Reid LM. Reduction in bronchial subdivision in bronchiectasis. Thorax. 1950 Sep. 5(3):233-47. [QxMD MEDLINE Link]. [Full Text].
Tiddens HA. Chest computed tomography scans should be considered as a routine investigation in cystic fibrosis. Paediatr Respir Rev. 2006 Sep. 7(3):202-8. [QxMD MEDLINE Link].
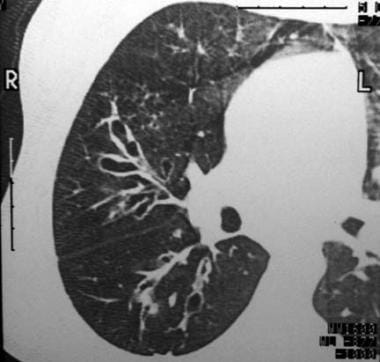
Young K, Aspestrand F, Kolbenstvedt A. High resolution CT and bronchography in the assessment of bronchiectasis. Acta Radiol. 1991 Nov. 32(6):439-41. [QxMD MEDLINE Link].
Smith IE, Flower CD. Review article: imaging in bronchiectasis. Br J Radiol. 1996 Jul. 69(823):589-93. [QxMD MEDLINE Link].
Chalmers JD, McHugh BJ, Docherty C, Govan JR, Hill AT. Vitamin-D deficiency is associated with chronic bacterial colonisation and disease severity in bronchiectasis. Thorax. 2013 Jan. 68(1):39-47. [QxMD MEDLINE Link]. [Full Text].
Davies G, Wilson R. Prophylactic antibiotic treatment of bronchiectasis with azithromycin. Thorax. 2004 Jun. 59(6):540-1. [QxMD MEDLINE Link]. [Full Text].
Tagaya E, Tamaoki J, Kondo M, Nagai A. Effect of a short course of clarithromycin therapy on sputum production in patients with chronic airway hypersecretion. Chest. 2002 Jul. 122(1):213-8. [QxMD MEDLINE Link].
Yalçin E, Kiper N, Ozcelik U, Dogru D, Firat P, Sahin A. Effects of claritromycin on inflammatory parameters and clinical conditions in children with bronchiectasis. J Clin Pharm Ther. 2006 Feb. 31(1):49-55. [QxMD MEDLINE Link].
Luce JM. Bronchiectasis. Murray JF, Nadel JA, eds. Textbook of Respiratory Medicine. 2nd ed. Philadelphia, Pa: WB Saunders and Co; 1994. 1398-1417.
Ip MS, Lam WK. Bronchiectasis and related disorders. Respirology. 1996 Jun. 1(2):107-14. [QxMD MEDLINE Link].
Kolbe J, Wells AU. Bronchiectasis: a neglected cause of respiratory morbidity and mortality. Respirology. 1996 Dec. 1(4):221-5. [QxMD MEDLINE Link].
Morrissey D. Pathogenesis of Bronchiectasis. Clin Chest Med. 2007. 28:289-296.
Cole PJ. A new look at the pathogenesis, management of persistent bronchial sepsis: A 'viscious circle' hypothesis and its logical therapeutic connotations. Davies RJ. Strategies for the Management of Chronic Bacterial Sepsis. Oxford: Medicine Publishing Foundation; 1984. 1-20.
Pasteur M, Helliwell S, Houghton S, et al. An investigation into causitive factors in patients with bronchiectasis. Am J Respir Crit Care Med. 2000. 162:1277-1284.
Singleton R, Morris A, Redding G, et al. Bronchiectasis in Alaska Native children: causes and clinical courses. Pediatr Pulmonol. 2000 Mar. 29(3):182-7. [QxMD MEDLINE Link].
Chang A, Grimwood K, Mulholland E, et al. Bronchiectasis in indigenous children in remote Australian communities. Med J Aust. 2002. 117:200-204.
Barker AF. Bronchiectasis. N Engl J Med. 2002 May 2. 346(18):1383-93. [QxMD MEDLINE Link].
Holmes AH, Trotman-Dickenson B, Edwards A, Peto T, Luzzi GA. Bronchiectasis in HIV disease. Q J Med. 1992 Nov-Dec. 85(307-308):875-82. [QxMD MEDLINE Link].
