Overview
An oral nerve block is a simple and effective way to manage orofacial pain without distorting the anatomy of a wound and without the use of narcotics. (See the image below of an inferior alveolar nerve block.)
This article highlights the indications, equipment, contraindications, complications, and approach to performing the more commonly used oral nerve blocks. The technique section displays a step-by-step method for each block; illustrations depict the area to be anesthetized and the position of the needle in relation to the anatomy.
Indications
Indications include the following:
-
Toothache, pulpitis, or root impaction
-
Postextraction pain, including dry socket
-
Mandibular and maxillary fractures
Contraindications
Contraindications include the following:
-
Hypersensitivity or allergy to local anesthetic agents
-
Distortion of landmarks needed to perform the nerve block
-
Patient who are uncooperative because of anxiety, altered mental status, or any other reason (Procedural sedation may be necessary to minimize risk to the clinician and patient. )
-
Injecting through infected tissue (Anesthetics are less effective in infected tissue and can cause bacteremia or spread infection to adjacent tissues, planes, or bone, which can be extremely difficult to treat. Use only superficial or local anesthesia in these cases. [1] )
-
Presence of cardiac disease, including valves, congenital abnormalities, and previous surgeries (These patients need prophylaxis to prevent endocarditis.)
-
History of bleeding disorder or coagulopathy
-
Preexisting neurologic damage (This should be documented well but should not deter the clinician from treating the patient.)
Anesthesia
Topical anesthetics
Topical anesthetics are as follows:
-
Topical anesthetics are used to reduce the pain caused by needle insertion.
-
Commonly used topical anesthetics include the following:
Benzocaine 20% (eg, Hurricaine spray, Orajel): Use caution and monitor patient for methemoglobinemia.
Lidocaine 5% solution (applied topically)
-
Application of topical anesthesia for oral nerve block is as follows: [2]
Dry the mucous membranes with gauze over the site to be anesthetized.
Place a generous amount of topical agent onto cotton-tipped applicators.
Apply the topical agent over the mucosa for approximately 3 minutes.
*NOTE: Do not use tetracaine/Adrenalin/cocaine (TAC) or other cutaneous preparations on mucous membranes; severe systemic toxicity can result. For more information, see Anesthesia, Topical.
Local anesthetics
Local anesthetics are as follows:
-
Lidocaine (1% or 2%) and bupivacaine (0.25%) are the 2 most commonly used local anesthetics.
Lidocaine is preferred for indications such as laceration repair because of its shorter duration of action.
Bupivacaine is preferred for indications such as toothache or mandibular fracture because of its longer duration of action.
-
Note that anesthetics are divided into 2 classes: amide and ester. These can be substituted for each other if the patient has an allergy to one type. For more information, see Local Anesthetic Agents, Infiltrative Administration.
-
Avoid using local anesthetics in at-risk patients (eg, those with cardiovascular disease). For more information, including local anesthetic toxicity, see Toxicity, Local Anesthetics.
-
For information on calculating appropriate amounts of local anesthetic/epinephrine, please refer to the Calculating Concentrations and Dilutions section below.
-
A study investigated the anaesthetic efficacy, duration of action, pain, pulpal anaesthesia, and cardiovascular effects of 0.5% ropivacaine. The study concluded that 0.5% ropivacaine alone does not affect the cardiovascular system and ropivacaine can be useful for oral and maxillofacial surgeons who are looking for a local anaesthetic with minimal cardiovascular risk and without a vasoconstrictor to provide regional anaesthesia for long procedures. [5]
Equipment
Equipment includes the following:
-
Syringe, 3 mL, or aspirating dental syringe
-
Needle, 25-27 gauge, 1.5-2.0 inch
-
Anesthetic (local and topical)
-
Nonsterile gloves
-
4 X 4 gauze
-
Cotton-tipped applicators
-
Suction source, tubing, Yankauer suction catheter
-
Light source
-
One of the following antiseptic mouth rinses:
Hydrogen peroxide
Chlorhexidine (0.5%) with ethanol (7%)
Povidone iodine (Betadine)
Chlorhexidine (Peridex) 0.12% (This mouth rinse is recommended by some texts but is not an absolute necessity. [6] )
Positioning
Positioning is as follows:
-
To perform an oral nerve block, the patient should be supine, reclined to approximately 75 degrees. [6]
A prospective, randomized study reported that for inferior alveolar nerve block, the supine position improved success in the second premolars (63% vs 53%) and first premolars (75% vs 64%) when compared to the upright position; however, no statistical difference was seen for the supine position in the second molars (73% vs 65%), first molars (59% vs 54%), lateral incisors (28% vs 23%), and central incisors (11% vs 8%). [7]
-
For some particular nerve blocks, however, patients should be positioned differently as follows: [6]
Inferior alveolar nerve block: For this procedure, the patient should be seated, with the head firmly against the head rest, positioned so that when the mandible is open, the body of the mandible is parallel to the floor.
