Hoffman GS. Giant Cell Arteritis. Ann Intern Med. 2016 Nov 1. 165 (9):ITC65-ITC80. [QxMD MEDLINE Link].
Ameer MA, Peterfy RJ, Khazaeni B. Temporal Arteritis. 2022 Jan. [QxMD MEDLINE Link]. [Full Text].
Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, et al. 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 2013 Jan. 65 (1):1-11. [QxMD MEDLINE Link]. [Full Text].
Waldman CW, Waldman SD, Waldman RA. Giant cell arteritis. Med Clin North Am. 2013 Mar. 97(2):329-35. [QxMD MEDLINE Link].
Cantini F, Niccoli L, Storri L, Nannini C, Olivieri I, Padula A, et al. Are polymyalgia rheumatica and giant cell arteritis the same disease?. Semin Arthritis Rheum. 2004 Apr. 33(5):294-301. [QxMD MEDLINE Link].
Dejaco C, Duftner C, Buttgereit F, Matteson EL, Dasgupta B. The spectrum of giant cell arteritis and polymyalgia rheumatica: revisiting the concept of the disease. Rheumatology (Oxford). 2016 Aug 1. [QxMD MEDLINE Link].
Liozon E, Ly KH, Robert PY. [Ocular complications of giant cell arteritis]. Rev Med Interne. 2013 Jul. 34(7):421-30. [QxMD MEDLINE Link].
Birkhead NC, Wagener HP, Shick RM. Treatment of temporal arteritis with adrenal corticosteroids: Results in 55 cases in which the lesion was proved at biopsy. JAMA. 1975. 163:821.
O'Brien JP, Regan W. Actinically degenerate elastic tissue is the likely antigenic basis of actinic granuloma of the skin and of temporal arteritis. J Am Acad Dermatol. 1999 Feb. 40(2 Pt 1):214-22. [QxMD MEDLINE Link].
Samson M, Corbera-Bellalta M, Audia S, Planas-Rigol E, Martin L, Cid MC, et al. Recent advances in our understanding of giant cell arteritis pathogenesis. Autoimmun Rev. 2017 May 28. [QxMD MEDLINE Link].
Diaz VA, DeBroff BM, Sinard J. Comparison of histopathologic features, clinical symptoms, and erythrocyte sedimentation rates in biopsy-positive temporal arteritis. Ophthalmology. 2005 Jul. 112(7):1293-8. [QxMD MEDLINE Link].
Rodríguez-Pla A, Bosch-Gil JA, Rosselló-Urgell J, Huguet-Redecilla P, Stone JH, Vilardell-Tarres M. Metalloproteinase-2 and -9 in giant cell arteritis: involvement in vascular remodeling. Circulation. 2005 Jul 12. 112(2):264-9. [QxMD MEDLINE Link].
Eberhardt RT, Dhadly M. Giant cell arteritis: diagnosis, management, and cardiovascular implications. Cardiol Rev. 2007 Mar-Apr. 15(2):55-61. [QxMD MEDLINE Link].
Cid MC, Cebrián M, Font C, Coll-Vinent B, Hernández-Rodríguez J, Esparza J, et al. Cell adhesion molecules in the development of inflammatory infiltrates in giant cell arteritis: inflammation-induced angiogenesis as the preferential site of leukocyte-endothelial cell interactions. Arthritis Rheum. 2000 Jan. 43(1):184-94. [QxMD MEDLINE Link].
Maugeri N, Baldini M, Rovere-Querini P, Maseri A, Sabbadini MG, Manfredi AA. Leukocyte and platelet activation in patients with giant cell arteritis and polymyalgia rheumatica: a clue to thromboembolic risks?. Autoimmunity. 2009 May. 42(4):386-8. [QxMD MEDLINE Link].
Goodwin JS. Progress in gerontology: polymyalgia rheumatica and temporal arteritis. J Am Geriatr Soc. 1992 May. 40(5):515-25. [QxMD MEDLINE Link].
Borchers AT, Gershwin ME. Giant cell arteritis: a review of classification, pathophysiology, geoepidemiology and treatment. Autoimmun Rev. 2012 May. 11(6-7):A544-54. [QxMD MEDLINE Link].
Wilkinson IM, Russell RW. Arteries of the head and neck in giant cell arteritis. A pathological study to show the pattern of arterial involvement. Arch Neurol. 1972 Nov. 27(5):378-91. [QxMD MEDLINE Link].
Scola CJ, Li C, Upchurch KS. Mesenteric involvement in giant cell arteritis. An underrecognized complication? Analysis of a case series with clinicoanatomic correlation. Medicine (Baltimore). 2008 Jan. 87(1):45-51. [QxMD MEDLINE Link].
Kermani TA, Warrington KJ. Lower extremity vasculitis in polymyalgia rheumatica and giant cell arteritis. Curr Opin Rheumatol. 2011 Jan. 23(1):38-42. [QxMD MEDLINE Link]. [Full Text].
Salvarani C, Pipitone N, Boiardi L, Hunder GG. Do we need treatment with tumour necrosis factor blockers for giant cell arteritis?. Ann Rheum Dis. 2008 May. 67(5):577-9. [QxMD MEDLINE Link].
Caylor TL, Perkins A. Recognition and management of polymyalgia rheumatica and giant cell arteritis. Am Fam Physician. 2013 Nov 15. 88 (10):676-84. [QxMD MEDLINE Link]. [Full Text].
Salvarani C, Cantini F, Hunder GG. Polymyalgia rheumatica and giant-cell arteritis. Lancet. 2008 Jul 19. 372(9634):234-45. [QxMD MEDLINE Link].
Buttgereit F, Dejaco C, Matteson EL, Dasgupta B. Polymyalgia Rheumatica and Giant Cell Arteritis: A Systematic Review. JAMA. 2016 Jun 14. 315 (22):2442-58. [QxMD MEDLINE Link].
