Approach Considerations
In recent years, laboratory evaluation of trauma patients has been a matter of significant discussion. Commonly recommended studies include serum glucose, complete blood count (CBC), serum chemistries, serum amylase, urinalysis, coagulation studies, blood typing and cross-matching, arterial blood gases (ABGs), blood ethanol, urine drug screens, and a urine pregnancy test (for females of childbearing age).
Serum electrolyte values, creatinine level, and glucose values are often obtained for reference, but typically they have little or no value in the initial management period.
Aggressive radiographic and surgical investigation is indicated in patients with persistent hyperamylasemia or hyperlipasemia, conditions that suggest significant intra-abdominal injury.
All patients should have their tetanus immunization history reviewed. If it is not current, prophylaxis should be given.
The most important initial concern in the evaluation of a patient with blunt abdominal trauma is an assessment of hemodynamic stability. In the hemodynamically unstable patient, a rapid evaluation must be made regarding the presence of hemoperitoneum. This can be accomplished by means of diagnostic peritoneal lavage (DPL) or the focused assessment with sonography for trauma (FAST). Radiographic studies of the abdomen are indicated in stable patients when the physical examination findings are inconclusive.
A prospective, observational study by Kwok et al indicates that in children with blunt torso trauma, plain anteroposterior pelvic radiographs have only 78% sensitivity in detecting pelvic fracture or dislocation. The investigators found that such radiographic examination performed in the emergency department detected pelvic fracture or dislocation in only 297 of 382 patients known to have these injuries. The study also indicated that computed tomography (CT) scanning has a much higher sensitivity in such cases. Eighty four of the 85 patients whose injuries were not detected by radiography underwent CT scanning, which detected fracture or dislocation in 82 of them (98% sensitivity). The investigators stated, however, that CT scanning should be used only if physical exam findings indicate the presence of such trauma. [13, 14]
Go to Focused Assessment with Sonography in Trauma (FAST) for complete information on this topic.
Blood Studies
Complete blood count
The presence of massive hemorrhage is usually obvious from hemodynamic parameters, and an abnormal hematocrit value merely confirms the diagnosis. Normal hemoglobin and hematocrit results do not rule out significant hemorrhage. Patients bleed whole blood. Until blood volume is replaced with crystalloid solution or hormonal effects (eg, adrenocorticotropic hormone [ACTH], aldosterone, antidiuretic hormone [ADH]) and transcapillary refill occurs, anemia may not develop.
Bedside diagnostic testing with rapid hemoglobin or hematocrit machines may quickly identify patients who have physiologically significant volume deficits and hemodilution. Reported hemoglobin from ABG measurements also may be useful in identifying anemia. Some studies have correlated a low initial hematocrit (ie, < 30%) with significant injuries.
Do not withhold transfusion in patients who have relatively normal hematocrit results (ie, >30%) but have evidence of clinical shock, serious injuries (eg, open-book pelvic fracture), or significant ongoing blood loss. Hemodynamic instability in an adult despite the administration of 2 L of fluid indicates ongoing blood loss and is an indication for immediate blood transfusion. Use platelet transfusions to treat patients with thrombocytopenia (ie, platelet count < 50,000/µL) and ongoing hemorrhage.
An elevated white blood cell (WBC) count on admission is nonspecific and does not predict the presence of a hollow viscus injury (HVI). The diagnostic value of serial WBC counts for predicting HVI within the first 24 hours after trauma is very limited. [15]
Serum electrolyte measurements
Recently, the usefulness of routine serum chemistries of trauma patients has been questioned. Most trauma victims are younger than 40 years and rarely are taking medications that may alter electrolytes (eg, diuretics, potassium replacements).
The more prudent choice when attempting to limit cost involves selective ordering of these studies. Selection should be based on the patient’s medications, the presence of concurrent nausea or vomiting, the presence of dysrhythmias, or a history of renal failure or other chronic medical problems associated with electrolyte imbalance.
Serum glucose and carbon dioxide measurements
If blood gas measurements are not routinely obtained, serum chemistries that measure serum glucose and carbon dioxide levels are indicated. Rapid bedside blood-glucose determination, obtained with a finger-stick measuring device, is important for patients with altered mental status.