Nasopalatine and greater palatine nerve blocks: For these procedures, place a rolled sheet beneath the patient’s shoulders to assist in neck extension of 45 degrees.
Technique
Supraperiosteal infiltrations
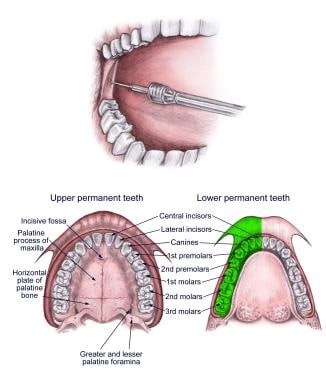
A supraperiosteal infiltration anesthetizes individual teeth (see image below). Use this technique only with the maxillary incisors, canines, and premolars. [2, 6, 1]
Note the following:
Landmarks: Locate the mucobuccal fold above the tooth to be anesthetized by grasping the membrane with gauze and pulling out and down for maxillary locations and out and up for mandibular locations.
Apply topical anesthetic as described in the Anesthesia section.
Approach: Insert needle into the mucobuccal fold with the bevel facing bone, aligned with the center of the tooth to be anesthetized, aimed toward the maxilla. Contact the maxilla, then withdraw the needle 1 mm.
Aspirate.
Slowly inject 1-2 mL of local anesthetic at the apex of the root tip.
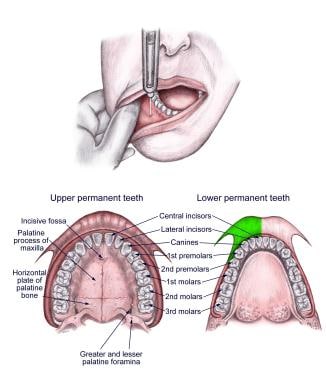
Anterior superior alveolar nerve block
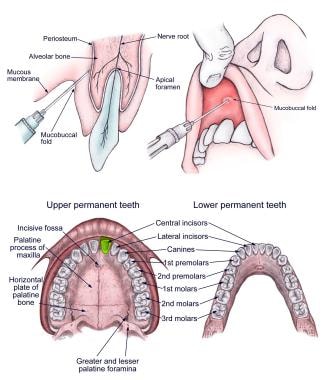
The anterior superior alveolar (ASA) nerve block anesthetizes the maxillary canine, the central and lateral incisors, and the mucosa above these teeth, with occasional crossover to the contralateral maxillary incisors (see image below). [2, 8]
Note the following:
Landmarks: Locate the mucobuccal fold where it intersects with the apex of the canine (cuspid) tooth by retracting the membrane with gauze and pulling out and down.
Apply topical anesthetic as described in the Anesthesia section.
Approach: While retracting the lip, insert the needle into the intersection of the mucobuccal fold and the apex/center of the canine at a 45-degree angle, advancing the needle approximately 1-1.5 cm.
Aspirate.
Slowly inject 2 mL of local anesthetic and massage for 10-20 seconds.
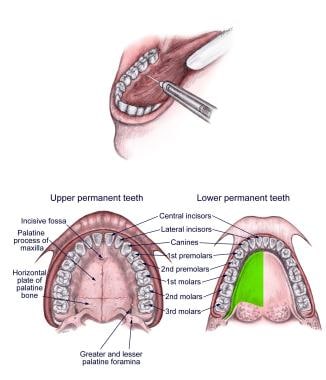
Middle superior alveolar nerve block
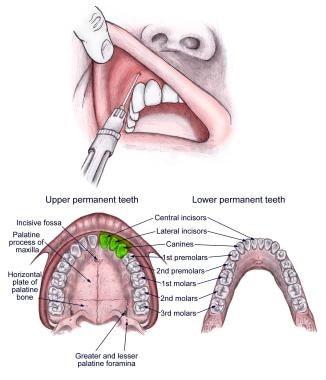
The middle superior alveolar (MSA) nerve block anesthetizes the maxillary premolars with occasional overlap to the canine and first molar (see image below). [2, 1, 8]
Note the following:
Landmarks: Locate the mucobuccal fold where it intersects with the junction of maxillary premolar 2 and molar 1.
