Laboratory Studies
All patients with suspected E coli infection should undergo laboratory analysis based on the clinical syndrome suspected.
Routine CBC count with differential to evaluate for leukocytosis or a left shift may be helpful in isolating a systemic infection but may be normal in isolated cystitis or non-invasive E coli diarrheal diseases.
Microbiological cultures with gram stain from regions of suspected infection can be helpful. Gram stain results determine if the organism is gram-negative, but findings do not distinguish among the other aerobic gram-negative bacilli that cause similar infectious diseases.
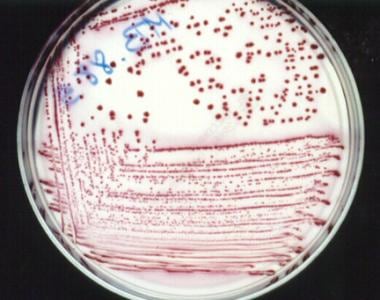
E coli is a gram-negative bacillus that grows well on commonly used media. It is lactose-fermenting and beta-hemolytic on blood agar. Most E coli strains are nonpigmented on blood agar. If additional agars are used, it will grow pink on MacConkey’s agar, and may have a darker color around the colony due to secretion of the bile salts. The image below shows Escherichia coli as a gram-negative (red appearing – safranin counterstain) bacillus (rod shape) on Gram staining.
In the image below Escherichia coli can be seen growing on MacConkey agar.
Definitive diagnosis is based on the isolation of the organism in the microbiology laboratory from clinical specimens. Specimens may be blood, urine, sputum, or other fluids such as cerebrospinal fluid, pleural fluid, abscesses, and peritoneal fluid.
Recovery of the organism in contaminated sites, such as sputum and wounds, must be analyzed in the context of the patient's clinical state to determine if it represents colonization or infection. Recovery from normally sterile sites, such as the CSF, should be considered diagnostic of infection.
Lumbar puncture and a CSF culture positive for E coli establish the diagnosis of acute E coli meningitis; however, lumbar puncture is not justified in all babies presenting with sepsis. Indications for lumbar puncture include positive blood culture results, abnormal neurological signs, and detection of bacterial antigens in the urine.
Individuals with pneumonia generally do not need sputum cultures or blood cultures unless their pneumonia is severe. Patients with severe community acquired pneumonia (CAP) should have sputum cultures performed and have blood cultures performed if septic. These cultures are ideally obtained pre-antibiotic treatment, however antibiotics should not be withheld if cultures cannot be obtained in a timely manner. Factors that favor obtaining sputum cultures are intubated patients, being treated for MRSA/Pseudomonas, previously infected with these prior organisms, or recently hospitalized and received parenteral antibiotics within the past 90 days [10] .
A sputum culture with gram stain is considered a good specimen if there are many leukocytes observed with few squamous cells, representing infection without significant oropharyngeal contamination.
In enteric infections, the causative organism is suggested based on the clinical presentation and the characteristic of the patient's stool. Enterotoxigenic E coli (ETEC), enteropathogenic E coli (EPEC), enteroaggregative E coli (EAggEC), and enteroadherent E coli (EAEC) infections produce watery stools without inflammatory cells. Enteroinvasive E coli (EIEC) infection produces dysentery-type stools, and enterohemorrhagic E coli (EHEC) infection produces hemorrhagic-type stools. If available, a diarrhea panel polymerase chain reaction (PCR) test on stool can assist in discriminating between the different types of E. coli.
In urinary tract infections, a urine dipstick test may be utilized to rapidly determine if the patient has pyuria (white blood cells) or nitrate reducing bacteriuria (many enteric gram-negative bacteria) based on the detection of leukocyte esterase and nitrites. Definitive diagnosis is based on urine culture results, with a normal individual requiring >100,000 colony forming units (CFUs) of a bacteria to be considered an infection, whereas this number is less in a catheterized patient.
Collect the specimen from a midstream clean void or from the superior access area of a urinary catheter in patients with an indwelling Foley catheter. Recognize longstanding Foley catheters may have colonization and may not represent a true infection. If this is the case, it is reasonable to replace the Foley catheter and then draw a urine culture specimen. Do not draw urine cultures on those without symptoms, as there may be bacterial growth >100,000 CFUs, that represents asymptomatic bacteriuria, which only requires treatment in pregnancy and in those undergoing urologic procedures. [11]
Imaging Studies
In suspected pneumonia, chest imaging such as chest radiography is indicated. A CT may be indicated to further delineate potential cause of pneumonia or if used in combination with CT angiography to assess for a pulmonary embolism in the setting of shortness of breath.
In cholecystitis/cholangitis, a right upper quadrant ultrasound is indicated to assess for inflammation and dilation of the gallbladder and bile ducts. CT scans can be utilized to further visualize the inflammation as well as to assess for alternative causes of intraabdominal pain.
In intra-abdominal abscesses, a CT scan with and without IV contrast is indicated to assess for intraabdominal abscesses. Sonograms may be missed due to depth of the lesion as well as bowel air obstructing the sound waves of the ultrasound,
In UTI, a bilateral renal ultrasound is useful to assess for hydronephrosis and inflammation suggestive of obstruction versus pyelonephritis. If clinically indicated, a CT scan may be indicated to assess for obstruction, nephrolithiasis, or intraparenchymal abscesses.
Other Tests
E coli strains that cause diarrhea can be differentiated based on results from molecular tests such as such as polymerase chain reactions on stool. Use of these tests generally is not indicated for acute uncomplicated diarrhea but may be helpful in distinguishing hemorrhagic strains from non-hemorrhagic strains as well as assessing for outbreaks of disease.
Besides PCR tests, other types of E coli can be identified from older tests that are not performed routinely, are difficult to interpret, and require trained microbiology personnel. EPEC can be identified based on findings from serotyping, assays of adherence, and DNA probes. For EAEC and EAggEC, serotyping is not useful, and these strains are identified based on their adherence pattern on tissue culture cells.
EHEC can be identified by looking for the major serotype involved, 0157:H7. Recognize there are other hemolytic strains that do not possess this serotype. EHEC strains are cultured in a sorbitol MacConkey agar. Strains that are sorbitol-negative then are serotyped with 0157:H7 antisera.
Procedures
The following procedures may be indicated:
-
Meningitis - Lumbar puncture with CSF Gram stain/culture. Blood cultures to assess for bacteremic seeding of CSF.
-
Pneumonia – Sputum cultures, bronchoscopy
-
Lung Abscess – Blood cultures, thoracentesis with gram stain / wound culture, sputum culture
-
Cholecystitis/cholangitis - Decompression of biliary system through endoscopic drainage, sphincterotomy for stone extraction, or endoscopic cholangiography
-
Intra-abdominal abscess - Aspiration and drainage. Depending on the size of the abscess, a drain may need to be left to ensure resolution of the abscess.
-
UTI - In cases of ureteral obstruction, placement of stent or stone extraction. Lithotripsy may be required to eliminate a nephrolithiasis, as these can become seeded in UTIs and infection persists until the infected source is removed.
-
Prostatic hypertrophy - Transurethral prostatectomy or transurethral resection of the prostate (TURP)
-
Prostatic abscess – Surgical drainage
-
Escherichia coli liver abscess.
-
Escherichia coli right pyelonephritis.
-
Escherichia coli on Gram stain. Gram-negative bacilli.
-
Escherichia coli culture on MacConkey agar.