Liver function tests
Liver function tests (LFTs) may be useful in the patient with blunt abdominal trauma; however, test findings may be elevated for several reasons (eg, alcohol abuse). [16] One study has shown that an aspartate aminotransferase (AST) or alanine aminotransferase (ALT) level more than 130 U corresponds with significant hepatic injury. [17] Lactate dehydrogenase (LDH) and bilirubin levels are not specific indicators of hepatic trauma.
Serum amylase or lipase measurements
The serum lipase or amylase level is neither sensitive nor specific as a marker for major pancreatic or enteric injury. Normal levels do not exclude a major pancreatic injury. Elevated levels may be caused by injuries to the head and face or by an assortment of nontraumatic causes (eg, alcohol, narcotics, various other drugs). Amylase or lipase levels may be elevated because of pancreatic ischemia caused by the systemic hypotension that accompanies trauma.
However, persistent hyperamylasemia or hyperlipasemia (eg, abnormal elevation 3-6 hours after trauma) should raise the suggestion of significant intra-abdominal injury and is an indication for aggressive radiographic and surgical investigation.
Coagulation profile
The cost-effectiveness of routine prothrombin time (PT)/activated partial thromboplastin time (aPTT) determination upon admission is questionable. PT or aPTT should be measured in patients who have a history of blood dyscrasias (eg, hemophilia), who have synthetic problems (eg, cirrhosis), or who take anticoagulant medications (eg, warfarin, heparin).
Blood typing, screening, and cross-matching
Blood from all trauma patients with suspected blunt abdominal injury should be screened and typed. If an injury is identified, this practice greatly reduces the time required for cross-matching. An initial cross-match should be performed on a minimum of 4-6 units for those patients with clear evidence of abdominal injury and hemodynamic instability. Until cross-matched blood is available, O-negative or type-specific blood should be used.
Arterial blood gas measurements
ABG values may provide important information in major trauma victims. In addition to information about oxygenation (eg, partial pressure of oxygen [PO2] and arterial oxygen saturation [SaO2]) and ventilation (partial pressure of carbon dioxide [PCO2]), this test provides valuable information regarding oxygen delivery through calculation of the alveolar-arterial (A-a) gradient. ABG determinations also report total hemoglobin more rapidly than CBCs.
Upon initial hospital admission, suspect metabolic acidemia to result from the lactic acidosis that accompanies shock. A moderate base deficit (ie, more than –5 mEq) indicates the need for aggressive resuscitation and determination of the etiology.
Attempt to improve systemic oxygen delivery by ensuring an adequate SaO2 (ie, >90%) and by acquiring volume resuscitation with crystalloid solutions and, if indicated, blood.
Drug and alcohol screening
Perform drug and alcohol screens on trauma patients who have alterations in their level of consciousness. Breath or blood testing may quantify alcohol level.
Urine Studies
Indications for diagnostic urinalysis include significant trauma to the abdomen and/or flank, gross hematuria, microscopic hematuria in the setting of hypotension, and a significant deceleration mechanism. [18]
Obtain a contrast nephrogram by utilizing intravenous pyelography (IVP) or computed tomography (CT) scanning with intravenous (IV) contrast. Gross hematuria indicates a workup that includes cystography and IVP or CT scanning of the abdomen with contrast.
Perform a urine toxicologic screen as appropriate. Obtain a serum or urine pregnancy test on all females of childbearing age.
Plain Radiography
Although their overall value in the evaluation of patients with blunt abdominal trauma is limited, plain films can demonstrate numerous findings. The chest radiograph may aid in the diagnosis of abdominal injuries such as ruptured hemidiaphragm (eg, a nasogastric tube seen in the chest) or pneumoperitoneum.
The pelvic or chest radiograph can demonstrate fractures of the thoracolumbar spine. The presence of transverse fractures of the vertebral bodies (ie, Chance fractures) suggests a higher likelihood of blunt injuries to the bowel. In addition, free intraperitoneal air, or trapped retroperitoneal air from duodenal perforation, may be seen.