Apply topical anesthetic as described in the Anesthesia section.
Approach: While retracting the cheek, insert the needle into the aforementioned intersection point at a 45-degree angle, and advance 1-1.5 cm.
Aspirate.
Slowly inject 2-3 mL of local anesthetic and massage for 10-20 seconds.
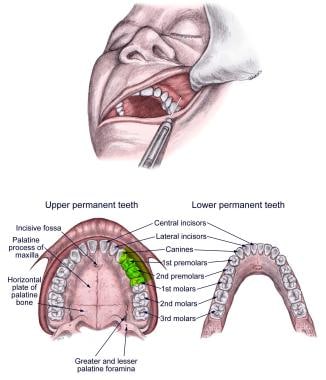
Posterior superior alveolar nerve block
The posterior superior alveolar (PSA) nerve block anesthetizes maxillary molar teeth (see image below). With the PSA nerve block, the first molar may not be completely anesthetized; in this case, the PSA nerve block can be used in conjunction with an MSA/supraperiosteal block. [2, 6, 1, 8]
Note the following:
Landmarks: Start with the jaw half open and swung toward the operator. Retract the cheek laterally and locate the intersection of the mucobuccal fold and the junction of molars 1 and 2.
Apply topical anesthetic as described in the Anesthesia section.
Approach: Insert the needle into the intersection and direct it toward the posterolateral maxillary tuberosity (up, back, and inward) along the curvature or the maxilla and to a depth of approximately 2-2.5 cm. If the needle contacts bone, withdraw and redirect more laterally.
Aspirate.
Slowly inject 2-3 mL of local anesthetic.
Infraorbital nerve block
An infraorbital nerve block, which branches from the maxillary nerve, anesthetizes the lower eyelid, upper cheek, part of the nose, and upper lip (see image below). The ASA nerve, which innervates the maxillary canine, the central and lateral incisors, and the mucosa above these teeth, with occasional crossover to the contralateral maxillary incisors, also branches from the maxillary nerve, proximal to the infraorbital nerve. [2, 6, 1, 8] Because of this anatomy, anesthetizing the infraorbital nerve can result in some overlapping anesthesia of the ASA nerve or vice versa. However, anesthetizing one of these nerves does not guarantee anesthesia of the other.
Note the following:
Landmarks: Externally, the intraorbital foramen is just medial to the intersection of a vertical line from the pupil (when midline) to the inferior border of the infraorbital ridge. Internally, the intraorbital foramen is approached at the intersection of the mucobuccal fold and the junction of premolars 1 and 2.
Apply topical anesthetic as described in the Anesthesia section.
Approach: Place the index finger of the nondominant hand over the above the intersection mentioned above (ie, the infraorbital foramen) and retract the cheek with the thumb. Insert the needle into the mucobuccal fold at junction of premolars 1 and 2. Direct the needle parallel to the long axis of premolar 2, palpating its location as the needle is advanced until it is adjacent to the infraorbital foramen (approximately 1.5-2 cm). If the needle is directed at an angle that is too acute, it will hit the maxillary eminence; if directed at an angle that is too superior, the needle will enter the orbit.
Aspirate.
Inject 2-3 mL of local anesthetic while holding firm pressure with the index finger over infraorbital ridge to prevent ballooning of lower eyelid. Massage for 10-20 seconds.
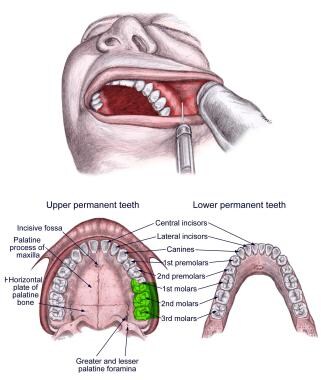
Nasopalatine nerve block
The nasopalatine nerve block anesthetizes the anterior hard palate and associated soft tissues (see image below). [6, 8]
Note the following:
Landmarks: The location for this injection is 0.5 cm posterior to the central incisors at the midline. Look for a slight soft tissue elevation; this is the incisive papilla, which overlies the incisive foramen.
