Approach Considerations
Bacillus anthracis is present in high numbers in the ulcer/eschar of cutaneous anthrax, in bloody pleural fluid in inhalational anthrax, in the cerebrospinal fluid (CSF) in anthrax meningitis, and in the blood in septicemic anthrax. Specimens may be stained or cultured to demonstrate the organism. Culture is performed on sheep blood or peptone agar. In persons exposed to antibiotics, immunohistochemical examination of the suspected fluid (eg pleural fluid, CSF, cutaneous biopsy) is performed using antibodies to B anthracis cell wall and capsule.
The diagnosis of cutaneous anthrax is usually suggested by the characteristic appearance of skin lesions. As spore germination occurs within macrophages at the site of inoculation, anthrax bacilli are isolated easily from the vesicular lesions and can be observed on Gram stain. If prior treatment with antibiotics has occurred, the best way to determine infection is to perform serologic testing and punch biopsy at the edge of the lesion and examine by silver staining and immunohistochemical testing.
In patients with inhalational anthrax, a chest radiograph typically shows widening of the mediastinum and pleural effusions, whereas the parenchyma may appear normal. In a review of the 11 patients infected by anthrax in October 2001, chest radiographs from the initial examination showed mediastinal widening, paratracheal and hilar fullness, and pleural effusions or infiltrates. In some patients, the initial findings were subtle and not detected immediately.
Gram Stain and Blood Culture
The preferred diagnostic procedure for cutaneous anthrax is staining the ulcer exudate with methylene blue or Giemsa stain. B anthracis readily grows on blood agar, and staining microbiologically differentiates the organism from non– B anthracis bacilli. Warn laboratory personnel that contracting anthrax from specimens is possible and that they must take appropriate biohazard (level II) precautions.
 Polychrome methylene blue stain of Bacillus anthracis. Image courtesy of Anthrax Vaccine Immunization Program Agency, Office of the Army Surgeon General, United States.
Polychrome methylene blue stain of Bacillus anthracis. Image courtesy of Anthrax Vaccine Immunization Program Agency, Office of the Army Surgeon General, United States.
In patients with cutaneous anthrax who have fever and systemic symptoms that suggest extracutaneous spread, blood culture may be indicated. Treat blood cultures as biohazard II specimens. Blood culture and Gram stain are high-yield tests in infected persons who have not taken antibiotics. Sputum from patients seldom yields positive smears or cultures. A Gram stain is the easiest means of initially identifying suggested cases. Anthrax appears as a large, gram-positive rod.
In October 2001, blood cultures were positive for anthrax in all 8 patients who did not receive antibiotics. Serologic diagnosis of anthrax can be made using a microhemagglutination test specific for the protective antigen (PA) component of the toxin. Any Gram stain results suggestive of anthrax should be reported to the CDC.
Several biochemical tests aid in differentiating B anthracis from other members of the species (chief among them is Bacillus cereus, which has been associated with outbreaks of human food poisoning). B anthracis is characterized by the absence of hemolysis on sheep blood agar, lack of motility, absence of salicin fermentation, gelatin hydrolysis, and lack of growth on phenylethyl alcohol medium.
Enzyme-Linked Immunosorbent Assay
Enzyme-linked immunosorbent assay (ELISA) serologic diagnosis is also available. The ELISA for edema and lethal toxins is positive if a single acute-phase titer is highly elevated or if a fourfold greater rise in the titer is observed between acute and convalescent specimens.
ELISA to detect immunoglobulin G (IgG) response to B anthracis protective antigen (PA) is 98.6% sensitive and 80% specific. Protective antigen–competitive inhibition ELISA is used as a second confirmatory step to improve specificity. Specific IgG anti-PA antibody can be detected as early as 10 days after onset of symptoms, but peak IgG levels may not be observed until 40 days of symptom onset.
Chest Radiography and Computed Tomography
If inhalational anthrax is suspected, obtain a chest radiograph or computed tomography (CT) scan. The appearance on chest radiograph or CT scan may suggest the diagnosis, especially if other predisposing disorders that might result in a widening mediastinum (eg, dissecting aortic aneurysm, bacterial mediastinitis) are absent.
 Inhalation anthrax. Chest radiograph with widened mediastinum 22 hours before death. Image courtesy of P.S. Brachman, MD, Public Health Image Library, US Centers for Disease Control and Prevention, Atlanta, Georgia.
Inhalation anthrax. Chest radiograph with widened mediastinum 22 hours before death. Image courtesy of P.S. Brachman, MD, Public Health Image Library, US Centers for Disease Control and Prevention, Atlanta, Georgia.
