Overview
Choriocarcinoma of the testis is a germ cell tumor that is rarely identified in its pure form; it is more often seen as a component of a nonseminomatous germ cell tumor. [1, 2] Choriocarcinoma is defined by the presence of 2 cellular components, both syncytiotrophoblasts—which often show bizarre, atypical nuclei—and cytotrophoblasts, arranged in solid nests and sheets. Intermediate trophoblasts are also often present. [3] See the image below.
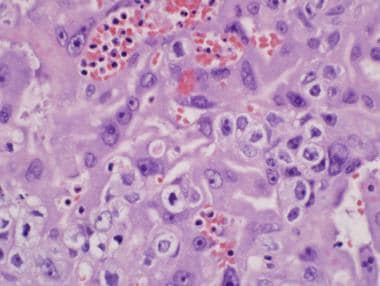
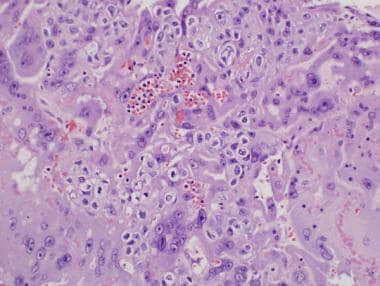
 In this image, both cytotrophoblasts and syncytiotrophoblasts are admixed with rare mitotic figures identified. 100× view.
In this image, both cytotrophoblasts and syncytiotrophoblasts are admixed with rare mitotic figures identified. 100× view.
Choriocarcinoma is extremely rare in its pure form, constituting less than 1% of testicular tumors. [4] More frequently, this tumor is seen as a component of mixed germ cell tumors in approximately 8-10% of such cases. [5] The overall incidence of choriocarcinoma of the testis is approximately 0.8 cases per year per 100,000 male population in countries with the highest frequency of testicular cancer. [6] This tumor most is often found in males between the ages of 15 and 30 years but may be seen from puberty to old age. [7]
Etiology and Location
Although there is no known specific etiology of choriocarcinoma, germ cell tumors in general are believed to originate from malignant intratubular germ cells. Choriocarcinoma occurs within the testicular parenchyma, with no predilection to a particular site. Vascular invasion is common and the high metastatic potential of this tumor allows for it to travel throughout the body.
Clinical Features
Choriocarcinoma of the testis presents most commonly in 15- to 30-year-old patients with hormonal symptoms such as gynecomastia and an elevated human chorionic gonadotropin (hCG) level. The hCG level is elevated due to an increase in production by the syncytiotrophoblastic component of the tumor. Other features may include mild testicular enlargement and evidence of metastatic disease due to the high incidence of vascular invasion. [5]
The most common sites of metastasis include the lungs, retroperitoneum, gastrointestinal tract, liver, and central nervous system. [8] Oftentimes, the metastatic tumor is discovered first only to unveil the primary tumor in the testis afterward. This occurs because of the rapid malignant potential of this tumor. In certain cases in which metastatic disease is uncovered, the primary tumor may no longer be visible and only a scar is seen within the testis. Thyrotoxicosis is a rare symptom that occurs due to the structural similarities between hCG and thyroid-stimulating hormone (TSH).
Differential Diagnosis
The following conditions should be considered in the differential diagnosis of testicular choriocarcinomas:
Tumor Imaging
Imaging plays a vital role in the assessment of germ cell tumors in general. Tumor bulk, sites of metastases, and response to treatment can all be assessed by various imaging techniques. The most commonly used imaging modality is computed tomography (CT) scanning, but plain film radiography, ultrasonography, and magnetic resonance imaging (MRI) are used as well. [9]
Primary testicular disease often shows a hypoechoic pattern on ultrasonograms. CT scanning has been shown to be the most sensitive method of assessing metastatic disease within the thorax, abdomen, and pelvis.