Ultrasonography
The use of diagnostic ultrasonography to evaluate a patient with blunt trauma for abdominal injuries has been advocated since the 1970s. European and Asian investigators have extensive experience with this technology and are leaders in the use of ultrasound for the diagnosis of blunt abdominal trauma.
The first American report of physician-performed abdominal ultrasonography in the evaluation of blunt abdominal trauma was published in 1992 by Tso and colleagues. [19] Since then, numerous articles have been published in the United States advocating the use of ultrasound (ie, FAST) in the evaluation of the patient with blunt abdominal trauma.
Bedside ultrasonography is a rapid, portable, noninvasive, and accurate examination that can be performed by emergency clinicians and trauma surgeons to detect hemoperitoneum. In fact, in many medical centers, the FAST examination has virtually replaced DPL as the procedure of choice in the evaluation of hemodynamically unstable trauma patients.
The FAST examination is based on the assumption that all clinically significant abdominal injuries are associated with hemoperitoneum. However, the detection of free intraperitoneal fluid is based on factors such as the body habitus, injury location, presence of clotted blood, position of the patient, and amount of free fluid present.
In a patient with isolated blunt abdominal trauma and multisystem injuries, FAST performed by an experienced sonographer can rapidly identify free intraperitoneal fluid (generally appearing as a black stripe). The sensitivity for solid organ encapsulated injury is moderate in most studies. Hollow viscus injury (HVI) rarely is identified; however, free fluid may be visualized. For patients with persistent pain or tenderness or those developing peritoneal signs, FAST may be considered as a complementary measure to CT scanning, DPL, or exploration.
The minimum threshold for detecting hemoperitoneum is unknown and remains a subject of interest. Kawaguchi and colleagues found that 70 mL of blood could be detected, [20] whereas Tiling et al found that 30 mL is the minimum requirement for detection with ultrasonography. [21] They also concluded that a small anechoic stripe in the Morison pouch represents approximately 250 mL of fluid, whereas 0.5-cm and 1-cm stripes represent approximately 500 mL and 1 L of free fluid, respectively.
The current FAST examination protocol consists of 4 acoustic windows with the patient supine. These windows are pericardiac, perihepatic, perisplenic, and pelvic (known as the 4 P s). An examination is interpreted as positive if free fluid is found in any of the 4 acoustic windows and as negative if no fluid is seen. An examination is deemed indeterminate if any of the windows cannot be adequately assessed.
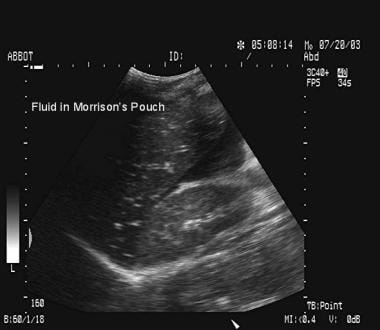
The pericardial window is obtained via a subcostal or transthoracic approach. It provides a 4-chamber view of the heart and can detect the presence of hemopericardium, which is demonstrated by the separation of the visceral and parietal pericardial layers. The perihepatic window yields views of portions of the liver, diaphragm, and right kidney. It reveals fluid in the Morison pouch (see the images below), the subphrenic space, and the right pleural space.
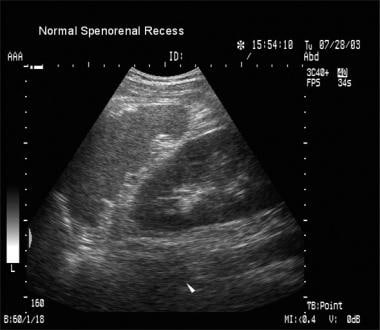
The perisplenic window provides views of the spleen and the left kidney and reveals fluid in the splenorenal recess (see the images below), the left pleural space, and the subphrenic space. The pelvic window makes use of the bladder as a sonographic window and thus is best accomplished while the patient has a full bladder. In males, free fluid is seen as an anechoic area (sonographically black) in the rectovesicular pouch or cephalad to the bladder. In females, fluid accumulates in the Douglas pouch, posterior to the uterus.
