Practice Essentials
Placental abruption, or abruptio placentae, is the premature separation of a normally implanted placenta from the uterus. [1] Abruption may be categorized into 2 subtypes, revealed and concealed. In revealed abruption, the dissection occurs along the uterine wall and blood escapes through the cervix. In concealed abruption, blood is retained behind the placenta and does not communicate with the cervix. Furthermore, an abruption may be complete or partial, depending on the extent of placental detachment. Placental abruption complicates approximately 1% of pregnancies and is associated with increased maternal, fetal, and neonatal morbidity and mortality. [2, 3, 4]
A number of factors increase the risk for placental abruption, including smoking, alcohol or cocaine use during pregnancy, advanced maternal age, history of maternal hypertension, and preeclampsia. Women who have had a previous placental abruption have a higher risk in subsequent pregnancies, as do women with multiple gestational pregnancies. Trauma from a motor vehicle accident, a fall, or a blow to the abdomen may cause placental abruption. Domestic violence should be included in the differential diagnosis. [5, 6, 7, 8, 9]
(See the images of placental abruption below).
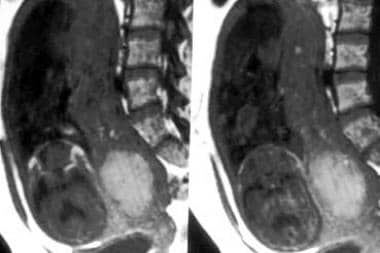
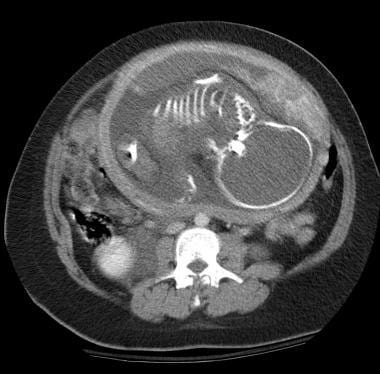 Placental ischemia: Contrast-enhanced CT image through the level of the placenta in a patient with acute trauma demonstrating an ischemic region affecting more than half of the visualized portion of the placenta. Ischemia was found to be secondary to placental abruption from a deceleration injury.
Placental ischemia: Contrast-enhanced CT image through the level of the placenta in a patient with acute trauma demonstrating an ischemic region affecting more than half of the visualized portion of the placenta. Ischemia was found to be secondary to placental abruption from a deceleration injury.
 Placental abruption: Fluid collection with a bright signal posterior to the placenta and just superior to the internal os in this T2-weighted sequence demonstrating a hyperacute hemorrhage.
Placental abruption: Fluid collection with a bright signal posterior to the placenta and just superior to the internal os in this T2-weighted sequence demonstrating a hyperacute hemorrhage.
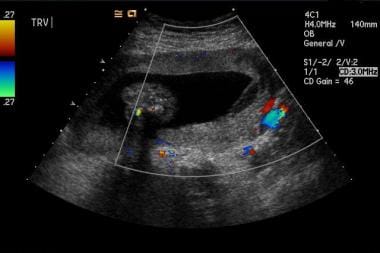 Marginal placental hemorrhage: Color Doppler flow image demonstrating the absence of flow in the retroplacental fluid collection.
Marginal placental hemorrhage: Color Doppler flow image demonstrating the absence of flow in the retroplacental fluid collection.
Preferred examination
Although radiologic, laboratory, and pathologic findings may assist in diagnosis, placental abruption is primarily diagnosed clinically. Patients presenting with vaginal bleeding, abdominal pain, history of trauma, or unexplained preterm labor should be assessed for abruption. To further assist the clinical diagnosis, radiologic imaging may be obtained; the choice of study depends on the clinical situation. Ultrasonography is usually the preferred study. The primary benefits of ultrasonography include avoiding ionizing radiation, the dynamic nature of the examination, and its speed and availability in most centers. In patients with severe trauma, CT scanning may be required to evaluate for abdominopelvic injuries. Although ionizing radiation poses an obvious fetal risk, in critical circumstances, its use may be vital to detect an underlying condition that jeopardizes the patient's life. [10, 11, 12, 13, 4, 14]
According to American College of Radiology guidelines, ultrasound FAST (focused assessment with sonography for trauma) scan of the chest, abdomen, and pelvis can be useful as a limited bedside adjunct to the physical examination and is primarily used for triage in a pregnant patient with major blunt trauma. Ultrasonography of the pelvis, CT of the abdomen and pelvis with IV contrast, CT of the whole body with IV contrast, or radiography trauma series is usually appropriate in addition to US FAST for the initial imaging of major blunt trauma in a pregnant patient. According to the ACR, these procedures are equivalent alternatives, so that only one of the procedures will be ordered to obtain clinical information. [15]
Computed Tomography
CT scanning is used to detect uterine rupture, placental separation, placental ischemia, and, occasionally, fetal injuries. In pregnant patients with blunt abdominal trauma, CT evaluation may be a highly sensitive and specific means of assessment, especially in unstable patients and in those with a high clinical suspicion for abdominopelvic injuries. [16, 17] However, because approximately 10-50 mGy of ionizing radiation is delivered to the patient and fetus during a pelvic CT scan, the use of this imaging modality must be carefully considered and weighed against the degree of clinical suspicion for abdominopelvic injuries, as well as the gestational age. [18, 19, 20, 21]
According to Wei and colleagues, [19] placental abruptions are often overlooked on CT scans, but the authors found that sensitivity can be improved by systematic evaluation of the placenta and that specificity can be improved by increased training regarding normal placenta pathology. In their study of 44 CT scans of pregnant women who presented with abdominal traumatic conditions, there were 7 placental abruptions, all of which were identified on CT scanning.