Reich JM, Johnson RE. Mycobacterium avium complex pulmonary disease presenting as an isolated lingular or middle lobe pattern. The Lady Windermere syndrome. Chest. 1992 Jun. 101(6):1605-9. [QxMD MEDLINE Link].
Koh WJ, Kwon OJ. Bronchiectasis and non-tuberculous mycobacterial pulmonary infection. Thorax. 2006 May. 61(5):458; author reply 458. [QxMD MEDLINE Link]. [Full Text].
Wickremasinghe M, Ozerovitch LJ, Davies G, et al. Non-tuberculous mycobacteria in patients with bronchiectasis. Thorax. 2005 Dec. 60(12):1045-51. [QxMD MEDLINE Link]. [Full Text].
Angrill J, Augusti C, de Celis R, et al. Bacterial colonization in patients with bronchiectasis: microbiological pattern and risk factors. Thorax. 2002. 57:15-19.
King PT, Holdsworth SR, Freezer NJ, Villanueva E, Holmes PW. Microbiologic follow-up study in adult bronchiectasis. Respir Med. 2007 Aug. 101(8):1633-8. [QxMD MEDLINE Link].
Davies G, Wells AU, Doffman S, Watanabe S, Wilson R. The effect of Pseudomonas aeruginosa on pulmonary function in patients with bronchiectasis. Eur Respir J. 2006 Nov. 28(5):974-9. [QxMD MEDLINE Link].
Tsang KW, Lam SK, Lam WK, et al. High seroprevalence of Helicobacter pylori in active bronchiectasis. Am J Respir Crit Care Med. 1998 Oct. 158(4):1047-51. [QxMD MEDLINE Link].
Tsang KW, Lam WK, Kwok E, et al. Helicobacter pylori and upper gastrointestinal symptoms in bronchiectasis. Eur Respir J. 1999 Dec. 14(6):1345-50. [QxMD MEDLINE Link].
De Groote M, Huitt G, Fulton K, et al. Retrospective analysis of aspiration risk and genetic predisposition in bronchiectasis patients with and without non-tuberculous mycobacteria infection. Am J Respir Crit Care Med. 2003. 163:A763.
National Institutes of Health. Genetic testing for cystic fibrosis. National Institutes of Health Consensus Development Conference Statement on genetic testing for cystic fibrosis. Arch Intern Med. 1999 Jul 26. 159(14):1529-39. [QxMD MEDLINE Link].
Yankaskas JR, Marshall BC, Sufian B, Simon RH, Rodman D. Cystic fibrosis adult care: consensus conference report. Chest. 2004 Jan. 125(1 Suppl):1S-39S. [QxMD MEDLINE Link].
Kerem E, Corey M, Kerem BS, et al. The relation between genotype and phenotype in cystic fibrosis--analysis of the most common mutation (delta F508). N Engl J Med. 1990 Nov 29. 323(22):1517-22. [QxMD MEDLINE Link].
Groman JD, Meyer ME, Wilmott RW, Zeitlin PL, Cutting GR. Variant cystic fibrosis phenotypes in the absence of CFTR mutations. N Engl J Med. 2002 Aug 8. 347(6):401-7. [QxMD MEDLINE Link].
Drumm ML, Konstan MW, Schluchter MD, et al. Genetic modifiers of lung disease in cystic fibrosis. N Engl J Med. 2005 Oct 6. 353(14):1443-53. [QxMD MEDLINE Link].
Li Z, Kosorok MR, Farrell PM, et al. Longitudinal development of mucoid Pseudomonas aeruginosa infection and lung disease progression in children with cystic fibrosis. JAMA. 2005 Feb 2. 293(5):581-8. [QxMD MEDLINE Link].
Handelsman DJ, Conway AJ, Boylan LM, Turtle JR. Young's syndrome. Obstructive azoospermia and chronic sinopulmonary infections. N Engl J Med. 1984 Jan 5. 310(1):3-9. [QxMD MEDLINE Link].
Sturgess JM, Thompson MW, Czegledy-Nagy E, Turner JA. Genetic aspects of immotile cilia syndrome. Am J Med Genet. 1986 Sep. 25(1):149-60. [QxMD MEDLINE Link].
Noone PG, Leigh MW, Sannuti A, et al. Primary ciliary dyskinesia: diagnostic and phenotypic features. Am J Respir Crit Care Med. 2004 Feb 15. 169(4):459-67. [QxMD MEDLINE Link].