FAST’s diagnostic accuracy generally is equal to that of DPL. Studies in the United States have demonstrated the value of bedside sonography as a noninvasive approach for rapid evaluation of hemoperitoneum. The studies demonstrate a degree of operator dependence; however, some studies have shown that with a structured learning session, even novice operators can identify free intra-abdominal fluid, especially if more than 500 mL of fluid is present. Sensitivity and specificity of these studies range from 85% to 95%. [22, 23, 24, 25, 26]
As noted, FAST relies on hemoperitoneum to identify patients with injury. Chiu and colleagues, in their study of 772 patients with blunt trauma undergoing FAST scans, reported 52 patients had an abdominal injury. [27] Of the 52 patients, 15 (29%) had no hemoperitoneum on FAST or CT scan results. These findings suggest that the reliance on hemoperitoneum as the sole indicator of abdominal visceral injury limits the utility of FAST as a diagnostic screening tool in stable patients with blunt abdominal trauma.
Rozycki et al studied 1540 patients and reported that ultrasonography was the most sensitive and specific modality for the evaluation of hypotensive patients with blunt abdominal trauma (sensitivity and specificity, 100%). [26]
A randomized clinical trial by Holmes et al reported that FAST examination did not improve clinical care (use of resources, ED length of stay, missed intra-abdominal injuries, or hospital charges) in 975 hemodynamically stable children younger than 18 years of age treated for blunt torso trauma. [28]
Hemodynamically stable patients with positive FAST results may require a CT scan to better define the nature and extent of their injuries. Taking every patient with a positive FAST result to the operating room may result in an unacceptably high laparotomy rate.
Hemodynamically stable patients with negative FAST results require close observation, serial abdominal examinations, and a follow-up FAST examination. However, strongly consider performing a CT scan, especially if the patient is intoxicated or has other associated injuries.
A Cochrane Review reported that positive point-of-care sonography findings can help guide treatment decisions, however, a negative point-of-care sonography exam should not eliminate abdominal trauma injuries and should be verified with another reference test (e.g. CT), particularly in pediatric cases. [29]
Hemodynamically unstable patients with negative FAST results are a diagnostic challenge. Options include DPL, exploratory laparotomy, and, possibly, a CT scan after aggressive resuscitation.
Go to Focused Assessment with Sonography in Trauma (FAST) for complete information on this topic.
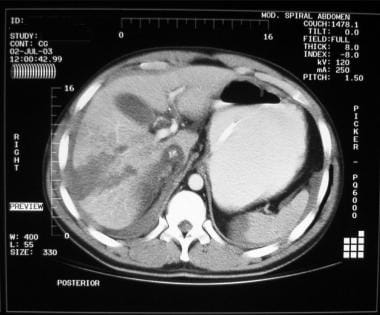
Computed Tomography
Although expensive and potentially time-consuming, CT scanning often provides the most detailed images of traumatic pathology and may assist in determination of operative intervention. [1, 2, 3, 4] CT remains the criterion standard for the detection of solid organ injuries (see the image below). In addition, a CT scan of the abdomen can reveal other associated injuries, notably vertebral and pelvic fractures and injuries in the thoracic cavity.
CT scanning, unlike DPL or FAST, has the capability to determine the source of hemorrhage (see the image below). In addition, many retroperitoneal injuries go unnoticed with DPL and FAST examinations.
Transport only hemodynamically stable patients to the CT scanner. When performing CT scans, closely and carefully monitor vital signs for clinical evidence of decompensation. Preliminary evidence suggests that a flat vena cava on CT scan is a marker for underresuscitation and may be correlated with higher mortality and hemodynamic decompensation. [30]
CT scans provide excellent imaging of the pancreas, duodenum, and genitourinary system. The images can help quantitate the amount of blood in the abdomen and can reveal individual organs with precision. The primary advantage of CT scanning is its high specificity and use for guiding nonoperative management of solid organ injuries.
Drawbacks of CT scanning relate to the need to transport the patient from the trauma resuscitation area and the additional time required to perform CT scanning compared to FAST or DPL.
In addition, CT scanning may miss injuries to the diaphragm and perforations of the gastrointestinal (GI) tract, especially when performed soon after the injury. Although some pancreatic injuries may be missed with a CT scan performed soon after trauma, virtually all are identified if the scan is repeated in 36-48 hours. For selected patients, endoscopic retrograde cholangiopancreatography (ERCP) may complement CT scanning to rule out a ductal injury.