Apply topical anesthetic as described in the Anesthesia section.
Approach: Insert needle with the bevel facing the hard palate just lateral to incisive papilla. Advance 3-4 mm medially or until the needle contacts bone.
Aspirate.
Inject 0.25-0.4 mL of local anesthetic. Do not inject more than this because it can cause separation of the mucosa from the palate and subsequent tissue necrosis.
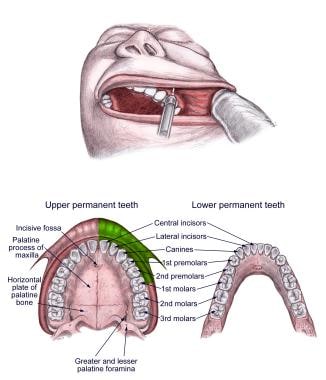
Greater palatine nerve block
Blocking the greater palatine nerve anesthetizes the posterior two thirds of the hard palate (see image below). [6, 8]
Note the following:
Landmarks: The greater palatine foramen can be identified by finding the junction of molars 2 and 3 and then moving the needle 1 cm medially.
Apply topical anesthetic as described in the Anesthesia section.
Approach: Insert the needle adjacent to the greater palatine foramen, at a 90-degree angle to the curvature of the hard palate. Do not advance further.
Aspirate.
Inject 0.3-0.5 mL of anesthetic. Do not inject more than this because it can cause separation of the mucosa from the palate and subsequent tissue necrosis.
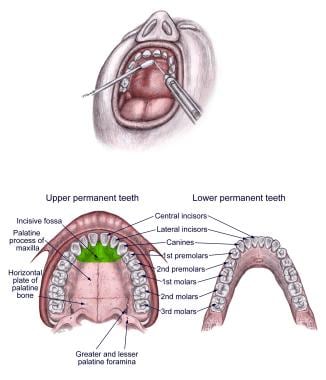
Inferior alveolar nerve block
An inferior alveolar nerve block anesthetizes all teeth on the ipsilateral side of mandible, as well as the ipsilateral lip and chin via the mental nerve (see image below). [2, 6, 1, 8]
Note the following:
Landmarks: Start by standing contralateral to the side to be anesthetized. Place the thumb in the mouth, and place the index finger externally and posterior to the ramus (angle of the jaw). Retract cheek laterally and palpate the retromolar fossa to find the greatest depth of the anterior border of the ramus; this is the coronoid notch.
Apply topical anesthetic as described in the Anesthesia section.
Approach: With the patient’s jaw open, align the barrel of the syringe with occlusive surfaces of the teeth, angled between the first and second premolars on contralateral side (the syringe must be thus aligned for a successful nerve block). Insert the needle 1 cm above the occlusive surface of the teeth in the triangle at the lingula. The lingula is a bony projection on the medial surface of the ramus 1 cm above the occlusive plain. The goal is to insert the needle just superior and posterior to the lingula; if the needle is inserted too low, anesthesia does not occur. Stop insertion when the needle strikes the bone but not before. Withdraw the needle 1-2 mm.
Aspirate.
Inject 2-4 mL of local anesthetic. Because of its close proximity to the inferior alveolar nerve, the lingual nerve is usually also anesthetized with this technique.
A study by Saha et al looked to determine the effect of administration of oral premedication with ketorolac (KETO) and diclofenac potassium (DP) on the efficacy of inferior alveolar nerve block in patients with irreversible pulpitis. The study found that oral premedication with 10 mg KETO resulted in significantly higher percentage of successful inferior alveolar block in patients with irreversible pulpitis than premedication with 50 mg DP and placebo. [9]
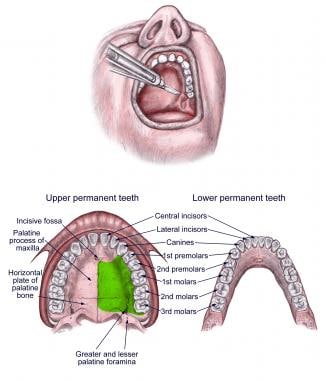
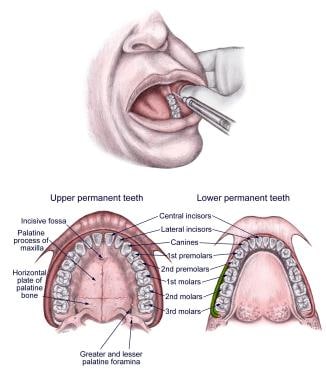
Mental nerve block
A mental nerve block anesthetizes the ipsilateral lower lip and skin of the chin (not the teeth; see image below). [2, 6, 1, 8]
Note the following:
Landmarks: To locate the mental foramen, retract the cheek and lip and locate the junction of mandibular premolars 1 and 2 and down 1 cm inferior to the gum line (just medial to the midline pupil). Note that this is in the same line as the infraorbital foramen.