Lillington GA. Dyskinetic cilia and Kartagener's syndrome. Bronchiectasis with a twist. Clin Rev Allergy Immunol. 2001 Aug. 21(1):65-9. [QxMD MEDLINE Link].
Morrissey B, Louie S. Allergic bronchopulmonary aspergillosis: an evolving challenge in asthma. Gershwin M, Albertson T, eds. Bronchial Asthma: A Guide for Practical Understanding and Treatment. 5th ed. Totowa, NJ: Humana Press; 2006. 279-309.
Vendrell M, de Gracia J, Rodrigo MJ, et al. Antibody production deficiency with normal IgG levels in bronchiectasis of unknown etiology. Chest. 2005 Jan. 127(1):197-204. [QxMD MEDLINE Link].
De Gracia J, Rodrigo MJ, Morell F, et al. IgG subclass deficiencies associated with bronchiectasis. Am J Respir Crit Care Med. 1996 Feb. 153(2):650-5. [QxMD MEDLINE Link].
Thickett KM, Kumararatne DS, Banerjee AK, Dudley R, Stableforth DE. Common variable immune deficiency: respiratory manifestations, pulmonary function and high-resolution CT scan findings. QJM. 2002 Oct. 95(10):655-62. [QxMD MEDLINE Link].
Notarangelo LD, Plebani A, Mazzolari E, Soresina A, Bondioni MP. Genetic causes of bronchiectasis: primary immune deficiencies and the lung. Respiration. 2007. 74(3):264-75. [QxMD MEDLINE Link].
Stover DE, White DA, Romano PA, Gellene RA, Robeson WA. Spectrum of pulmonary diseases associated with the acquired immune deficiency syndrome. Am J Med. 1985 Mar. 78(3):429-37. [QxMD MEDLINE Link].
McGuinness G, Naidich DP, Garay S, Leitman BS, McCauley DI. AIDS associated bronchiectasis: CT features. J Comput Assist Tomogr. 1993 Mar-Apr. 17(2):260-6. [QxMD MEDLINE Link].
Jones VF, Eid NS, Franco SM, Badgett JT, Buchino JJ. Familial congenital bronchiectasis: Williams-Campbell syndrome. Pediatr Pulmonol. 1993 Oct. 16(4):263-7. [QxMD MEDLINE Link].
Woodring JH, Howard RS 2nd, Rehm SR. Congenital tracheobronchomegaly (Mounier-Kuhn syndrome): a report of 10 cases and review of the literature. J Thorac Imaging. 1991 Apr. 6(2):1-10. [QxMD MEDLINE Link].
Cordasco EM Jr, Beder S, Coltro A, Bavbek S, Gurses H, Mehta AC. Clinical features of the yellow nail syndrome. Cleve Clin J Med. 1990 Jul-Aug. 57(5):472-6. [QxMD MEDLINE Link].
Shin MS, Ho KJ. Bronchiectasis in patients with alpha 1-antitrypsin deficiency. A rare occurrence?. Chest. 1993 Nov. 104(5):1384-6. [QxMD MEDLINE Link].
Chan E, Feldman N, Chmura K. Do mutations of the alpha-1-antitrypsin gene predispose to non-tuberculous mycobacterial infection?. Am J Respir Crit Care Med. 2004. 169:A132.
Parr DG, Guest PG, Reynolds JH, Dowson LJ, Stockley RA. Prevalence and impact of bronchiectasis in alpha1-antitrypsin deficiency. Am J Respir Crit Care Med. 2007 Dec 15. 176(12):1215-21. [QxMD MEDLINE Link].
Cuvelier A, Muir JF, Hellot MF, Benhamou D, Martin JP, Benichou J. Distribution of alpha(1)-antitrypsin alleles in patients with bronchiectasis. Chest. 2000 Feb. 117(2):415-9. [QxMD MEDLINE Link].
Walker WC. Pulmonary infections and rheumatoid arthritis. Q J Med. 1967 Apr. 36(142):239-51. [QxMD MEDLINE Link].
Perez T, Remy-Jardin M, Cortet B. Airways involvement in rheumatoid arthritis: clinical, functional, and HRCT findings. Am J Respir Crit Care Med. 1998 May. 157(5 Pt 1):1658-65. [QxMD MEDLINE Link].
McMahon MJ, Swinson DR, Shettar S, Wolstenholme R, Chattopadhyay C, Smith P. Bronchiectasis and rheumatoid arthritis: a clinical study. Ann Rheum Dis. 1993 Nov. 52(11):776-9. [QxMD MEDLINE Link].
