Laboratory Studies
Results of routine laboratory studies are usually normal, although thrombocytopenia can result from sequestration and destruction of platelets in large lesions.
Hypofibrinogenemia has been attributed to intratumoral fibrinolysis.
Normal alpha-fetoprotein, CA 19-9, and carcinogenic embryonic antigen (CEA) levels bolster the clinical suspicion of a benign hepatic mass lesion.
Imaging Studies
The modalities used to aid in the diagnosis of hepatic hemangiomas include ultrasonography, dynamic contrast-enhanced computed tomography (CT) scanning, nuclear medicine studies using technetium-99m (99m Tc)–labeled red blood cells (RBCs), magnetic resonance imaging (MRI), hepatic arteriography, and digital subtraction angiography (DSA).
Ultrasonography
Ultrasonography is the most commonly used initial diagnostic tool. It is widely available and inexpensive. Hepatic hemangiomas usually are echogenic, but their sonographic appearance is variable and nonspecific. See the images below.
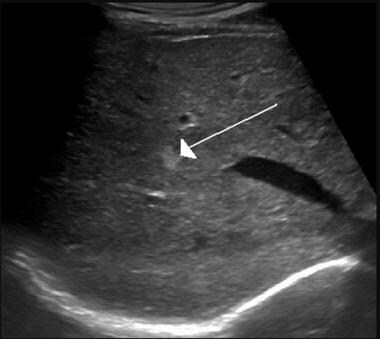 Hemangioma of the liver as seen on ultrasound. Courtesy of Wikimedia Commons/James Heilman, MD (https://commons.wikimedia.org/wiki/File:Hemangiomaliver.PNG).
Hemangioma of the liver as seen on ultrasound. Courtesy of Wikimedia Commons/James Heilman, MD (https://commons.wikimedia.org/wiki/File:Hemangiomaliver.PNG).
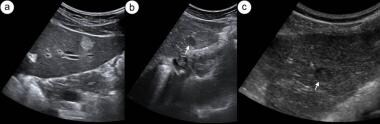 Hepatic hemangioma. (a): Transverse sonogram of left lobe of liver presenting a typical hyperechogenic hemangioma. (b) and (c): Two different hypoechogenic liver lesions suspected to be atypical hemangioma, subsequently confirmed by computed tomography scanning. Courtesy of BMC Gastroenterology (https://bmcgastroenterol.biomedcentral.com/articles/10.1186/1471-230X-11-43).
Hepatic hemangioma. (a): Transverse sonogram of left lobe of liver presenting a typical hyperechogenic hemangioma. (b) and (c): Two different hypoechogenic liver lesions suspected to be atypical hemangioma, subsequently confirmed by computed tomography scanning. Courtesy of BMC Gastroenterology (https://bmcgastroenterol.biomedcentral.com/articles/10.1186/1471-230X-11-43).
The addition of color Doppler to routine ultrasonography provides qualitative and quantitative data and increases the sensitivity and specificity of the test. Serial ultrasonographic examinations can be used to monitor any increase in the size of the hemangioma over time.
The use of microbubble-enhanced ultrasonography has been studied. Lesions show peripheral puddles and pools of enhancement that expand in a centripetal pattern (progressing inward toward the center) during the portal venous phase of enhancement. [27] With delayed imaging, the lesion may completely "fill in." [28] However, complete enhancement might not occur in large lesions where central thrombosis or scarring may be present.
In one study, the addition of a contrast agent to routine ultrasonography improved the sensitivity from 78% to 100% and specificity from 23% to 92%. [29] Unfortunately, contrast-enhanced ultrasonography is available at relatively few medical centers. [30]
In general, the finding on ultrasonography of a suspected hemangioma should be diagnostically integrated with computed tomography (CT) scanning or magnetic resonance imaging (MRI) to ensure a correct diagnosis.
Computed tomography scanning
Dynamic contrast-enhanced CT scanning is preferred to routine CT scanning. When requesting a CT scan to investigate a liver mass, the physician should inform the radiologist about the need for nonenhanced, arterial, portal venous, and delayed imaging (the so-called triple-phase CT scanning with delayed imaging).
First, the liver is imaged by CT scanning before the administration of intravenous contrast. The next series of images is obtained about 30 seconds after the injection of contrast, at the time that contrast is entering the liver via the hepatic artery. Portal venous imaging occurs 60 seconds later, as contrast is returning to the liver from the mesenteric veins via the portal vein. Finally, delayed images are obtained several minutes later.
Hepatic hemangiomas are typically hypodense on precontrast imaging. In the arterial phase, there may be enhancement of the peripheral portions of the lesion. There may be ring enhancement or globular enhancement. The center of the lesion typically remains hypodense.
In the portal venous phase and in delayed images, contrast enhancement progresses centripetally. The center of the lesion may only become hyperdense in delayed images.