Finally, CT scanning is relatively expensive and time consuming and requires oral or intravenous (IV) contrast, which may cause adverse reactions. The best CT imagery requires both oral and IV contrast. Some controversy has arisen over the use of oral contrast and whether the additional information it provides negates the drawbacks of increased time to administration and risk of aspiration. The value of oral contrast in diagnosing bowel injury has been debated, but no definitive answer exists at this time.
A prediction rule created by Holmes and colleagues for use in children who have suffered blunt torso trauma demonstrated a negative predictive value of 99.9% for identifying patients at very low risk for intra-abdominal injuries undergoing acute intervention and for whom CT scanning could be obviated. [31, 32] The rule consists of the following 7 patient history and physical examination findings (in descending order of importance):
-
No evidence of abdominal wall trauma or seat belt sign
-
Glasgow Coma Scale score >13 (see the Glasgow Coma Scale calculator)
-
No abdominal tenderness
-
No evidence of thoracic wall trauma
-
No complaints of abdominal pain
-
No decreased breath sounds
-
No vomiting
A prospective analysis that evaluated the use of computed tomography of the abdomen and pelvis (CTAP) in 1193 blunt trauma patients under 14 years of age reported that a negative CTAP indicates that clinically significant abdominal injury is unlikely. For the 479 asymptomatic patients with negative imaging, the median length of stay was 3 days and there were not any missed injuries. [33, 34]
Diagnostic Laparoscopy
The introduction of minimally invasive surgery has revolutionized many surgical diagnostic protocols. In the late 1980s and early 1990s, there was considerable interest in the use of laparoscopy for evaluation and management of blunt and penetrating abdominal trauma. Subsequent studies, however, revealed major limitations to this approach and cautioned against its widespread use. The most important limitation is inability to reliably identify hollow viscus and retroperitoneal injuries, even in the hands of experienced laparoscopists.
Diagnostic laparoscopy involves placing a subumbilical or subcostal trocar for the introduction of the laparoscope and creating other ports for retractors, clamps, and other tools necessary for visualization of the repair.
Diagnostic laparoscopy has been most useful in the evaluation of possible diaphragmatic injuries, especially in penetrating thoracoabdominal injuries on the left side. [35, 36, 37] In blunt trauma, it has no clear advantages over less invasive modalities such as DPL and CT scanning; furthermore, complications can result from trocar misplacement.
Diagnostic Peritoneal Lavage
The idea of evaluating the abdomen by analyzing its contents was first used in the diagnosis of acute abdominal conditions. In 1906, Salomon described the passage of a urethral catheter by means of a trocar inserted through the abdominal wall to obtain samples of peritoneal fluid with the aim of establishing the diagnosis of peritonitis from infectious agents (eg, pneumococcal or tuberculous organisms). This technique has since been refined and is now known as abdominal paracentesis.
In 1926, Neuhof and Cohen described the sampling of peritoneal fluid in cases of acute pancreatitis and blunt abdominal trauma by passing a spinal needle through the abdominal wall. [38] In 1965, Root et al reported the use of percutaneous DPL in patients who had sustained blunt abdominal trauma. [39]
DPL is used as a method of rapidly determining the presence of intraperitoneal blood. It is particularly useful if the history and abdominal examination of an unstable patient with multisystem injuries are either unreliable (eg, because of head injury, alcohol, or drug intoxication) or equivocal (eg, because of lower rib fractures, pelvic fractures, or confounding clinical examination).
DPL is also useful for patients in whom serial abdominal examinations cannot be performed (eg, those in an angiographic suite or operating room during emergency orthopedic or neurosurgical procedures). [40]
DPL is indicated for the following patients in the setting of blunt trauma:
-
Patients with a spinal cord injury
-
Those with multiple injuries and unexplained shock
-
Obtunded patients with a possible abdominal injury
-
Intoxicated patients in whom abdominal injury is suggested
-
Patients with potential intra-abdominal injury who will undergo prolonged anesthesia for another procedure
The only absolute contraindication to DPL is the obvious need for laparotomy. Relative contraindications include morbid obesity, a history of multiple abdominal surgeries, and pregnancy.