Swinson DR, Symmons D, Suresh U, Jones M, Booth J. Decreased survival in patients with co-existent rheumatoid arthritis and bronchiectasis. Br J Rheumatol. 1997 Jun. 36(6):689-91. [QxMD MEDLINE Link].
Robinson DA, Meyer CF. Primary Sjögren's syndrome associated with recurrent sinopulmonary infections and bronchiectasis. J Allergy Clin Immunol. 1994 Aug. 94(2 Pt 1):263-4. [QxMD MEDLINE Link].
Casserly IP, Fenlon HM, Breatnach E, Sant SM. Lung findings on high-resolution computed tomography in idiopathic ankylosing spondylitis--correlation with clinical findings, pulmonary function testing and plain radiography. Br J Rheumatol. 1997 Jun. 36(6):677-82. [QxMD MEDLINE Link].
Fenlon HM, Doran M, Sant SM, Breatnach E. High-resolution chest CT in systemic lupus erythematosus. AJR Am J Roentgenol. 1996 Feb. 166(2):301-7. [QxMD MEDLINE Link].
Tillie-Leblond I, Wallaert B, Leblond D, et al. Respiratory involvement in relapsing polychondritis. Clinical, functional, endoscopic, and radiographic evaluations. Medicine (Baltimore). 1998 May. 77(3):168-76. [QxMD MEDLINE Link].
Camus P, Colby TV. The lung in inflammatory bowel disease. Eur Respir J. 2000 Jan. 15(1):5-10. [QxMD MEDLINE Link].
Rockoff SD, Rohatgi PK. Unusual manifestations of thoracic sarcoidosis. AJR Am J Roentgenol. 1985 Mar. 144(3):513-28. [QxMD MEDLINE Link].
Wood JR, Bellamy D, Child AH, Citron KM. Pulmonary disease in patients with Marfan syndrome. Thorax. 1984 Oct. 39(10):780-4. [QxMD MEDLINE Link]. [Full Text].
Driscoll JA, Bhalla S, Liapis H, Ibricevic A, Brody SL. Autosomal dominant polycystic kidney disease is associated with an increased prevalence of radiographic bronchiectasis. Chest. 2008 May. 133(5):1181-8. [QxMD MEDLINE Link].
Javidan-Nejad C, Bhalla S. Bronchiectasis. Radiol Clin North Am. 2009 Mar. 47(2):289-306. [QxMD MEDLINE Link].
Kennedy TP, Weber DJ. Nontuberculous mycobacteria. An underappreciated cause of geriatric lung disease. Am J Respir Crit Care Med. 1994 Jun. 149(6):1654-8. [QxMD MEDLINE Link].
Nikolaizik WH, Warner JO. Aetiology of chronic suppurative lung disease. Arch Dis Child. 1994 Feb. 70(2):141-2. [QxMD MEDLINE Link]. [Full Text].
Wallace RJ Jr. Mycobacterium avium complex lung disease and women. Now an equal opportunity disease. Chest. 1994 Jan. 105(1):6-7. [QxMD MEDLINE Link].
Iseman MD, Buschman DL, Ackerson LM. Pectus excavatum and scoliosis. Thoracic anomalies associated with pulmonary disease caused by Mycobacterium avium complex. Am Rev Respir Dis. 1991 Oct. 144(4):914-6. [QxMD MEDLINE Link].
Nicotra MB, Rivera M, Dale AM, Shepherd R, Carter R. Clinical, pathophysiologic, and microbiologic characterization of bronchiectasis in an aging cohort. Chest. 1995 Oct. 108(4):955-61. [QxMD MEDLINE Link].
Seitz AE, Olivier KN, Steiner CA, et al. Trends and burden of bronchiectasis-associated hospitalizations in the United States, 1993-2006. Chest. 2010 Oct. 138(4):944-9. [QxMD MEDLINE Link]. [Full Text].
Morrissey BM, Harper RW. Bronchiectasis: sex and gender considerations. Clin Chest Med. 2004 Jun. 25(2):361-72. [QxMD MEDLINE Link].
Perry K, King D. Bronchiectasis, a study of prognosis based on a follow-up of 400 patients. Am Rev Tuber. 1941. 40:53.