Inhalational anthrax often does not appear on chest radiographs as a typical pneumonia; pulmonary densities often are absent. A prominent mediastinum with pleural effusions may be present. The prominent mediastinum is caused by hilar lymphadenopathy. In the 11 cases of inhalational anthrax, initial examination was often subtle but showed mediastinal widening, paratracheal and hilar fullness, and pleural effusions and/or infiltrates.
CT of the chest detects hemorrhagic mediastinal and hilar lymph nodes and edema, peribronchial thickening, and pleural effusions. It also may help differentiate inhalational anthrax from histoplasmosis, sarcoidosis, tuberculosis, and lymphoma.
Lumbar Puncture
If anthrax meningitis is suspected, perform a lumbar puncture to obtain CSF for stain and culture. The CSF in patients with anthrax meningitis is grossly hemorrhagic with few polymorphonuclear neutrophils (PMNs) and numerous gram-positive bacilli. As with other specimens from patients with possible anthrax, advise laboratory personnel to handle specimens with biohazard level II precautions.
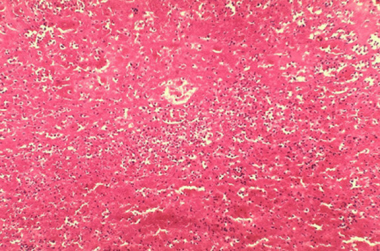
Histologic Findings
The characteristic finding in anthrax is the presence of the organisms in the capillaries at the infection site; therefore, if a patient is infected, expect B anthracis in the capillaries of the skin, intestines, liver, spleen, lungs, or leptomeninges. Pathological findings are not in proportion to the numbers of bacilli present, which is best explained by the effects of one or more of the toxins associated with B anthracis. Hemorrhage may be evident.
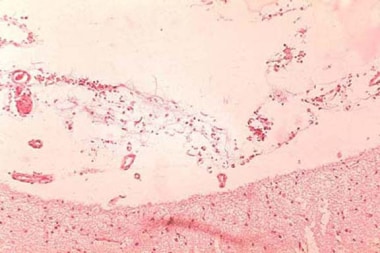
 Histopathology of mediastinal lymph node showing a microcolony of Bacillus anthracis on Giemsa stain. Image courtesy of Marshall Fox, MD, Public Health Image Library, US Centers for Disease Control and Prevention, Atlanta, Georgia.
Histopathology of mediastinal lymph node showing a microcolony of Bacillus anthracis on Giemsa stain. Image courtesy of Marshall Fox, MD, Public Health Image Library, US Centers for Disease Control and Prevention, Atlanta, Georgia.
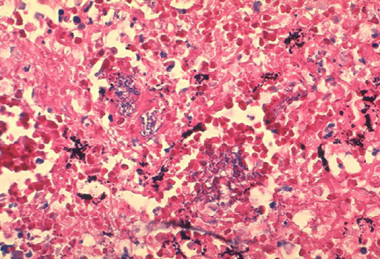
 Histopathology of large intestine showing marked hemorrhage in the mucosa and submucosa. Image courtesy of Marshall Fox, MD, Public Health Image Library, US Centers for Disease Control and Prevention, Atlanta, Georgia.
Histopathology of large intestine showing marked hemorrhage in the mucosa and submucosa. Image courtesy of Marshall Fox, MD, Public Health Image Library, US Centers for Disease Control and Prevention, Atlanta, Georgia.
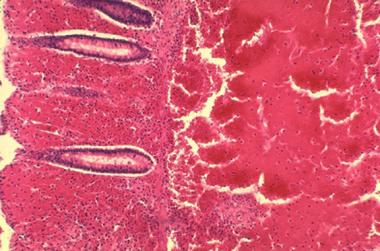
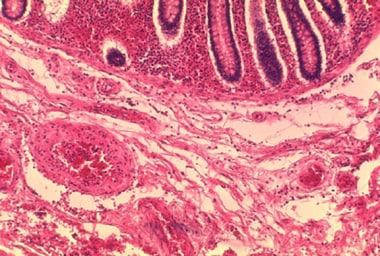 Histopathology of the large intestine showing submucosal thrombosis and edema. Image courtesy of Marshall Fox, MD, Public Health Image Library, US Centers for Disease Control and Prevention, Atlanta, Georgia.
Histopathology of the large intestine showing submucosal thrombosis and edema. Image courtesy of Marshall Fox, MD, Public Health Image Library, US Centers for Disease Control and Prevention, Atlanta, Georgia.