Liozon E, Ouattara B, Rhaiem K, Ly K, Bezanahary H, Loustaud V, et al. Familial aggregation in giant cell arteritis and polymyalgia rheumatica: a comprehensive literature review including 4 new families. Clin Exp Rheumatol. 2009 Jan-Feb. 27(1 Suppl 52):S89-94. [QxMD MEDLINE Link].
Palomino-Morales R, Torres O, Vazquez-Rodriguez TR, Morado IC, Castañeda S, Callejas-Rubio JL, et al. Association between toll-like receptor 4 gene polymorphism and biopsy-proven giant cell arteritis. J Rheumatol. 2009 Jul. 36(7):1501-6. [QxMD MEDLINE Link].
Alvarez-Lafuente R, Fernández-Gutiérrez B, Jover JA, Júdez E, Loza E, Clemente D, et al. Human parvovirus B19, varicella zoster virus, and human herpes virus 6 in temporal artery biopsy specimens of patients with giant cell arteritis: analysis with quantitative real time polymerase chain reaction. Ann Rheum Dis. 2005 May. 64(5):780-2. [QxMD MEDLINE Link]. [Full Text].
Russo MG, Waxman J, Abdoh AA, Serebro LH. Correlation between infection and the onset of the giant cell (temporal) arteritis syndrome. A trigger mechanism?. Arthritis Rheum. 1995 Mar. 38(3):374-80. [QxMD MEDLINE Link].
Gilden D, Nagel M. Varicella Zoster Virus in Temporal Arteries of Patients With Giant Cell Arteritis. J Infect Dis. 2015 Jul 15. 212 Suppl 1:S37-9. [QxMD MEDLINE Link]. [Full Text].
Pache M, Kaiser HJ, Haufschild T, Lübeck P, Flammer J. Increased endothelin-1 plasma levels in giant cell arteritis: a report on four patients. Am J Ophthalmol. 2002 Jan. 133(1):160-2. [QxMD MEDLINE Link].
Patel SJ, Lundy DC. Ocular manifestations of autoimmune disease. Am Fam Physician. 2002 Sep 15. 66(6):991-8. [QxMD MEDLINE Link].
Salvarani C, Gabriel SE, O'Fallon WM, Hunder GG. The incidence of giant cell arteritis in Olmsted County, Minnesota: apparent fluctuations in a cyclic pattern. Ann Intern Med. 1995 Aug 1. 123(3):192-4. [QxMD MEDLINE Link].
Smeeth L, Cook C, Hall AJ. Incidence of diagnosed polymyalgia rheumatica and temporal arteritis in the United Kingdom, 1990-2001. Ann Rheum Dis. 2006 Aug. 65(8):1093-8. [QxMD MEDLINE Link]. [Full Text].
Ing EB, Lahaie Luna G, Pagnoux C, Baer PA, Wang D, Benard-Seguin E, et al. The incidence of giant cell arteritis in Ontario, Canada. Can J Ophthalmol. 2019 Feb. 54 (1):119-124. [QxMD MEDLINE Link].
Ramstead CL, Patel AD. Giant cell arteritis in a neuro-ophthalmology clinic in Saskatoon, 1998-2003. Can J Ophthalmol. 2007 Apr. 42(2):295-8. [QxMD MEDLINE Link].
Ostberg G. Temporal arteritis in a large necropsy series. Ann Rheum Dis. 1971 May. 30(3):224-35. [QxMD MEDLINE Link]. [Full Text].
Bosley TM, Riley FC. Giant cell arteritis in Saudi Arabia. Int Ophthalmol. 1998. 22(1):59-60. [QxMD MEDLINE Link].
Artal NM, Rodriguez M, Luna JD, Reviglio VE, Cuello O, Muiñ JC, et al. Giant cell arteritis in a Hispanic population. Ophthalmology. 2002 Oct. 109(10):1757; discussion 1757. [QxMD MEDLINE Link].
Liu NH, LaBree LD, Feldon SE, Rao NA. The epidemiology of giant cell arteritis : a 12-year retrospective study. Ophthalmology. 2001 Jun. 108(6):1145-9. [QxMD MEDLINE Link].
Restuccia G, Boiardi L, Cavazza A, Catanoso M, Macchioni P, Muratore F, et al. Long-term remission in biopsy proven giant cell arteritis: A retrospective cohort study. J Autoimmun. 2016 Oct 11. [QxMD MEDLINE Link].
Narváez J, Nolla-Solé JM, Clavaguera MT, Valverde-García J, Roig-Escofet D. Longterm therapy in polymyalgia rheumatica: effect of coexistent temporal arteritis. J Rheumatol. 1999 Sep. 26(9):1945-52. [QxMD MEDLINE Link].
Foroozan R, Deramo VA, Buono LM, Jayamanne DG, Sergott RC, Danesh-Meyer H, et al. Recovery of visual function in patients with biopsy-proven giant cell arteritis. Ophthalmology. 2003 Mar. 110(3):539-42. [QxMD MEDLINE Link].
González-Gay MA, García-Porrúa C, Llorca J, Hajeer AH, Brañas F, Dababneh A, et al. Visual manifestations of giant cell arteritis. Trends and clinical spectrum in 161 patients. Medicine (Baltimore). 2000 Sep. 79(5):283-92. [QxMD MEDLINE Link].
Scheurer RA, Harrison AR, Lee MS. Treatment of vision loss in giant cell arteritis. Curr Treat Options Neurol. 2012 Feb. 14(1):84-92. [QxMD MEDLINE Link].
Danesh-Meyer H, Savino PJ, Gamble GG. Poor prognosis of visual outcome after visual loss from giant cell arteritis. Ophthalmology. 2005 Jun. 112(6):1098-103. [QxMD MEDLINE Link].