Positron emission tomography (PET) scanning is an emerging diagnostic imaging technique used to assess for metastatic disease. However, its optimal role is yet to be agreed upon. [9]
Gross and Microscopic Findings
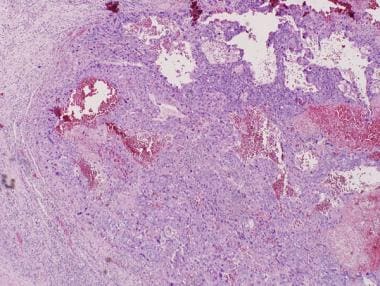
Typically, the testis is normal in size but may show mild enlargement. The tumor displays abundant hemorrhage and necrosis, usually with poorly defined, grayish viable tissue at the periphery. [5]
Histologically, choriocarcinoma is composed of syncytiotrophoblasts and cytotrophoblasts, of which the presence of both is required for diagnosis. These cells are typically intermingled together in solid nests or sheets, occasionally in a villuslike arrangement. [5, 7] The syncytiotrophoblasts are large, multinucleated cells with vacuolization and amphophilic cytoplasm. They typically have multiple large, pleomorphic, smudged-appearing nuclei. The cytotrophoblasts are small to medium in size, with clear cytoplasm and mild to moderate nuclear pleomorphism. Mitotic activity is oftentimes abundant. The background shows extensive hemorrhage and necrosis. See the following images.
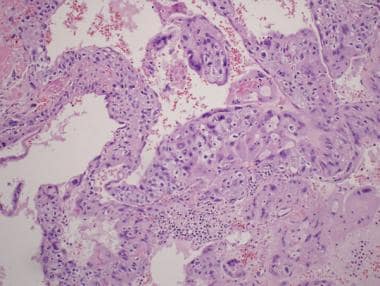
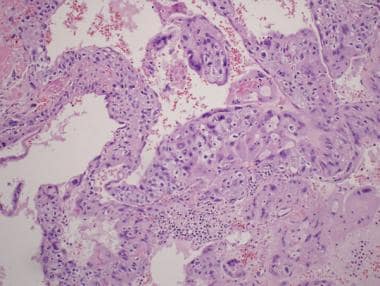
 Cytotrophoblasts and syncytiotrophoblasts are intermingled amongst a hemorrhagic background. 40× view.
Cytotrophoblasts and syncytiotrophoblasts are intermingled amongst a hemorrhagic background. 40× view.
 In this image, both cytotrophoblasts and syncytiotrophoblasts are admixed with rare mitotic figures identified. 100× view.
In this image, both cytotrophoblasts and syncytiotrophoblasts are admixed with rare mitotic figures identified. 100× view.
Cytotrophoblasts may be indistinct, and it is often difficult to discern them from other seminoma or embryonal carcinoma cells, aside from their close concurrence with syncytiotrophoblasts. Commonly, the syncytiotrophoblasts surround the cytotrophoblasts creating a "cap." [5] See the images below.
 In this image, the syncytiotrophoblasts are large, multinucleated cells with vacuolization and amphophilic cytoplasm. They typically have multiple large, pleomorphic, smudged-appearing nuclei. The cytotrophoblasts are small to medium in size, with clear cytoplasm and mild to moderate nuclear pleomorphism. 200× view.
In this image, the syncytiotrophoblasts are large, multinucleated cells with vacuolization and amphophilic cytoplasm. They typically have multiple large, pleomorphic, smudged-appearing nuclei. The cytotrophoblasts are small to medium in size, with clear cytoplasm and mild to moderate nuclear pleomorphism. 200× view.
Rare variants of choriocarcinoma have been described. Two of these are grouped under the term choriocarcinomalike lesion (CCLL). [10] The first variant shows an unusual proliferation of teratomatous epithelium and is known as teratomatous CCLL. The second variant is a cystic, nonbiphasic form.
Another variant is known as placental-site trophoblastic tumor (PSTT). This is a well-known entity within the female reproductive tract. However, in males, only 2 cases have been reported. [11] The first case involved an adult male patient whose tumor showed a predominant component of cytotrophoblastic nodules with only rare syncytiotrophoblastic cells. The second case involved a 16-month-old boy whose tumor consisted of only mononuclear, intermediate trophoblast cells and was identical to the more common PSTT of the uterus.
Very rarely, a monophasic variant has been described, in which the syncytiotrophoblasts are very infrequent, and the tumor is composed almost exclusively of cytotrophoblasts. [11, 12]
A single case of choriocarcinoma was reported with an angiosarcomatous component. This phenomenon, although rare, portends a poor clinical outcome with a decreased life expectancy. [13]
These infrequent variants highlight the importance that trophoblastic tumors other than classic choriocarcinoma can occur in the testis.