Ellis DA, Thornley PE, Wightman AJ, Walker M, Chalmers J, Crofton JW. Present outlook in bronchiectasis: clinical and social study and review of factors influencing prognosis. Thorax. 1981 Sep. 36(9):659-64. [QxMD MEDLINE Link]. [Full Text].
Keistinen T, Saynajakangas O, Tuuponen T, Kivela SL. Bronchiectasis: an orphan disease with a poorly-understood prognosis. Eur Respir J. 1997 Dec. 10(12):2784-7. [QxMD MEDLINE Link].
Saynajakangas O, Keistinen T, Tuuponen T, Kivela SL. Bronchiectasis in Finland: trends in hospital treatment. Respir Med. 1997 Aug. 91(7):395-8. [QxMD MEDLINE Link].
Dupont M, Gacouin A, Lena H, et al. Survival of patients with bronchiectasis after the first ICU stay for respiratory failure. Chest. 2004 May. 125(5):1815-20. [QxMD MEDLINE Link].
Onen ZP, Gulbay BE, Sen E, et al. Analysis of the factors related to mortality in patients with bronchiectasis. Respir Med. 2007 Jul. 101(7):1390-7. [QxMD MEDLINE Link].
Janeczko L. Children With Chronic Wet Cough Despite Antibiotics May Have Bronchiectasis. Medscape Medical News. Available at http://www.medscape.com/viewarticle/822067. Accessed: March 24, 2014.
Goyal V, Grimwood K, Marchant J, Masters IB, Chang AB. Does failed chronic wet cough response to antibiotics predict bronchiectasis?. Arch Dis Child. 2014 Feb 12. [QxMD MEDLINE Link].
Rosen MJ. Chronic cough due to bronchiectasis: ACCP evidence-based clinical practice guidelines. Chest. 2006 Jan. 129(1 Suppl):122S-131S. [QxMD MEDLINE Link].
King PT, Holdsworth SR, Freezer NJ, Villanueva E, Holmes PW. Characterisation of the onset and presenting clinical features of adult bronchiectasis. Respir Med. 2006 Dec. 100(12):2183-9. [QxMD MEDLINE Link].
Flume PA, Yankaskas JR, Ebeling M, Hulsey T, Clark LL. Massive hemoptysis in cystic fibrosis. Chest. 2005 Aug. 128(2):729-38. [QxMD MEDLINE Link].
Prys-Picard CO, Niven R. Urinary incontinence in patients with bronchiectasis. Eur Respir J. 2006 Apr. 27(4):866-7. [QxMD MEDLINE Link].
Hansell DM. Bronchiectasis. Radiol Clin North Am. 1998 Jan. 36(1):107-28. [QxMD MEDLINE Link].
Mannino DM, Davis KJ. Lung function decline and outcomes in an elderly population. Thorax. 2006 Jun. 61(6):472-7. [QxMD MEDLINE Link]. [Full Text].
Martinez-Garcia MA, Soler-Cataluna JJ, Perpina-Tordera M, Roman-Sanchez P, Soriano J. Factors associated with lung function decline in adult patients with stable non-cystic fibrosis bronchiectasis. Chest. 2007 Nov. 132(5):1565-72. [QxMD MEDLINE Link].
Chang C, Singleton R, Morris P and et al. Pneumococcal vaccines for children and adults with bronchiectasis. The Cochrane Database of Systematic Reviews. 2008. 3:
Chang CC, Morris PS, Chang AB. Influenza vaccine for children and adults with bronchiectasis. Cochrane Database Syst Rev. 2007 Jul 18. CD006218. [QxMD MEDLINE Link].
Evans DJ, Bara AI, Greenstone M. Prolonged antibiotics for purulent bronchiectasis. Cochrane Database Syst Rev. 2003. (4):CD001392. [QxMD MEDLINE Link].
Evans DJ, Greenstone M. Long-term antibiotics in the management of non-CF bronchiectasis--do they improve outcome?. Respir Med. 2003 Jul. 97(7):851-8. [QxMD MEDLINE Link].
Rubin BK. Aerosolized antibiotics for non-cystic fibrosis bronchiectasis. J Aerosol Med Pulm Drug Deliv. 2008 Mar. 21(1):71-6. [QxMD MEDLINE Link].
Barker AF, Couch L, Fiel SB, et al. Tobramycin solution for inhalation reduces sputum Pseudomonas aeruginosa density in bronchiectasis. Am J Respir Crit Care Med. 2000 Aug. 162(2 Pt 1):481-5. [QxMD MEDLINE Link].