Apply topical anesthetic as described in the Anesthesia section.
Approach: Insert the needle 1 cm inferior to the second premolar at a 45-degree angle. Advance until the needle contacts the mandible. Withdraw the needle slightly.
Aspirate.
Inject 1-2 mL of anesthetic adjacent to the foramen and massage for 10-20 seconds.
Lingual nerve block
The lingual nerve block anesthetizes the anterior two thirds of tongue (see image below). The lingual nerve also conveys chorda tympani from the facial nerve to provide taste to the anterior two thirds of the tongue and preganglionic fibers from chorda tympani to the submandibular ganglion and, in turn, the submandibular and sublingual glands. [6, 8]
A study that included 59 dental students who received an inferior alveolar nerve block injection reported the highest soft tissue anesthetic success rate on the lingual gingiva. [10]
Note the following:
Landmarks: The lingual nerve is located on the lingual side of the second mandibular molar.
Apply topical anesthetic as described in the Anesthesia section.
Approach: Stand on the contralateral side. Lift the tongue with a tongue blade and insert the needle 1 cm below the gumline of the second mandibular molar. Advance posteriorly 1 cm.
Aspirate.
Inject 1-1.5 mL of local anesthetic.
Buccal nerve block
The buccal nerve block anesthetizes the mucous membrane of the cheek and vestibule and, to a lesser extent, a small patch of skin on the face (see image below). [6, 8]
Note the following:
Landmarks: Locate the buccal nerve 1 mm lateral to mandibular molar 3 at the anterior border of the ramus in the occlusive plane.
Apply topical anesthetic as described in the Anesthesia section.
Approach: With the thumb of the nondominant hand, pull the cheek laterally. Insert the needle into the anterior border of the ramus 1 mm lateral to the third mandibular molar and in line with the occlusive plane. Advance the needle 3-4 mm.
Aspirate.
Slowly inject 2 mL of local anesthetic.
Pearls
Note the following:
-
Always remember to obtain informed consent prior to performing a nerve block.
-
Inject slowly (30 seconds for each mL of anesthetic) to decrease pain. [11]
-
In order to aspirate properly, use a needle that is 27 gauge or larger for deep nerve blocks.
-
Buffering with bicarbonate is not recommended for oral nerve blocks. [2]
-
Applying pressure to the site adjacent to injection while inserting the needle may distract the patient and, thereby, decrease the sensation of pain.
-
Massaging tissue for 10-20 seconds is thought to hasten the onset of local anesthetic.
-
Achieving anesthesia with oral nerve blocks may take as long as 10 minutes.
-
True allergies to local anesthetics are rare. With a good patient history, the clinician may be able to discriminate whether the patient is truly allergic or, rather, has experienced adverse effects due to something other than the local anesthetic, such as the epinephrine, a toxic dose of the anesthetic, or a vagal reaction. If the patient has an allergy to one anesthetic, an anesthetic from the other class can be used (amide vs ester), or an alternative agent such as benzyl alcohol or diphenhydramine can be used. [1]
-
If the first attempt at the nerve block fails, try the block again. Some of the blocks (ie, inferior alveolar, infraorbital) are best attempted after a skilled clinician has demonstrated them.
Pearls for infraorbital nerve block
Note the following:
-
If the infraorbital nerve cannot be located, similar anesthesia can be achieved by injecting 5 mL of local anesthetic in a fanlike distribution in the upper buccal fold. [2]
-
The intraoral approach described above is the preferred method for infraorbital nerve block. However, for patients in whom the intraoral approach is contraindicated (eg, by distorted anatomy, infection), the infraorbital nerve can be blocked using an extraoral approach. [2, 6] To perform an extraoral infraorbital nerve block, proceed with the following steps:
Identify external landmarks.
Sterilize the overlying skin.
Insert the needle over the infraorbital foramen, penetrating just beneath the subcutaneous tissue but not into the foramen.
Aspirate.
