablation, which is approximately 95% curative and has a low risk of complications. It is the preferred method of treatment for most patients.
Complications of AVNRT include hemodynamic compromise, congestive heart failure, syncope, tachycardia-induced angina, cardiomyopathy, myocardial ischemia, and myocardial infarction.
-
Atrioventricular Nodal Reentry Tachycardia. Electrophysiologic mechanism of atrioventricular nodal reentry tachycardia (AVNRT).
-
Atrioventricular Nodal Reentry Tachycardia. Atypical atrioventricular nodal (AV) reentry tachycardia. Often, an inverted P wave is seen just before the QRS complex in leads II, III, aVF. This represents activation of the posterior septum due to antegrade conduction via the fast pathway and retrograde conduction via the slow pathway of the AV node.
-
Atrioventricular Nodal Reentry Tachycardia. Typical atrioventricular nodal (AV) reentry tachycardia. In this electrocardiogram, the P wave appears immediately after or just within the QRS complex. Often a “pseudo R wave" is seen in lead V1 and a “pseudo S wave" in leads II, III, aVF. The retrograde P wave represents retrograde activation via the fast pathway, which is anterior septal and superior to the AV node.