Bilton D, Henig N, Morrissey B, Gotfried M. Addition of inhaled tobramycin to ciprofloxacin for acute exacerbations of Pseudomonas aeruginosa infection in adult bronchiectasis. Chest. 2006 Nov. 130(5):1503-10. [QxMD MEDLINE Link].
Haciibrahimoglu G, Fazlioglu M, Olcmen A, Gurses A, Bedirhan MA. Surgical management of childhood bronchiectasis due to infectious disease. J Thorac Cardiovasc Surg. 2004 May. 127(5):1361-5. [QxMD MEDLINE Link].
Drobnic ME, Sune P, Montoro JB, Ferrer A, Orriols R. Inhaled tobramycin in non-cystic fibrosis patients with bronchiectasis and chronic bronchial infection with Pseudomonas aeruginosa. Ann Pharmacother. 2005 Jan. 39(1):39-44. [QxMD MEDLINE Link].
Scheinberg P, Shore E. A pilot study of the safety and efficacy of tobramycin solution for inhalation in patients with severe bronchiectasis. Chest. 2005 Apr. 127(4):1420-6. [QxMD MEDLINE Link].
Lin H, Cheng H, Wang C, et al. Inhaled gentamicin reduces airway neutrophil activity and mucus secretion in bronchiectasis. Am J Respir Crit Care Med. 1999. 155:2024-2029.
Steinfort DP, Steinfort C. Effect of long-term nebulized colistin on lung function and quality of life in patients with chronic bronchial sepsis. Intern Med J. 2007 Jul. 37(7):495-8. [QxMD MEDLINE Link].
Murray MP, Govan JR, Doherty CJ, et al. A randomized controlled trial of nebulized gentamicin in non-cystic fibrosis bronchiectasis. Am J Respir Crit Care Med. 2011 Feb 15. 183(4):491-9. [QxMD MEDLINE Link].
Patterson JE, Hewitt O, Kent L, Bradbury I, Elborn JS, Bradley JM. Acapella versus 'usual airway clearance' during acute exacerbation in bronchiectasis: a randomized crossover trial. Chron Respir Dis. 2007. 4(2):67-74. [QxMD MEDLINE Link].
Eaton T, Young P, Zeng I, Kolbe J. A randomized evaluation of the acute efficacy, acceptability and tolerability of flutter and active cycle of breathing with and without postural drainage in non-cystic fibrosis bronchiectasis. Chron Respir Dis. 2007. 4(1):23-30. [QxMD MEDLINE Link].
Langenderfer B. Alternatives to percussion and postural drainage. A review of mucus clearance therapies: percussion and postural drainage, autogenic drainage, positive expiratory pressure, flutter valve, intrapulmonary percussive ventilation, and high-frequency chest compression with the ThAIRapy Vest. J Cardiopulm Rehabil. 1998 Jul-Aug. 18(4):283-9. [QxMD MEDLINE Link].
Mutalithas K, Watkin G, Willig B, Wardlaw A, Pavord ID, Birring SS. Improvement in health status following bronchopulmonary hygiene physical therapy in patients with bronchiectasis. Respir Med. 2008 Aug. 102(8):1140-4. [QxMD MEDLINE Link].
Donaldson SH, Bennett WD, Zeman KL, Knowles MR, Tarran R, Boucher RC. Mucus clearance and lung function in cystic fibrosis with hypertonic saline. N Engl J Med. 2006 Jan 19. 354(3):241-50. [QxMD MEDLINE Link].
Elkins MR, Robinson M, Rose BR, et al. A controlled trial of long-term inhaled hypertonic saline in patients with cystic fibrosis. N Engl J Med. 2006 Jan 19. 354(3):229-40. [QxMD MEDLINE Link].
Florescu DF, Murphy PJ, Kalil AC. Effects of prolonged use of azithromycin in patients with cystic fibrosis: a meta-analysis. Pulm Pharmacol Ther. 2009 Dec. 22(6):467-72. [QxMD MEDLINE Link].
Fuchs HJ, Borowitz DS, Christiansen DH, et al. Effect of aerosolized recombinant human DNase on exacerbations of respiratory symptoms and on pulmonary function in patients with cystic fibrosis. The Pulmozyme Study Group. N Engl J Med. 1994 Sep 8. 331(10):637-42. [QxMD MEDLINE Link].