Hayreh SS, Zimmerman B. Visual deterioration in giant cell arteritis patients while on high doses of corticosteroid therapy. Ophthalmology. 2003 Jun. 110(6):1204-15. [QxMD MEDLINE Link].
Loddenkemper T, Sharma P, Katzan I, Plant GT. Risk factors for early visual deterioration in temporal arteritis. J Neurol Neurosurg Psychiatry. 2007 Nov. 78(11):1255-9. [QxMD MEDLINE Link]. [Full Text].
Wiszniewska M, Devuyst G, Bogousslavsky J. Giant cell arteritis as a cause of first-ever stroke. Cerebrovasc Dis. 2007. 24(2-3):226-30. [QxMD MEDLINE Link].
Solans-Laqué R, Bosch-Gil JA, Molina-Catenario CA, Ortega-Aznar A, Alvarez-Sabin J, Vilardell-Tarres M. Stroke and multi-infarct dementia as presenting symptoms of giant cell arteritis: report of 7 cases and review of the literature. Medicine (Baltimore). 2008 Nov. 87(6):335-44. [QxMD MEDLINE Link].
Taylor S, Lightman S. The eye in cardiac and cardiovascular disease. Hosp Med. 2003 May. 64(5):299-301. [QxMD MEDLINE Link].
Smulders YM, Verhagen DW. Giant cell arteritis causing aortic dissection and acute hypertension. BMJ. 2008 Jul 4. 337:a426. [QxMD MEDLINE Link].
Tomasson G, Peloquin C, Mohammad A, Love TJ, Zhang Y, Choi HK, et al. Risk for cardiovascular disease early and late after a diagnosis of giant-cell arteritis: a cohort study. Ann Intern Med. 2014 Jan 21. 160(2):73-80. [QxMD MEDLINE Link].
Ninan J, Nguyen AM, Cole A, Rischmueller M, Dodd T, Roberts-Thomson P, et al. Mortality in patients with biopsy-proven giant cell arteritis: a south australian population-based study. J Rheumatol. 2011 Oct. 38(10):2215-7. [QxMD MEDLINE Link].
Hunder GG, Bloch DA, Michel BA, Stevens MB, Arend WP, Calabrese LH, et al. The American College of Rheumatology 1990 criteria for the classification of giant cell arteritis. Arthritis Rheum. 1990 Aug. 33(8):1122-8. [QxMD MEDLINE Link].
[Guideline] Dasgupta B, Borg FA, Hassan N, Alexander L, Barraclough K, Bourke B, et al. BSR and BHPR guidelines for the management of giant cell arteritis. Rheumatology (Oxford). 2010 Aug. 49 (8):1594-7. [QxMD MEDLINE Link]. [Full Text].
Kuo CH, McCluskey P, Fraser CL. Chewing Gum Test for Jaw Claudication in Giant-Cell Arteritis. N Engl J Med. 2016 May 5. 374 (18):1794-5. [QxMD MEDLINE Link]. [Full Text].
Bhatti MT, Frohman L, Nesher G. MD Roundtable: Diagnosing Giant Cell Arteritis. EyeNet. 2017 June. 21(6):31-34.
Kumar B, Toney DE, Alikhan M, Lohr KM. Giant cell arteritis presenting as depressed mood and headache in an elderly patient. J Clin Rheumatol. 2013 Oct. 19(7):405-6. [QxMD MEDLINE Link].
Johnson H, Bouman W, Pinner G. Psychiatric aspects of temporal arteritis: a case report and review of the literature. J Geriatr Psychiatry Neurol. 1997 Oct. 10(4):142-5. [QxMD MEDLINE Link].
Adams WB, Becknell CA. Rare manifestation of scalp necrosis in temporal arteritis. Arch Dermatol. 2007 Aug. 143(8):1079-80. [QxMD MEDLINE Link].
Tsianakas A, Ehrchen JM, Presser D, Fischer T, Kruse-Loesler B, Luger TA, et al. Scalp necrosis in giant cell arteritis: case report and review of the relevance of this cutaneous sign of large-vessel vasculitis. J Am Acad Dermatol. 2009 Oct. 61(4):701-6. [QxMD MEDLINE Link].
Brodmann M, Dorr A, Hafner F, Gary T, Pilger E. Tongue necrosis as first symptom of giant cell arteritis (GCA). Clin Rheumatol. 2009 Jun. 28 Suppl 1:S47-9. [QxMD MEDLINE Link].
Nesher G, Nesher R, Rozenman Y, Sonnenblick M. Visual hallucinations in giant cell arteritis: association with visual loss. J Rheumatol. 2001 Sep. 28(9):2046-8. [QxMD MEDLINE Link].
Amor-Dorado JC, Llorca J, Garcia-Porrua C, Costa C, Perez-Fernandez N, Gonzalez-Gay MA. Audiovestibular manifestations in giant cell arteritis: a prospective study. Medicine (Baltimore). 2003 Jan. 82(1):13-26. [QxMD MEDLINE Link].
Rizzo J. Giant cell arteritis. Boston, Mass: Lecture presented at: Massachusetts Eye and Ear Infirmary; Spring 2000.
Danesh-Meyer H, Savino PJ, Spaeth GL, Gamble GD. Comparison of arteritis and nonarteritic anterior ischemic optic neuropathies with the Heidelberg Retina Tomograph. Ophthalmology. 2005 Jun. 112(6):1104-12. [QxMD MEDLINE Link].
Hayreh SS. Posterior ischaemic optic neuropathy: clinical features, pathogenesis, and management. Eye (Lond). 2004 Nov. 18(11):1188-206. [QxMD MEDLINE Link].
Lessell S. Optic neuropathy in giant cell arteritis. J Neuroophthalmol. 2005 Sep. 25(3):247. [QxMD MEDLINE Link].