Immunohistochemistry
Syncytiotrophoblasts are positive for human chorionic gonadotropin (hCG), human placental lactogen (HPL), and pregnancy-specific beta-1 glycoprotein (SP1), whereas cytotrophoblasts are negative for all of these markers. [14] Low–molecular-weight keratins such as Cam 5.2 are positive in both syncytiotrophoblasts and cytotrophoblasts. Placental alkaline phosphatase (PLAP) is positive in about 50% of choriocarcinomas, whereas carcinoembryonic antigen (CEA) is positive in about 25%. [15, 16] Vimentin is negative. Inhibin is typically positive in syncytiotrophoblasts and negative in cytotrophoblasts. [17] Immunohistochemical stains may also play an important role in differentiating choriocarcinoma from other germ cell tumors with syncytiotrophoblastic cells. OCT 3/4 will be negative in syncytiotrophoblastic components of choriocarcinoma but positive in those of seminoma or embryonal carcinoma. [18]
Molecular/Genetic Features
Choriocarcinoma of the testis shares similar genetic features of other malignant germ cell testicular neoplasms. The most recent developments show that the most common genetic abnormality is the formation of an isochromosome 12p [i(12p)]. The i(12p) occurs in both primary and metastatic disease sites. [19] Currently, no specific gene on i(12p) involved with the development of germ cell tumors is known.
Tumor Spread and Staging
Choriocarcinoma spreads through both lymphatic and hematogenous routes. The most commonly involved lymph nodes are the retroperitoneal. Other common sites of involvement include the lungs, liver, gastrointestinal tract, spleen, brain, and adrenal glands.
Tumor staging of choriocarcinoma is similar to that of all testicular germ cell neoplasms. It is typically determined after the orchiectomy is performed and the diagnosis is made. The tumor classification is as follows [20] :
-
The primary tumor is classified as pT1 if it is limited to the testis and does not invade the tunica vaginalis.
-
The tumor is classified as pT2 if it shows vascular or lymphatic invasion or it invades the tunica vaginalis.
-
The tumor is classified pT3 if it invades the spermatic cord.
-
The tumor is classified as pT4 if it invades the scrotum.
Regional lymph node metastasis is staged depending on the size and number of metastases, as follows [20] :
-
Stage N0 is reserved for no metastases.
-
Stage N1 is refers to a metastasis within any number of lymph node with the mass(es) measuring no greater than 2 cm in its greatest dimension.
-
Stage N2 refers to a metastasis within any number of lymph node with the mass(es) measuring greater than 2 but less than 5 cm in its greatest dimension.
-
Stage N3 refers to a lymph node metastasis greater than 5 cm in its greatest dimension.
Distant metastases are staged based on their location within the body, as follows [20] :
-
Stage M0 is reserved for no distant metastasis.
-
Stage M1a is refers to a nonregional nodal or pulmonary metastasis.
-
Stage M1b refers to a distant metastasis other than to nonregional lymph nodes or lungs.
Serum tumor markers including lactate dehydrogenase (LDH), human chorionic gonadotropin (hCG), and alpha-fetoprotein (AFP) also play a role in the staging of testicular tumors.
Prognosis and Predictive Factors
The natural history of choriocarcinoma is similar to the adult type of embryonal carcinoma. It presents with advanced-stage disease in a majority of cases. The ability of choriocarcinoma to rapidly invade blood vessels allows for rapid dissemination of the tumor. In addition, increasing levels of human chorionic gonadotropin (hCG) correspond to a worse prognosis. [6] There are currently no predictive factors for this tumor.
-
In this image, both cytotrophoblasts and syncytiotrophoblasts are admixed with rare mitotic figures identified. 100× view.
-
In this image, the syncytiotrophoblasts are large, multinucleated cells with vacuolization and amphophilic cytoplasm. They typically have multiple large, pleomorphic, smudged-appearing nuclei. The cytotrophoblasts are small to medium in size, with clear cytoplasm and mild to moderate nuclear pleomorphism. 200× view.
-
A high-power view of the previous image. 400× view.
-
Cytotrophoblasts and syncytiotrophoblasts are intermingled amongst a hemorrhagic background. 40× view.