Paul K, Rietschel E, Ballmann M, et al. Effect of treatment with dornase alpha on airway inflammation in patients with cystic fibrosis. Am J Respir Crit Care Med. 2004 Mar 15. 169(6):719-25. [QxMD MEDLINE Link].
O'Donnell AE, Barker AF, Ilowite JS, Fick RB. Treatment of idiopathic bronchiectasis with aerosolized recombinant human DNase I. rhDNase Study Group. Chest. 1998 May. 113(5):1329-34. [QxMD MEDLINE Link].
Franco F, Sheikh A, Greenstone M. Short acting beta-2 agonists for bronchiectasis. Cochrane Database Syst Rev. 2003. CD003572. [QxMD MEDLINE Link].
Sheikh A, Nolan D, Greenstone M. Long-acting beta-2-agonists for bronchiectasis. Cochrane Database Syst Rev. 2001. CD002155. [QxMD MEDLINE Link].
Lasserson T, Holt K, Evans D, Greenstone M. Anticholinergic therapy for bronchiectasis. Cochrane Database Syst Rev. 2001. CD002163. [QxMD MEDLINE Link].
Kolbe J, Wells A, Ram FS. Inhaled steroids for bronchiectasis. Cochrane Database Syst Rev. 2000. CD000996. [QxMD MEDLINE Link].
Lasserson T, Holt K, Greenstone M. Oral steroids for bronchiectasis (stable and acute exacerbations). Cochrane Database Syst Rev. 2001. CD002162. [QxMD MEDLINE Link].
Corless JA, Warburton CJ. Leukotriene receptor antagonists for non-cystic fibrosis bronchiectasis. Cochrane Database Syst Rev. 2000. (4):CD002174. [QxMD MEDLINE Link].
Kapur N, Petsky HL, Bell S, Kolbe J, Chang AB. Inhaled corticosteroids for bronchiectasis. Cochrane Database Syst Rev. 2018 May 16. 5:CD000996. [QxMD MEDLINE Link].
Tsang KW, Tan KC, Ho PL, et al. Inhaled fluticasone in bronchiectasis: a 12 month study. Thorax. 2005 Mar. 60(3):239-43. [QxMD MEDLINE Link]. [Full Text].
Martinez-Garcia MA, Perpina-Tordera M, Roman-Sanchez P, Soler-Cataluna JJ. Inhaled steroids improve quality of life in patients with steady-state bronchiectasis. Respir Med. 2006 Sep. 100(9):1623-32. [QxMD MEDLINE Link].
Anwar GA, Bourke SC, Afolabi G, Middleton P, Ward C, Rutherford RM. Effects of long-term low-dose azithromycin in patients with non-CF bronchiectasis. Respir Med. 2008 Oct. 102(10):1494-6. [QxMD MEDLINE Link].
Wong C, Jayaram L, Karalus N, Eaton T, Tong C, Hockey H, et al. Azithromycin for prevention of exacerbations in non-cystic fibrosis bronchiectasis (EMBRACE): a randomised, double-blind, placebo-controlled trial. Lancet. 2012 Aug 18. 380(9842):660-7. [QxMD MEDLINE Link].
Kapur N, Bell S, Kolbe J, Chang AB. Inhaled steroids for bronchiectasis. Cochrane Database Syst Rev. 2009 Jan 21. CD000996. [QxMD MEDLINE Link].
Corless JA, Warburton CJ. Surgery vs non-surgical treatment for bronchiectasis. Cochrane Database Syst Rev. 2000. (4):CD002180. [QxMD MEDLINE Link].
Balkanli K, Genc O, Dakak M, et al. Surgical management of bronchiectasis: analysis and short-term results in 238 patients. Eur J Cardiothorac Surg. 2003 Nov. 24(5):699-702. [QxMD MEDLINE Link].
Agasthian T, Deschamps C, Trastek VF, Allen MS, Pairolero PC. Surgical management of bronchiectasis. Ann Thorac Surg. 1996 Oct. 62(4):976-8; discussion 979-80. [QxMD MEDLINE Link].
[Guideline] Polverino E, Goeminne PC, McDonnell MJ, et al. European Respiratory Society guidelines for the management of adult bronchiectasis. Eur Respir J. 2017 Sep. 50 (3):[QxMD MEDLINE Link]. [Full Text].