Slowly inject 1-2 mL of local anesthetic while holding pressure over the infraorbital ridge to prevent ballooning of the lower eyelid. Massage the area for 10-20 seconds.
Pearls for inferior alveolar nerve block
Note the following:
-
To facilitate the angle needed in the inferior alveolar block, the needle can be bent 30 degrees. Never bend needle more than 30 degrees, as it may fracture. [2] Due to the high failure rate in traditional methods of inferior alveolar block (approximately 35-45%), a new arched needle technique was studied with a reported 98% success rate. [12]
-
Failure to achieve complete anesthesia of the mandibular teeth (particularly the incisors and canines) may be due to accessory innervation from the mylohyoid nerve. Better anesthesia can be achieved in this scenario by injecting 1-2 mL of local anesthetic below the second premolar at the intersection of the floor of the mouth and the lingular mandible. [13, 14]
-
The closed-mouth inferior alveolar nerve block approach is useful for patients whose jaws cannot be adequately opened because of abscess, swelling, pain, fracture, or surgical wiring. [6] To perform a closed-mouth inferior alveolar nerve block, proceed with the following steps:
Place the nondominant thumb on the inner surface of the cheek and retract the cheek laterally.
Place the syringe parallel to the occlusive plane at the level of the maxillary molars and their gingival junction.
Direct needle just medial to the ramus and advance 3 cm.
Aspirate.
Inject 3 mL of local anesthetic.
Pearl for posterior superior alveolar nerve block
Note the following:
-
To facilitate the angle needed in the posterior superior alveolar block, the needle can be bent 30 degrees. Never bend needle more than 30 degrees, as it may fracture. [2]
Pearl for anterior superior alveolar nerve block
Note the following:
-
If the block fails to anesthetize the central incisor, use the nasopalatine block to obtain anesthesia. Some patients receive innervation to this tooth via the nasopalatine nerve. [15]
Complications
Potential complications include the following:
-
Trismus and deep space infections can result if the needle is inserted through infected tissue. When the overlying tissue is infected, use only superficial or local infiltration for anesthesia.
-
While experiencing the lack of sensation caused by a nerve block, patients can injure themselves without realizing it. Advise patients to avoid hot beverages and refrain from biting the anesthetized area to test sensation (this is particularly important for pediatric patients).
-
Toxicity can result from the local anesthetic or epinephrine, either from an overdose or from an intravascular injection. For more details, please see Emergency Medicine article Toxicity, Local Anesthetics.
-
If the needle is inserted into the nerve or if anesthetic is injected into a foramen/nerve, neurologic damage can occur secondary to either pressure necrosis or chemical injury. Paresthesias or a sudden increase in pain indicates that the needle is within the nerve bundle. If this occurs, withdraw the needle by 1-2 mm, wait for the paresthesias or pain to subside (10-20 s), and then inject.
-
Hematomas can form if a venus plexus or arterial supply is interrupted by the needle. Treatment consists of cold packs during the first 24 hours, then hot packs to help disintegrate the clot. These are usually of no consequence.
-
Attempts to force the needle, inserting the needle to the hub, or redirecting the needle after insertion may result in needle breakage.
Complications of supraperiosteal nerve block
Note the following:
-
Failure to achieve anesthesia is a possible complication. This complication is usually secondary to the anesthetic not penetrating the cortex of the bone either because it was deposited too far from periosteum or because the cortex is too thick. Therefore, this type of block works best for teeth with thin cortical bone (ie, maxillary incisors, canines, premolars). It doesn’t work as well for the maxillary molars or mandibular teeth in adults because of their thicker bone cortex.
-
Breaching the nasal cavity or maxillary sinus can occur if the needle is inserted too deeply during an attempt to block the maxillary incisors or canines.
Complications of posterior superior alveolar nerve block
Note the following:
-
Advancing the needle too far posteriorly during an attempted posterior superior alveolar nerve block blocks the maxillary nerve.
Complications of nasopalatine nerve block
Note the following:
-
Injecting >0.4 mL of anesthetic can cause separation of the mucosa from the hard palate, resulting in ischemia and necrosis of the mucosa. [6]
Complications of greater palatine nerve block
Note the following:
-
Injecting >0.4-0.5 mL of anesthetic can cause separation of the mucosa from the hard palate, resulting in ischemia and necrosis of the mucosa. [6]
-
The lesser palatine nerve, which is just posterior to the greater palatine nerve and innervates the soft palate and uvula, can be inadvertently anesthetized during the greater palatine nerve block. This causes the patient to have the sensation of throat closure or gagging. Provide reassurance to the patient. [6]
Complications of infraorbital nerve block
Note the following:
-
Violation of the orbit can occur if the needle is advanced too far superiorly. To avoid this, make sure to palpate the position of the needle with the nondominant index finger as the needle is advanced.