The risk of radiation-induced fetal effects is greatly reduced as gestational age increases. Undertake a risk assessment before obtaining a CT scan. If obtaining a helical CT examination, increase the scan pitch (ideal for reducing radiation dose).
(See the images below.)
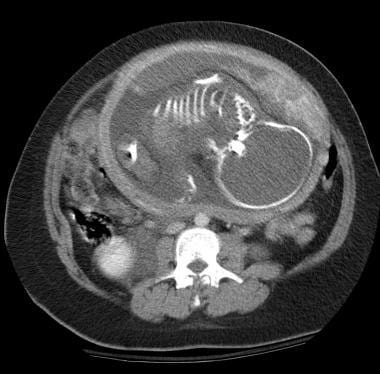 Placental ischemia: Contrast-enhanced CT image through the level of the placenta in a patient with acute trauma demonstrating an ischemic region affecting more than half of the visualized portion of the placenta. Ischemia was found to be secondary to placental abruption from a deceleration injury.
Placental ischemia: Contrast-enhanced CT image through the level of the placenta in a patient with acute trauma demonstrating an ischemic region affecting more than half of the visualized portion of the placenta. Ischemia was found to be secondary to placental abruption from a deceleration injury.
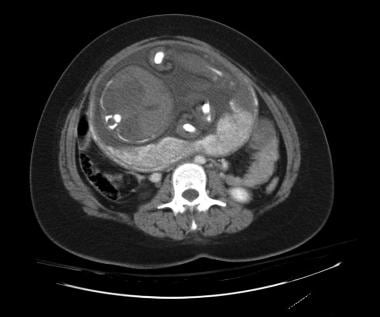 Placental ischemia: Contrast-enhanced CT image demonstrating a wedge-shaped region of ischemia in the lateral aspect of the placenta.
Placental ischemia: Contrast-enhanced CT image demonstrating a wedge-shaped region of ischemia in the lateral aspect of the placenta.
Magnetic Resonance Imaging
MRI is rarely used in the diagnosis and treatment of placental abruptions. Several factors limit its use in the evaluation of this acute, often critical, condition, including the length of scan time, the size limitation of the imaging chamber, the high susceptibility for motion artifact, and, occasionally, the high cost and lack of availability. Nonetheless, as MRI becomes ubiquitous and as more efficient imaging protocols are developed, MRI may serve an important function in the diagnosis of this condition. [22, 23, 24]
(See the images below.)
 Placental abruption: Fluid collection with a bright signal posterior to the placenta and just superior to the internal os in this T2-weighted sequence demonstrating a hyperacute hemorrhage.
Placental abruption: Fluid collection with a bright signal posterior to the placenta and just superior to the internal os in this T2-weighted sequence demonstrating a hyperacute hemorrhage.
 Placental hemorrhage: Large, oval-shaped bright collection in the inferior aspect of the placenta in this T2-weighted image demonstrating the hyperacute phase of hemorrhage within the placenta.
Placental hemorrhage: Large, oval-shaped bright collection in the inferior aspect of the placenta in this T2-weighted image demonstrating the hyperacute phase of hemorrhage within the placenta.
For abruption, MRI is best used to detect hematomatous collections and the physical separation of the placenta. Generally, placental ischemia cannot be accurately diagnosed with MRI.
Masselli et al studied the accuracy of ultrasound and MRI in 19 patients with abruption at delivery, and abruption was identified in 10 of 19 cases by ultrasound and in all 19 cases by MRI. According to the authors, MRI should be considered in cases of negative ultrasound findings when there is bleeding in late pregnancy if a diagnosis of abruption would result in a change in patient management. [23]
The appearance of hematomas on MRI widely varies, depends on age, and follows the same changes as hematomas in other parts of the body. The signal characteristics listed in the table below are based on conventional spin-echo techniques. Gradient-echo sequences may also be used to demonstrate blooming.
Table 1. MRI Signal Characteristics of Hematoma (Open Table in a new window)
Age |
Blood Products |
T1-signal |
T2-signal |
Hyperacute (0-1 d) |
Oxyhemoglobin |
Isointense |
Bright |
Acute (1-3 d) |
Deoxyhemoglobin |
Isointense |
Dark |
Early subacute (4-7 d) |
Intracellular methemoglobin |
Bright |
Dark |
Late subacute (>7 d) |
Extracellular methemoglobin |
Bright |
Bright |
Chronic (>2 wk) |
Hemosiderin |
Dark |
Dark |
Ultrasonography
In the evaluation of placental abruption, ultrasonography (see the images below) is the most accurate and practical radiologic study. The appearance of abruption on ultrasonography varies depending on the size, location, and time elapsed since onset of abruption. [10, 25, 26, 27, 28] Location and extent of abruption correlate with fetal mortality. The volume of the hematoma (estimated by [length × width × height]/2) and the amount of placental detachment are the most accurate predictors of pregnancy outcome. A hematoma larger than 50 mL or a placental detachment greater than 50% indicates a guarded prognosis.