McFadzean RM. Ischemic optic neuropathy and giant cell arteritis. Curr Opin Ophthalmol. 1998 Dec. 9(6):10-7. [QxMD MEDLINE Link].
Rucker JC, Biousse V, Newman NJ. Ischemic optic neuropathies. Curr Opin Neurol. 2004 Feb. 17(1):27-35. [QxMD MEDLINE Link].
WAGENER HP, HOLLENHORST RW. The ocular lesions of temporal arteritis. Am J Ophthalmol. 1958 May. 45 (5):617-30. [QxMD MEDLINE Link].
Saha N, Rehman SU. Reversal of chronic ocular ischaemia with good visual recovery in giant cell arteritis. Eye (Lond). 2006 Jun. 20(6):742-3. [QxMD MEDLINE Link].
Schäuble B, Wijman CA, Koleini B, Babikian VL. Ophthalmic artery microembolism in giant cell arteritis. J Neuroophthalmol. 2000 Dec. 20(4):273-5. [QxMD MEDLINE Link].
Schmidt D. Ocular ichemia syndrome - a malignant course of giant cell arteritis. Eur J Med Res. 2005 Jun 22. 10(6):233-42. [QxMD MEDLINE Link].
Tovilla-Canales JL. Ocular manifestations of giant cell arteritis. Curr Opin Ophthalmol. 1998 Dec. 9(6):73-9. [QxMD MEDLINE Link].
Al-Abdulla NA, Kelley JS, Green WR, Miller NR. Herpes zoster vasculitis presenting as giant cell arteritis with choroidal infarction. Retina. 2003 Aug. 23(4):567-9. [QxMD MEDLINE Link].
Casson RJ, Fleming FK, Shaikh A, James B. Bilateral ocular ischemic syndrome secondary to giant cell arteritis. Arch Ophthalmol. 2001 Feb. 119(2):306-7. [QxMD MEDLINE Link].
Velusami P, Doherty M, Gnanaraj L. A case of occult giant cell arteritis presenting with bilateral cotton wool spots. Eye (Lond). 2006 Jul. 20(7):863-4. [QxMD MEDLINE Link].
Wein FB, Miller NR. Unilateral central retinal artery occlusion followed by contralateral anterior ischemic optic neuropathy in giant cell arteritis. Retina. 2000. 20(3):301-3. [QxMD MEDLINE Link].
Borg FA, Salter VL, Dasgupta B. Neuro-ophthalmic complications in giant cell arteritis. Curr Allergy Asthma Rep. 2008 Jul. 8(4):323-30. [QxMD MEDLINE Link].
Killer HE, Holtz DJ, Kaiser HJ, Laeng RH. Diplopia, ptosis, and hepatitis as presenting signs and symptoms of giant cell arteritis. Br J Ophthalmol. 2000 Nov. 84(11):1319-20. [QxMD MEDLINE Link]. [Full Text].
Ahmad I, Zaman M. Bilateral internuclear ophthalmoplegia: an initial presenting sign of giant cell arteritis. J Am Geriatr Soc. 1999 Jun. 47(6):734-6. [QxMD MEDLINE Link].
Foroozan R, Buono LM, Savino PJ, Sergott RC. Tonic pupils from giant cell arteritis. Br J Ophthalmol. 2003 Apr. 87(4):510-2. [QxMD MEDLINE Link]. [Full Text].
Maksimowicz-McKinnon K, Clark TM, Hoffman GS. Takayasu arteritis and giant cell arteritis: a spectrum within the same disease?. Medicine (Baltimore). 2009 Jul. 88(4):221-6. [QxMD MEDLINE Link].
Audemard A, Boutemy J, Galateau-Salle F, Macro M, Bienvenu B. AL amyloidosis with temporal artery involvement simulates giant-cell arteritis. Joint Bone Spine. 2012 Mar. 79(2):195-7. [QxMD MEDLINE Link].
Ing EB, Miller NR, Nguyen A, Su W, Bursztyn LLCD, Poole M, et al. Neural network and logistic regression diagnostic prediction models for giant cell arteritis: development and validation. Clin Ophthalmol. 2019. 13:421-430. [QxMD MEDLINE Link].
Ing EB, Lahaie Luna G, Toren A, Ing R, Chen JJ, Arora N, et al. Multivariable prediction model for suspected giant cell arteritis: development and validation. Clin Ophthalmol. 2017. 11:2031-2042. [QxMD MEDLINE Link].
Wise CM, Agudelo CA, Chmelewski WL, McKnight KM. Temporal arteritis with low erythrocyte sedimentation rate: a review of five cases. Arthritis Rheum. 1991 Dec. 34(12):1571-4. [QxMD MEDLINE Link].
Salvarani C, Hunder GG. Giant cell arteritis with low erythrocyte sedimentation rate: frequency of occurence in a population-based study. Arthritis Rheum. 2001 Apr. 45(2):140-5. [QxMD MEDLINE Link].
Hayreh SS, Podhajsky PA, Raman R, Zimmerman B. Giant cell arteritis: validity and reliability of various diagnostic criteria. Am J Ophthalmol. 1997 Mar. 123(3):285-96. [QxMD MEDLINE Link].
Costello F, Zimmerman MB, Podhajsky PA, Hayreh SS. Role of thrombocytosis in diagnosis of giant cell arteritis and differentiation of arteritic from non-arteritic anterior ischemic optic neuropathy. Eur J Ophthalmol. 2004 May-Jun. 14(3):245-57. [QxMD MEDLINE Link].