Various methods of introducing the catheter into the peritoneal space have been described. These include the open, semiopen, and closed methods. The open method requires an infraumbilical skin incision that is extended to and through the linea alba. (In pregnant patients or in patients with particular risk for potential pelvic hematoma, the incision should be placed superior to the umbilicus.) The peritoneum is opened, and the catheter is inserted under direct visualization.
The semiopen method is identical, except that the peritoneum is not opened and the catheter is delivered percutaneously through the peritoneum into the peritoneal cavity. The closed technique requires the catheter to be inserted blindly through the skin, subcutaneous tissue, linea alba, and peritoneum.
The closed and semiopen techniques at the infraumbilical site are preferred at most centers. The fully open method is the most technically demanding and is restricted to those situations in which the closed or semiopen technique is unsuccessful or is deemed unsafe (eg, patients with pelvic fractures, pregnancy, obesity, or prior abdominal operations).
After insertion of the catheter into the peritoneum, attempt to aspirate free intraperitoneal blood (at least 15-20 mL). DPL results are considered positive in a blunt trauma patient if 10 mL of grossly bloody aspirate is obtained before infusion of the lavage fluid or if the siphoned lavage fluid contains more than 100,000 red blood cells (RBCs)/µL, more than 500 white blood cells (WBCs)/µL, elevated amylase content, bile, bacteria, vegetable matter, or urine. Only approximately 30 mL of blood is needed in the peritoneum to produce a microscopically positive DPL result.
If findings are negative, infuse 1 L of crystalloid solution (eg, lactated Ringer solution) into the peritoneum. Then, allow this fluid to drain by gravity, and ensure that laboratory analysis is performed.
Complications of DPL include bleeding from the incision and catheter insertion, infection (ie, wound, peritoneal), and injury to intra-abdominal structures (eg, urinary bladder, small bowel, uterus). These complications may increase the possibility of false-positive studies. Additionally, infection of the incision, peritonitis from the catheter placement, laceration of the urinary bladder, or injury to other intra-abdominal organs can occur.
Bleeding from the incision, dissection, or catheter insertion can cause false-positive results that may lead to unnecessary laparotomy. Achieve appropriate hemostasis prior to entering the peritoneum and placing the catheter. False-positive DPL results can occur if an infraumbilical approach is used in a patient with a pelvic fracture. A pelvic x-ray film should be obtained prior to performing DPL if a pelvic fracture is suggested. Before DPL is attempted, the urinary bladder and stomach should be decompressed.
DPL has been shown in some studies to have a diagnostic accuracy of 98-100%, a sensitivity of 98-100%, and a specificity of 90-96%. It has some advantages, including high sensitivity, rapidity, and immediate interpretation. The main limitations of DPL include its potential for iatrogenic abdominal injury and its high sensitivity, which can lead to nontherapeutic laparotomies.
With the availability of fast, noninvasive, and better imaging modalities (eg, FAST, CT scanning), the role of DPL is now limited to the evaluation of unstable trauma patients in whom FAST results are negative or inconclusive. In some contexts, DPL may be complemented with a CT scan if the patient has positive lavage results but stabilizes.
-
Blunt abdominal trauma. Normal Morison pouch (ie, no free fluid).
-
Blunt abdominal trauma. Free fluid in Morison pouch.
-
Blunt abdominal trauma. Normal splenorenal recess.
-
Blunt abdominal trauma. Free fluid in splenorenal recess.
-
Blunt abdominal trauma with splenic injury and hemoperitoneum.
-
Blunt abdominal trauma with liver laceration.
-
Blunt abdominal trauma. Right kidney injury with blood in perirenal space. Injury resulted from high-speed motor vehicle collision.
-
Ultrasound image of right flank. Clear hypoechoic stripe exists between right kidney and liver in Morison pouch.
-
Ultrasound image of left flank in same patient, with thin hypoechoic stripe above spleen and wider hypoechoic stripe in splenorenal recess.
-
Surgical cricothyroidotomy Seldinger. Video courtesy of Therese Canares, MD, and Jonathan Valente, MD, Rhode Island Hospital, Brown University.