The most common type of separation is a subchorionic hemorrhage; the least common is the preplacental. In a study of 57 instances of abruption, Nyberg et al reported subchorionic, retroplacental, and preplacental hemorrhage in 81%, 16%, and 4% of patients, respectively. They also reported a hyperechoic-to-isoechoic ultrasound appearance immediately following an abruption, which then became hypoechoic 1 week post abruption, and, finally, sonolucent 2 weeks post abruption. The jello sign may also be observed, in which the placenta jiggles when pressure is suddenly applied with the transducer. [29, 30]
Patients with fundal or corpus hematomas have a worse prognosis than those with supracervical hematomas. Fetal mortality is highest in retroplacental abruptions. The retroplacental hypoechoic complex (consisting of the uteroplacental vessels and myometrium) should be thinner than 1-2 cm. Consider a retroplacental hemorrhage or a uterine contraction if the complex is thicker. In addition, be aware of the potential to misinterpret hypoechoic fibroids as signs of placental separation.
 Marginal placental hemorrhage: Ultrasonographic image showing a hypoechoic fluid collection in the subchorionic region with extension into the retroplacental area.
Marginal placental hemorrhage: Ultrasonographic image showing a hypoechoic fluid collection in the subchorionic region with extension into the retroplacental area.
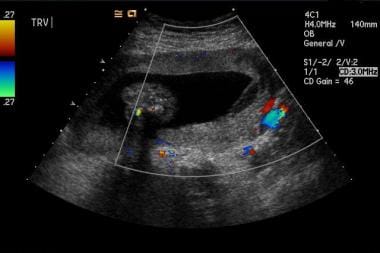 Marginal placental hemorrhage: Color Doppler flow image demonstrating the absence of flow in the retroplacental fluid collection.
Marginal placental hemorrhage: Color Doppler flow image demonstrating the absence of flow in the retroplacental fluid collection.
Ultrasonography has a low sensitivity but a high specificity for placental abruption. [31] According to Glantz and Purnell, the sensitivity, specificity, positive predictive values, and negative predictive values of ultrasonography are 24%, 96%, 88%, and 53%, respectively. [32] Most significantly, negative ultrasonographic results do not exclude abruption, while positive ultrasonographic results indicate a high probability of abruption.
If a diagnosis of placenta previa is made based on ultrasound, abruption is less likely to be the cause of the patient’s condition. However, other studies report different sensitivity rates. Sholl found a sensitivity of 25%, [33] while Jaffe et al reported a sensitivity of 50%. [25] Yeo et al evaluated 7 ultrasonographic parameters in a prospective cohort study of women with vaginal bleeding in the second trimester and reported a sensitivity of 80%, a specificity of 92%, a positive predictive value of 95%, and a negative predictive value of 69%. [34]
False positives or negatives
Several processes can be confused with a retroplacental hematoma on ultrasound. A retroplacental myometrial contraction can exert mass-effect upon the placenta. However, the contraction is transient and usually more homogeneous in appearance than a hematoma. A retroplacental mass such as a leiomyoma can also mimic a hematoma.
The normal subplacental vascular region is less echogenic than the placenta and can also mimic a hematoma. However, it does not have mass-effect on the placenta and may have visible vascular spaces.
Acute retroplacental hemorrhages can have similar echogenicity to overlying placenta and appear as a thickened placenta.
Subchorionic hemorrhages can resemble an elongated placenta or can mimic an intrauterine mass.
-
Placental ischemia: Contrast-enhanced CT image through the level of the placenta in a patient with acute trauma demonstrating an ischemic region affecting more than half of the visualized portion of the placenta. Ischemia was found to be secondary to placental abruption from a deceleration injury.
-
Placental ischemia: Contrast-enhanced CT image demonstrating a wedge-shaped region of ischemia in the lateral aspect of the placenta.
-
Healthy heterogeneous placenta: Contrast-enhanced CT demonstrating the typical degree of heterogeneity in the perfusion of the placenta. This pattern should not be mistaken for ischemia or abruption.
-
Placental abruption: Fluid collection with a bright signal posterior to the placenta and just superior to the internal os in this T2-weighted sequence demonstrating a hyperacute hemorrhage.
-
Placental hemorrhage: Large, oval-shaped bright collection in the inferior aspect of the placenta in this T2-weighted image demonstrating the hyperacute phase of hemorrhage within the placenta.
-
Marginal placental hemorrhage: Ultrasonographic image showing a hypoechoic fluid collection in the subchorionic region with extension into the retroplacental area.
-
Marginal placental hemorrhage.
-
Marginal placental hemorrhage: Color Doppler flow image demonstrating the absence of flow in the retroplacental fluid collection.