Parikh M, Miller NR, Lee AG, Savino PJ, Vacarezza MN, Cornblath W, et al. Prevalence of a normal C-reactive protein with an elevated erythrocyte sedimentation rate in biopsy-proven giant cell arteritis. Ophthalmology. 2006 Oct. 113(10):1842-5. [QxMD MEDLINE Link].
van der Geest KS, Abdulahad WH, Rutgers A, Horst G, Bijzet J, Arends S, et al. Serum markers associated with disease activity in giant cell arteritis and polymyalgia rheumatica. Rheumatology (Oxford). 2015 Aug. 54 (8):1397-402. [QxMD MEDLINE Link].
Gonzalez-Gay MA, Lopez-Diaz MJ, Barros S, Garcia-Porrua C, Sanchez-Andrade A, Paz-Carreira J, et al. Giant cell arteritis: laboratory tests at the time of diagnosis in a series of 240 patients. Medicine (Baltimore). 2005 Sep. 84(5):277-90. [QxMD MEDLINE Link].
Walvick MD, Walvick MP. Giant cell arteritis: laboratory predictors of a positive temporal artery biopsy. Ophthalmology. 2011 Jun. 118(6):1201-4. [QxMD MEDLINE Link].
Ellen H, Nusser J. Which clinical features and lab findings increase the likelihood of temporal arteritis?. The Journal of Family Practice. 2008. 57:119-120.
Murgatroyd H, Nimmo M, Evans A, MacEwen C. The use of ultrasound as an aid in the diagnosis of giant cell arteritis: a pilot study comparing histological features with ultrasound findings. Eye (Lond). 2003 Apr. 17(3):415-9. [QxMD MEDLINE Link].
Alberts MS, Mosen DM. Diagnosing temporal arteritis: duplex vs. biopsy. QJM. 2007 Dec. 100(12):785-9. [QxMD MEDLINE Link].
Karahaliou M, Vaiopoulos G, Papaspyrou S, Kanakis MA, Revenas K, Sfikakis PP. Colour duplex sonography of temporal arteries before decision for biopsy: a prospective study in 55 patients with suspected giant cell arteritis. Arthritis Res Ther. 2006. 8(4):R116. [QxMD MEDLINE Link]. [Full Text].
Ball EL, Walsh SR, Tang TY, Gohil R, Clarke JM. Role of ultrasonography in the diagnosis of temporal arteritis. Br J Surg. 2010 Dec. 97(12):1765-71. [QxMD MEDLINE Link].
Charlton R. Optimal management of giant cell arteritis and polymyalgia rheumatica. Ther Clin Risk Manag. 2012. 8:173-9. [QxMD MEDLINE Link]. [Full Text].
Diamantopoulos AP, Haugeberg G, Lindland A, Myklebust G. The fast-track ultrasound clinic for early diagnosis of giant cell arteritis significantly reduces permanent visual impairment: towards a more effective strategy to improve clinical outcome in giant cell arteritis?. Rheumatology (Oxford). 2016 Jan. 55 (1):66-70. [QxMD MEDLINE Link].
Duftner C, Dejaco C, Sepriano A, Falzon L, Schmidt WA, Ramiro S. Imaging in diagnosis, outcome prediction and monitoring of large vessel vasculitis: a systematic literature review and meta-analysis informing the EULAR recommendations. RMD Open. 2018. 4 (1):e000612. [QxMD MEDLINE Link]. [Full Text].
Schäfer VS, Chrysidis S, Dejaco C, Duftner C, Iagnocco A, et al. Assessing Vasculitis in Giant Cell Arteritis by Ultrasound: Results of OMERACT Patient-based Reliability Exercises. J Rheumatol. 2018 Jul 1. [QxMD MEDLINE Link].
Luqmani R, Lee E, Singh S, Gillett M, Schmidt WA, Bradburn M, et al. The Role of Ultrasound Compared to Biopsy of Temporal Arteries in the Diagnosis and Treatment of Giant Cell Arteritis (TABUL): a diagnostic accuracy and cost-effectiveness study. Health Technol Assess. 2016 Nov. 20 (90):1-238. [QxMD MEDLINE Link]. [Full Text].
Suelves AM, España-Gregori E, Tembl J, Rohrweck S, Millán JM, Díaz-Llopis M. Doppler ultrasound and giant cell arteritis. Clin Ophthalmol. 2010 Nov 25. 4:1383-4. [QxMD MEDLINE Link]. [Full Text].
Bley TA, Reinhard M, Hauenstein C, Markl M, Warnatz K, Hetzel A, et al. Comparison of duplex sonography and high-resolution magnetic resonance imaging in the diagnosis of giant cell (temporal) arteritis. Arthritis Rheum. 2008 Aug. 58(8):2574-8. [QxMD MEDLINE Link].
Koenigkam-Santos M, Sharma P, Kalb B, Oshinski JN, Weyand CM, Goronzy JJ, et al. Magnetic resonance angiography in extracranial giant cell arteritis. J Clin Rheumatol. 2011 Sep. 17(6):306-10. [QxMD MEDLINE Link].
Ghinoi A, Pipitone N, Nicolini A, Boiardi L, Silingardi M, Germanò G, et al. Large-vessel involvement in recent-onset giant cell arteritis: a case-control colour-Doppler sonography study. Rheumatology (Oxford). 2012 Apr. 51(4):730-4. [QxMD MEDLINE Link].
Brannan SO, Cheung D, Murray PI, Dewar C, Guest P. The use of magnetic resonance imaging in the diagnosis of suspected giant cell arteritis. Br J Ophthalmol. 2004 Dec. 88(12):1595-6. [QxMD MEDLINE Link]. [Full Text].
Garcia-Porrua C, Santamarina R, Armesto V, Gonzalez-Gay MA. Magnetic resonance imaging in optic neuritis due to giant cell arteritis. Arthritis Rheum. 2005 Apr 15. 53(2):313-4. [QxMD MEDLINE Link].