See the image below.
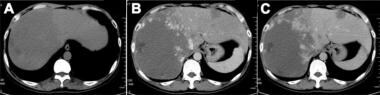 Hepatic hemangioma. (A) On plain computed tomography (CT) scan, an oval, low-density lesion with clear boundaries and central liquefactive necrosis is seen). (B) and (C): CT-enhanced scans show nodular enhancement at the edges of the lesion during the early arterial phase, and a higher density than the normal liver, appearing as the “fast out, slow in” sign. Courtesy of PLoS One (https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0135158).
Hepatic hemangioma. (A) On plain computed tomography (CT) scan, an oval, low-density lesion with clear boundaries and central liquefactive necrosis is seen). (B) and (C): CT-enhanced scans show nodular enhancement at the edges of the lesion during the early arterial phase, and a higher density than the normal liver, appearing as the “fast out, slow in” sign. Courtesy of PLoS One (https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0135158).
Magnetic resonance imaging
MRI is highly sensitive and specific for the diagnosis of hepatic hemangioma. [31, 32] Typically, hemangiomas have low signal intensity on T1-weighted images and high signal intensity on T2-weighted images (see the image below). When gadolinium is used as an intravenous contrast agent, hemangiomas enhance in a fashion similar to that seen on dynamic CT scanning. Typically, hemangiomas follow the signal intensity of blood. However, hemangiomas smaller than 2 cm may exhibit homogeneous enhancement in late arterial-phase imaging and can be mistaken for hepatocellular carcinoma or a hypervascular metastasis. [33] The sensitivity for detection of hepatic hemangioma is upwards of 90%. [34]
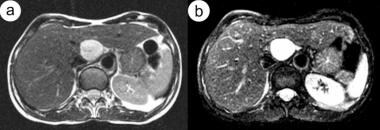 Hepatic hemangioma. Moderately (a) and heavily (b) T2-weighted magnetic resonance images show typical bright lesions. Courtesy of BMC Gastroenterology https://bmcgastroenterol.biomedcentral.com/articles/10.1186/1471-230X-11-43).
Hepatic hemangioma. Moderately (a) and heavily (b) T2-weighted magnetic resonance images show typical bright lesions. Courtesy of BMC Gastroenterology https://bmcgastroenterol.biomedcentral.com/articles/10.1186/1471-230X-11-43).
Giant cavernous hemangiomas (ie, >5 cm in diameter) may exhibit internal fluid levels on MRI and CT scan images. [35] This finding is attributed to the separation of the blood cells and serous fluid because of extremely slow blood flow through the tumor.
In the setting of hepatic fibrosis and cirrhosis, MRI features of hepatic hemangioma appear similar to those of normal livers. [36]
In the authors' opinion, MRI with arterial phase and delayed contrast is the test of choice for investigating a liver mass of unclear origin. This is particularly the case when hepatic hemangioma is suspected.
Nuclear medicine studies
Planar scintigraphic studies using Tc-99m pertechnetate-labeled red blood cells have been used for many years to help in diagnosing hepatic hemangiomas. Sensitivity for hemangiomas greater than 2 cm in diameter is reported to be as high as 82%, with a specificity of up to 100%. [37]
Single-photon emission computerized tomography (SPECT) scanning using Tc-99m pertechnetate-labeled RBCs is more accurate than planar imaging in helping to diagnose hepatic hemangioma. [38] However, it is not available at all medical centers.
SPECT is more specific than MRI, but it is less sensitive. This is particularly true for lesions near the heart or major blood vessels. [38]
Some investigators consider SPECT with 99mTc-labeled RBCs to be the criterion standard to establish a diagnosis of hepatic hemangiomas. However, the test may still miss some lesions. Also, pedunculated giant liver hemangiomas have been reported to mimic hypervascular gastric tumors on SPECT. [39]
Arteriography
The diagnostic accuracy of noninvasive tests has obviated the need for hepatic arteriography in most cases. However, this invasive modality still may be useful in helping to diagnose some hepatic hemangiomas.
Branches of the hepatic artery may be displaced and crowded together or stretched around the lesion, with normal vascular tapering.
Hemangiomas are characterized by the early opacification of irregular areas or lakes, with persistence of contrast in these areas long after arterial emptying. The hemangioma may appear as a ring or C-shaped lesion with an avascular center.