 Histopathology of mediastinal lymph node showing mediastinal necrosis. Image courtesy of Marshall Fox, MD, Public Health Image Library, US Centers for Disease Control and Prevention, Atlanta, Georgia.
Histopathology of mediastinal lymph node showing mediastinal necrosis. Image courtesy of Marshall Fox, MD, Public Health Image Library, US Centers for Disease Control and Prevention, Atlanta, Georgia.
-
Polychrome methylene blue stain of Bacillus anthracis. Image courtesy of Anthrax Vaccine Immunization Program Agency, Office of the Army Surgeon General, United States.
-
Histopathology of mediastinal lymph node showing a microcolony of Bacillus anthracis on Giemsa stain. Image courtesy of Marshall Fox, MD, Public Health Image Library, US Centers for Disease Control and Prevention, Atlanta, Georgia.
-
Cutaneous anthrax. Image courtesy of Anthrax Vaccine Immunization Program Agency, Office of the Army Surgeon General, United States.
-
Skin lesion of anthrax on face. Image courtesy of the Public Health Image Library, US Centers for Disease Control and Prevention, Atlanta, Georgia.
-
Skin lesions of anthrax on neck. Cutaneous anthrax showing the typical black eschar. Image courtesy of the Public Health Image Library, US Centers for Disease Control and Prevention, Atlanta, Georgia.
-
Histopathology of large intestine showing marked hemorrhage in the mucosa and submucosa. Image courtesy of Marshall Fox, MD, Public Health Image Library, US Centers for Disease Control and Prevention, Atlanta, Georgia.
-
Histopathology of the large intestine showing submucosal thrombosis and edema. Image courtesy of Marshall Fox, MD, Public Health Image Library, US Centers for Disease Control and Prevention, Atlanta, Georgia.
-
Inhalation anthrax. Chest radiograph with widened mediastinum 22 hours before death. Image courtesy of P.S. Brachman, MD, Public Health Image Library, US Centers for Disease Control and Prevention, Atlanta, Georgia.
-
Histopathology of mediastinal lymph node showing mediastinal necrosis. Image courtesy of Marshall Fox, MD, Public Health Image Library, US Centers for Disease Control and Prevention, Atlanta, Georgia.
-
Hemorrhagic meningitis resulting from inhalation anthrax. Image courtesy of the Public Health Image Library, US Centers for Disease Control and Prevention, Atlanta, Georgia.
-
Anthrax infection. Histopathology of hemorrhagic meningitis in anthrax. Image courtesy of Marshall Fox, MD, Public Health Image Library, US Centers for Disease Control and Prevention, Atlanta, Georgia.
-
Microscopic picture of anthrax showing gram-positive rods. Image courtesy of Ramon E. Moncada, MD.
-
Seven-month-old infant with anthrax. In this infant, the infection progressed rapidly with significant edema developing the day after exposure. This large hemorrhagic lesion developed within 3 more days. The infant was febrile and was admitted to the hospital on the second day after the symptoms appeared.On September 28, 2001, the infant had visited the mother's workplace. On September 29, nontender massive edema and a weeping erosion developed. On September 30, a 2-cm sore developed over the edematous area. (Note that edema preceded the primary lesion.) On October 2, an ulcer or eschar formed, and the lesion was diagnosed as a spider bite. Hemolytic anemia and thrombocytopenia developed, and the patient was hospitalized. Serum was drawn on October 2; the polymerase chain reaction results were positive for Bacillus anthracis. On October 13, skin biopsy results were positive with immunohistochemical testing for the cell wall antigen.Note that the initial working diagnosis was a Loxosceles reclusa spider bite with superimposed cellulitis. Courtesy of American Academy of Dermatology with permission of NEJM.
-
Fourth patient with cutaneous anthrax in New York City, October 2001. This dry ulcer was present. Photo used with permission of the patient. Courtesy of American Academy of Dermatology. Courtesy of Sharon Balter of the New York City Department of Health.
-
Note the hemorrhage that is associated with cutaneous anthrax lesions. The early ulcer has a moist base. Courtesy of American Academy of Dermatology.
-
Note the central ulcer and eschar. Courtesy of American Academy of Dermatology.
-
An example of a central ulcer and eschar with surrounding edema. Courtesy of American Academy of Dermatology with permission from Boni Elewski, MD.
-
Note the black eschar. Courtesy of American Academy of Dermatology. Courtesy of Gorgas Course in Clinical Tropical Medicine.
-
Anthrax with facial edema. Courtesy of American Academy of Dermatology.