Khoury JA, Hoxworth JM, Mazlumzadeh M, Wellik KE, Wingerchuk DM, Demaerschalk BM. The clinical utility of high resolution magnetic resonance imaging in the diagnosis of giant cell arteritis: a critically appraised topic. Neurologist. 2008 Sep. 14(5):330-5. [QxMD MEDLINE Link].
Rhéaume M, Rebello R, Pagnoux C, Carette S, Clements-Baker M, Cohen-Hallaleh V, et al. High-resolution Magnetic Resonance Imaging of scalp arteries for the diagnosis of giant cell arteritis: Results of a prospective cohort study. Arthritis Rheumatol. 2016 Aug 2. [QxMD MEDLINE Link].
Daumas A, Scafi M, Jean E, Andrianasolo M, Cammilleri S, Benyamine A, et al. Fluorine-18 Fluorodeoxyglucose Positron Emission Tomography Hypermetabolism of Vertebral Arteries Revealing Giant Cell Arteritis. Am J Med. 2015 Jul. 128 (7):e1-2. [QxMD MEDLINE Link].
Nielsen BD, Hansen IT, Kramer S, Haraldsen A, Hjorthaug K, Bogsrud TV, et al. Simple dichotomous assessment of cranial artery inflammation by conventional 18F-FDG PET/CT shows high accuracy for the diagnosis of giant cell arteritis: a case-control study. Eur J Nucl Med Mol Imaging. 2018 Jul 31. [QxMD MEDLINE Link].
[Guideline] Dejaco C, Ramiro S, Duftner C, Besson FL, Bley TA, Blockmans D, et al. EULAR recommendations for the use of imaging in large vessel vasculitis in clinical practice. Ann Rheum Dis. 2018 May. 77 (5):636-643. [QxMD MEDLINE Link]. [Full Text].
Murchison AP, Gilbert ME, Bilyk JR, Eagle RC Jr, Pueyo V, Sergott RC, et al. Validity of the American College of Rheumatology criteria for the diagnosis of giant cell arteritis. Am J Ophthalmol. 2012 Oct. 154 (4):722-9. [QxMD MEDLINE Link].
Niederkohr RD, Levin LA. A Bayesian analysis of the true sensitivity of a temporal artery biopsy. Invest Ophthalmol Vis Sci. 2007 Feb. 48(2):675-80. [QxMD MEDLINE Link].
Pountain G, Hazleman B. ABC of rheumatology. Polymyalgia rheumatica and giant cell arteritis. BMJ. 1995 Apr 22. 310(6986):1057-9. [QxMD MEDLINE Link]. [Full Text].
Ray-Chaudhuri N, Kiné DA, Tijani SO, Parums DV, Cartlidge N, Strong NP, et al. Effect of prior steroid treatment on temporal artery biopsy findings in giant cell arteritis. Br J Ophthalmol. 2002 May. 86(5):530-2. [QxMD MEDLINE Link]. [Full Text].
Ing EB, Wang DN, Kirubarajan A, Benard-Seguin E, Ma J, Farmer JP, et al. Systematic Review of the Yield of Temporal Artery Biopsy for Suspected Giant Cell Arteritis. Neuroophthalmology. 2019 Feb. 43 (1):18-25. [QxMD MEDLINE Link].
Mahr A, Saba M, Kambouchner M, Polivka M, Baudrimont M, Brochériou I, et al. Temporal artery biopsy for diagnosing giant cell arteritis: the longer, the better?. Ann Rheum Dis. 2006 Jun. 65 (6):826-8. [QxMD MEDLINE Link].
Ypsilantis E, Courtney ED, Chopra N, Karthikesalingam A, Eltayab M, Katsoulas N, et al. Importance of specimen length during temporal artery biopsy. Br J Surg. 2011 Nov. 98 (11):1556-60. [QxMD MEDLINE Link].
Oh LJ, Wong E, Gill AJ, McCluskey P, Smith JEH. Value of temporal artery biopsy length in diagnosing giant cell arteritis. ANZ J Surg. 2018 Mar. 88 (3):191-195. [QxMD MEDLINE Link].
Kling J. Researchers Home In on Optimal Biopsy Length for Giant Cell Arteritis. Medscape Medical News. Available at https://www.medscape.com/viewarticle/936665. Accessed: September 3, 2020.
Chu R, Foster C, Mohsin A, et al. Optimal length and usefulness of temporal artery biopsies in the diagnosis of giant cell arteritis: a 10-year retrospective review of medical records. Lancet Rheumatol. August 20, 2020. [Full Text].
Boyev LR, Miller NR, Green WR. Efficacy of unilateral versus bilateral temporal artery biopsies for the diagnosis of giant cell arteritis. Am J Ophthalmol. 1999 Aug. 128(2):211-5. [QxMD MEDLINE Link].
Danesh-Meyer HV, Savino PJ, Eagle RC Jr, Kubis KC, Sergott RC. Low diagnostic yield with second biopsies in suspected giant cell arteritis. J Neuroophthalmol. 2000 Sep. 20(3):213-5. [QxMD MEDLINE Link].
Hall JK, Volpe NJ, Galetta SL, Liu GT, Syed NA, Balcer LJ. The role of unilateral temporal artery biopsy. Ophthalmology. 2003 Mar. 110(3):543-8; discussion 548. [QxMD MEDLINE Link].
Pless M, Rizzo JF 3rd, Lamkin JC, Lessell S. Concordance of bilateral temporal artery biopsy in giant cell arteritis. J Neuroophthalmol. 2000 Sep. 20(3):216-8. [QxMD MEDLINE Link].
Riordan-Eva P, Landau K, O'Day J. Temporal artery biopsy in the management of giant cell arteritis with neuro-ophthalmic complications. Br J Ophthalmol. 2001 Oct. 85(10):1248-51. [QxMD MEDLINE Link]. [Full Text].