Accuracy of imaging studies
The diagnostic capabilities of ultrasonography, Doppler color ultrasonography, dynamic CT scanning, and MRI were compared in a retrospective study of 27 patients with 35 hemangiomas. [40]
Sensitivities reported in the study were as follows [40] :
-
Ultrasonography – 46% sensitivity
-
Combined B-mode and color Doppler ultrasonography – 69% sensitivity
-
Contrast-enhanced CT scanning - 66% sensitivity
-
T2-weighted MRI - 96% sensitivity
-
Gadolinium-enhanced MRI combined with dynamic CT scanning - 100% sensitivity
Hepatic angiosarcoma is a rare tumor that tends to grow rapidly. Although hepatic angiosarcoma is classically associated with risk factors, including exposure to Thorotrast, vinyl chloride, or arsenic, many cases have occurred in which no discrete risk factor has been identified. Unfortunately, hepatic angiosarcoma may occasionally be mistaken for hepatic hemangioma on MRI, and vice versa. In the case of a suspected hemangioma with an atypical enhancement pattern, it is reasonable to perform a follow-up radiologic study in a few months to rule out rapid interval growth of the lesion. [41, 42]
Features of angiosarcoma on multiphasic CT scanning and MRI include the following [43] :
-
Rapidly progressive multifocal tumors
-
Arterial-phase foci of hypervascular enhancement without washout
-
Hypervascular foci with progressive expansion followed by blood pooling on multiphasic imaging
-
Enhancement pattern resembling that of cavernous hemangiomas or showing a "reverse hemangioma" centrifugal pattern
Imaging of hemangiomas less than 2 cm
Diagnostic accuracy diminishes for all imaging modalities when assessing a liver lesion that is less than 2 cm in diameter.
MRI and 99mTc-RBC SPECT are the most accurate radiologic studies to establish the diagnosis of a small hepatic hemangioma.
The authors continue to regard MRI as the diagnostic test of choice for hepatic hemangioma at most centers. Nuclear medicine studies may be used to confirm the diagnosis when a probable hemangioma is detected on ultrasonography. Nuclear medicine studies may also help to clarify the nature of a lesion when the diagnosis is equivocal on CT scanning or MRI.
Procedures
Liver biopsy
Percutaneous biopsy of a hepatic hemangioma carries an increased risk of hemorrhage. Liver biopsy is contraindicated in most circumstances where a hemangioma is high in the differential diagnosis of a hepatic mass.
Liver biopsy can help provide an unequivocal histologic diagnosis and may shorten the diagnostic workup. One study reported the safe performance of ultrasonographically guided 18-gauge core needle biopsy in 51 hemangiomas ranging in size from 7-114 mm. [44] However, the authors do not recommend its performance.
Some authorities contend that either a percutaneous liver biopsy or laparoscopic liver biopsy may be reasonable to perform in cases where a small liver lesion must be differentiated from hepatocellular carcinoma. However, since 2001, hepatologists and surgeons have been increasingly resistant to include liver biopsy in the diagnostic workup of suspected hepatocellular carcinoma. The diagnosis of most hepatocellular carcinomas can be made by using a combination of CT scanning and MRI. [45] Liver biopsy is only used when radiologic study results and alpha fetoprotein testing are equivocal.
Histologic Findings
Microscopically, hemangiomas are composed of cavernous vascular channels. The channels are lined by single layers of flattened endothelium and are separated by fibrous septa. These vascular spaces may contain thrombin, calcifications, or prominent scarring with hyalinization (sclerosed hemangioma). Phleboliths are rare. Malignant transformation has not been reported.
Pathology
Hemangiomas are usually solitary. Multiple and diffuse hepatic lesions are seen infrequently. Sizes range from 2 mm to more than 20 cm. On gross examination, these lesions often appear as having a flat surface or as bulging subcapsular lesions.
Lesions are reddish-blue and well demarcated from surrounding tissue. Large tumors may become pedunculated.
Histologically, the tumor is thin walled. Its vascular spaces are lined by a single layer of endothelial cells that are separated by fibrous septa. [46, 47]
-
Hemangioma of the liver as seen on ultrasound. Courtesy of Wikimedia Commons/James Heilman, MD (https://commons.wikimedia.org/wiki/File:Hemangiomaliver.PNG).
-
Hepatic hemangioma. (a): Transverse sonogram of left lobe of liver presenting a typical hyperechogenic hemangioma. (b) and (c): Two different hypoechogenic liver lesions suspected to be atypical hemangioma, subsequently confirmed by computed tomography scanning. Courtesy of BMC Gastroenterology (https://bmcgastroenterol.biomedcentral.com/articles/10.1186/1471-230X-11-43).
-
Hepatic hemangioma. Moderately (a) and heavily (b) T2-weighted magnetic resonance images show typical bright lesions. Courtesy of BMC Gastroenterology https://bmcgastroenterol.biomedcentral.com/articles/10.1186/1471-230X-11-43).
-
Hepatic hemangioma. (A) On plain computed tomography (CT) scan, an oval, low-density lesion with clear boundaries and central liquefactive necrosis is seen). (B) and (C): CT-enhanced scans show nodular enhancement at the edges of the lesion during the early arterial phase, and a higher density than the normal liver, appearing as the “fast out, slow in” sign. Courtesy of PLoS One (https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0135158).