-
Vasoconstriction of the facial artery or vein can occur, which results in severe blanching of the face. This complication is more likely to occur if the nerve block was performed with the extraoral approach. Treatment consists of warm compresses and phentolamine to reverse the effects of the epinephrine. Epinephrine is best avoided during an extraoral approach to this nerve block. [2]
Complications of inferior alveolar nerve block
Note the following:
-
Anesthesia of the facial nerve can result if this injection is made too far posteriorly into the parotid gland. The patient then experiences transient Bell palsy. Treatment consists of reassurance and eye protection until the anesthetic wears off. To avoid this complication, make sure that the needle has contacted the bone/mandible prior to injection. [2]
-
Jenyon et al reported a case of transient facial nerve palsy after an inferior alveolar nerve block; full facial nerve function, including eyelid closure, was restored within 5 hours. [16]
-
Gillespie and Gunsolly reported a case of intracranial air embolism after inferior alveolar nerve block; the suspected cause was intravascular injection. [17]
Calculating Concentrations and Dilutions
Sample calculation for 1% lidocaine concentration
Use the following example to determine the maximum mL allowable using 1% lidocaine in a 70 kg male patient.
1% = 1000 mg/100 mL = 10 mg/mL of solution.
Maximum dose of lidocaine without epinephrine is 4.5 mg/kg.
4.5 mg/kg x 70 kg = 315 mg of lidocaine for the maximum allowable dose.
315 mg ÷ 10 mg/mL = 31.5 mL of 1% lidocaine solution for the maximum allowable dose.
Sample calculation for 1:100,000 epinephrine dilution
Note the following:
The concentration 1:100,000 means 1 g epinephrine in 100,000 mL solvent (ie, 1000 mg/100,000 mL or 1 mg/100 mL).
Therefore, 1:100,000 = 0.01 mg/mL epinephrine = 10 mcg epinephrine/mL of solution.
Questions & Answers
Overview
What are the indications for an oral nerve block?
What are the contraindications for an oral nerve block?
What is the role of topical anesthetics in the administration of an oral nerve block?
Which anesthetic agents are used in an oral nerve block?
What is the role of epinephrine in an oral nerve block?
What is the efficacy of ropivacaine for oral nerve block?
Which equipment is needed to perform an oral nerve block?
How is the patient positioned for oral nerve block?
How is the supraperiosteal infiltration oral nerve block performed?
How is the anterior superior alveolar (ASA) nerve block performed?
How is the middle superior alveolar (MSA) nerve block performed?
How is the posterior superior alveolar (PSA) nerve block performed?
How is the infraorbital nerve block performed?
How is the nasopalatine nerve block performed?
How is the greater palatine nerve block performed?
How is the inferior alveolar nerve block performed?
How is the mental nerve block performed?
How is the lingual nerve block performed?
How is the buccal nerve block performed?
What are pearls for performing oral nerve blocks?
What are pearls for performing infraorbital nerve block?
What are pearls for performing anterior superior alveolar nerve block?
What are pearls for performing inferior alveolar nerve block?
What are pearls for performing posterior superior alveolar nerve block?
What are the possible complications of oral nerve block?
What are the possible complications of supraperiosteal nerve block?
What are the possible complications of posterior superior alveolar nerve block?
What are the possible complications of nasopalatine nerve block?
What are the possible complications of greater palatine nerve block?
What are the possible complications of infraorbital nerve block?
What are the possible complications of inferior alveolar nerve block?
How is a 1% lidocaine concentration for oral nerve block calculated?
-
Supraperiosteal infiltration.
-
Anterior superior alveolar (ASA) nerve block.
-
Middle superior alveolar nerve (MSA) block.
-
Posterior superior alveolar (PSA) nerve block.
-
Infraorbital nerve block.
-
Nasopalatine nerve block.
-
Greater palatine nerve block.
-
Inferior alveolar nerve block.
-
Mental nerve block.
-
Lingual nerve block.
-
Buccal nerve block.