Armstrong AT, Tyler WB, Wood GC, Harrington TM. Clinical importance of the presence of giant cells in temporal arteritis. J Clin Pathol. 2008 May. 61(5):669-71. [QxMD MEDLINE Link].
Marí B, Monteagudo M, Bustamante E, Pérez J, Casanovas A, Jordana R, et al. Analysis of temporal artery biopsies in an 18-year period at a community hospital. Eur J Intern Med. 2009 Sep. 20(5):533-6. [QxMD MEDLINE Link].
de Boysson H, Boutemy J, Creveuil C, Ollivier Y, Letellier P, Pagnoux C, et al. Is there a place for cyclophosphamide in the treatment of giant-cell arteritis? A case series and systematic review. Semin Arthritis Rheum. 2013 Aug. 43(1):105-12. [QxMD MEDLINE Link].
Ing EB, Philteos J, Sholohov G, Kim DT, Nijhawan N, Mark PW, et al. Local anesthesia and anxiolytic techniques for oculoplastic surgery. Clin Ophthalmol. 2019. 13:153-160. [QxMD MEDLINE Link].
Wolff K et al. Fig 243-4. Fitzpatrick’s Dermatology In General Medicine. 7th. 2008. 2291.
Murchison AP, Bilyk JR, Eagle RC, et al. Shrinkage Revisited: How Long Is Long Enough?. Ophth Plas & Reconstructive Surg. May 2012 21;epub ahead of print.
Reinhard M, Schmidt D, Schumacher M, Hetzel A. Involvement of the vertebral arteries in giant cell arteritis mimicking vertebral dissection. J Neurol. 2003 Aug. 250(8):1006-9. [QxMD MEDLINE Link].
De Miguel E, Roxo A, Castillo C, Peiteado D, Villalba A, Martín-Mola E. The utility and sensitivity of colour Doppler ultrasound in monitoring changes in giant cell arteritis. Clin Exp Rheumatol. 2012 Jan-Feb. 30(1 Suppl 70):S34-8. [QxMD MEDLINE Link].
Calabrese LH. Clinical management issues in vasculitis. Angiographically defined angiitis of the central nervous system: diagnostic and therapeutic dilemmas. Clin Exp Rheumatol. 2003 Nov-Dec. 21(6 Suppl 32):S127-30. [QxMD MEDLINE Link].
Warrington KJ, Matteson EL. Management guidelines and outcome measures in giant cell arteritis (GCA). Clin Exp Rheumatol. 2007 Nov-Dec. 25(6 Suppl 47):137-41. [QxMD MEDLINE Link].
Salvarani C, Giannini C, Miller DV, Hunder G. Giant cell arteritis: Involvement of intracranial arteries. Arthritis Rheum. 2006 Dec 15. 55(6):985-9. [QxMD MEDLINE Link].
Weyand CM, Fulbright JW, Hunder GG, Evans JM, Goronzy JJ. Treatment of giant cell arteritis: interleukin-6 as a biologic marker of disease activity. Arthritis Rheum. 2000 May. 43(5):1041-8. [QxMD MEDLINE Link].
Matteson EL, Buttgereit F, Dejaco C, Dasgupta B. Glucocorticoids for Management of Polymyalgia Rheumatica and Giant Cell Arteritis. Rheum Dis Clin North Am. 2016 Feb. 42 (1):75-90, viii. [QxMD MEDLINE Link].
Fraser JA, Weyand CM, Newman NJ, Biousse V. The treatment of giant cell arteritis. Rev Neurol Dis. 2008 Summer. 5(3):140-52. [QxMD MEDLINE Link]. [Full Text].
Mazlumzadeh M, Hunder GG, Easley KA, Calamia KT, Matteson EL, Griffing WL, et al. Treatment of giant cell arteritis using induction therapy with high-dose glucocorticoids: a double-blind, placebo-controlled, randomized prospective clinical trial. Arthritis Rheum. 2006 Oct. 54(10):3310-8. [QxMD MEDLINE Link].
Prieto-González S, García-Martínez A, Arguis P, Cid MC. Early improvement of radiological signs of large-vessel inflammation in giant cell arteritis upon glucocorticoid treatment. Rheumatology (Oxford). 2013 Jul. 52(7):1335-6. [QxMD MEDLINE Link].
Nesher G, Berkun Y, Mates M, Baras M, Rubinow A, Sonnenblick M. Low-dose aspirin and prevention of cranial ischemic complications in giant cell arteritis. Arthritis Rheum. 2004 Apr. 50(4):1332-7. [QxMD MEDLINE Link].
[Guideline] Mackie SL, Dejaco C, Appenzeller S, et al. British Society for Rheumatology guideline on diagnosis and treatment of giant cell arteritis: executive summary. Rheumatology (Oxford). 2020 Mar 1. 59 (3):487-494. [QxMD MEDLINE Link]. [Full Text].
Chan CC, Paine M, O'day J. Predictors of recurrent ischemic optic neuropathy in giant cell arteritis. J Neuroophthalmol. 2005 Mar. 25(1):14-7. [QxMD MEDLINE Link].
Kim N, Trobe JD, Flint A, Keoleian G. Late ipsilateral recurrence of ischemic optic neuropathy in giant cell arteritis. J Neuroophthalmol. 2003 Jun. 23(2):122-6. [QxMD MEDLINE Link].
Durand M, Thomas SL. Incidence of infections in patients with giant cell arteritis: a cohort study. Arthritis Care Res (Hoboken). 2012 Apr. 64(4):581-8. [QxMD MEDLINE Link].
Villiger PM, Adler S, Kuchen S, Wermelinger F, Dan D, Fiege V, et al. Tocilizumab for induction and maintenance of remission in giant cell arteritis: a phase 2, randomised, double-blind, placebo-controlled trial. Lancet. 2016 May 7. 387 (10031):1921-7. [QxMD MEDLINE Link].
Stone JH, Tuckwell K, Dimonaco S, Klearman M, Aringer M, Blockmans D, et al. Efficacy and Safety of Tocilizumab in Patients with Giant Cell Arteritis: Primary and Secondary Outcomes from a Phase 3, Randomized, Double-Blind, Placebo-Controlled Trial [abstract]. Arthritis Rheumatol. 2016. 68(suppl 10):[Full Text].
FDA approves first drug to specifically treat giant cell arteritis. U.S. Food & Drug Administration. Available at https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm559791.htm. May 22, 2017; Accessed: May 23, 2017.
Loricera J, Blanco R, Hernández JL, Castañeda S, Mera A, et al. Tocilizumab in giant cell arteritis: Multicenter open-label study of 22 patients. Semin Arthritis Rheum. 2015 Jun. 44 (6):717-23. [QxMD MEDLINE Link].
Hoffman GS, Cid MC, Rendt-Zagar KE, Merkel PA, Weyand CM, Stone JH, et al. Infliximab for maintenance of glucocorticosteroid-induced remission of giant cell arteritis: a randomized trial. Ann Intern Med. 2007 May 1. 146(9):621-30. [QxMD MEDLINE Link].
Martínez-Taboada VM, Rodríguez-Valverde V, Carreño L, López-Longo J, Figueroa M, Belzunegui J, et al. A double-blind placebo controlled trial of etanercept in patients with giant cell arteritis and corticosteroid side effects. Ann Rheum Dis. 2008 May. 67(5):625-30. [QxMD MEDLINE Link].
Ly KH, Dalmay F, Gondran G, Palat S, Bezanahary H, Cypierre A, et al. Steroid-sparing effect and toxicity of dapsone treatment in giant cell arteritis: A single-center, retrospective study of 70 patients. Medicine (Baltimore). 2016 Oct. 95 (42):e4974. [QxMD MEDLINE Link].
De Silva M, Hazleman BL. Azathioprine in giant cell arteritis/polymyalgia rheumatica: a double-blind study. Ann Rheum Dis. 1986 Feb. 45(2):136-8. [QxMD MEDLINE Link]. [Full Text].
Taylor-Gjevre R, Vo M, Shukla D, Resch L. Temporal artery biopsy for giant cell arteritis. J Rheumatol. 2005 Jul. 32(7):1279-82. [QxMD MEDLINE Link].
Mahr AD, Jover JA, Spiera RF, Hernández-García C, Fernández-Gutiérrez B, Lavalley MP, et al. Adjunctive methotrexate for treatment of giant cell arteritis: an individual patient data meta-analysis. Arthritis Rheum. 2007 Aug. 56(8):2789-97. [QxMD MEDLINE Link].
Hoffman GS, Cid MC, Hellmann DB, Guillevin L, Stone JH, Schousboe J, et al. A multicenter, randomized, double-blind, placebo-controlled trial of adjuvant methotrexate treatment for giant cell arteritis. Arthritis Rheum. 2002 May. 46(5):1309-18. [QxMD MEDLINE Link].
Caporali R, Cimmino MA, Ferraccioli G, Gerli R, Klersy C, Salvarani C, et al. Prednisone plus methotrexate for polymyalgia rheumatica: a randomized, double-blind, placebo-controlled trial. Ann Intern Med. 2004 Oct 5. 141(7):493-500. [QxMD MEDLINE Link].
Grossman JM, Gordon R, Ranganath VK, Deal C, Caplan L, Chen W, et al. American College of Rheumatology 2010 recommendations for the prevention and treatment of glucocorticoid-induced osteoporosis. Arthritis Care Res (Hoboken). 2010 Nov. 62(11):1515-26. [QxMD MEDLINE Link].
Guslandi M. Steroid ulcers: Any news?. World J Gastrointest Pharmacol Ther. 2013 Aug 6. 4(3):39-40. [QxMD MEDLINE Link]. [Full Text].
[Guideline] Maz M, Chung SA, Abril A, et al. 2021 American College of Rheumatology/Vasculitis Foundation Guideline for the Management of Giant Cell Arteritis and Takayasu Arteritis. Arthritis Rheumatol. 2021 Aug. 73 (8):1349-1365. [QxMD MEDLINE Link]. [Full Text].
[Guideline] Hellmich B, Agueda A, Monti S, et al. 2018 Update of the EULAR recommendations for the management of large vessel vasculitis. Ann Rheum Dis. 2020 Jan. 79 (1):19-30. [QxMD MEDLINE Link]. [Full Text].
 Prominent temporal artery is visible on the temple of a 76-year-old woman with temporal arteritis. Courtesy of ScienceSource (https://www.sciencesource.com/).
Prominent temporal artery is visible on the temple of a 76-year-old woman with temporal arteritis. Courtesy of ScienceSource (https://www.sciencesource.com/).
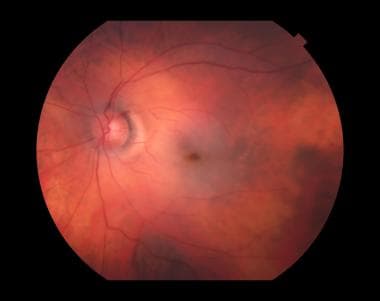
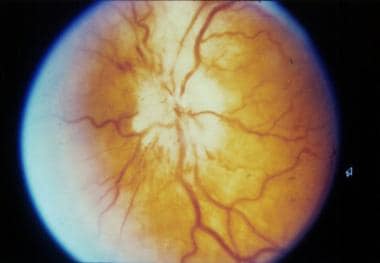 Anterior ischemic optic neuropathy. Image courtesy of Richard Kho, MD, Q.C. Eye Center, Quezon City, Philippines.
Anterior ischemic optic neuropathy. Image courtesy of Richard Kho, MD, Q.C. Eye Center, Quezon City, Philippines.