Laboratory Studies
No laboratory or blood tests are available to confirm pulmonary atresia with ventricular septal defect (PA-VSD). However, the following evaluations may be helpful:
-
Pulse oximetry can assist the diagnosis of cyanosis, especially in patients with dark skin and anemia (>5 mg/dL of reduced hemoglobin is required). It is also a useful indicator of the adequacy of pulmonary blood flow.
-
Patients with an oxygen saturation greater than 85%-90% usually have well-developed collateral systems; they are at risk for pulmonary overcirculation; patients with oxygen saturations less than 75% may have poorly developed pulmonary vascular and collateral systems.
-
An arterial blood gas (ABG) assessment can reveal hypoxemia and hypocarbia without any significant improvement with hyperoxia, favoring a diagnosis of cyanotic congenital heart disease.
-
Reactive polycythemia and coagulation defects may be evident from the results of hematologic studies.
-
Because, in some cases, pulmonary atresia with ventricular septal defect is associated with DiGeorge syndrome and velocardiofacial syndrome, genetic evaluation, including a fluorescent in situ hybridization (FISH) test, may be required.
Imaging Studies
Electrocardiography
Right ventricular (RV) hypertrophy and right-axis deviation are the rule on electrocardiography findings. Right atrial hypertrophy is also is present.
In a small subgroup of patients with increased pulmonary blood flow, combined ventricular hypertrophy with left atrial enlargement may be present.
Chest radiography
Chest radiographic features may include the following:
-
A boot-shaped heart (coeur en sabot) may be observed. It occurs secondary to an upturned cardiac apex caused by RV hypertrophy and concavity in the region of the main pulmonary artery, which is produced by underdevelopment of the subpulmonary infundibulum.
-
The heart size is usually normal or slightly enlarged, most often with an RV configuration.
-
The main pulmonary arterial shadow normally depicted on chest radiography is absent.
-
The pulmonary vascular markings have a heterogeneous reticular pattern in the presence of collateral arteries from the systemic arteries.
-
Approximately 50% of patients have a right aortic arch with a large aorta.
-
The lung field is oligemic in patients with very small collateral arteries.
-
Lung fields may be flooded if the patient has a large patent ductus arteriosus (PDA) with normally developed central pulmonary arteries or well-developed systemic collateral arteries.
Echocardiography
Findings on echocardiograms may include the following:
-
Parasternal long-axis scans reveal a large aortic valve overriding a malaligned ventricular septal defect.
-
Position of malalignment of the ventricular septal defect (membranous or infundibular) and a blind hypoplastic RV infundibulum is easily observed using parasternal cross-sectional echocardiography.
-
Atrial septal defects (ASDs) and other muscular ventricular septal defects can be detected.
-
Scans from the suprasternal notch and high parasternal windows usually can provide important information regarding the size of the proximal pulmonary arteries and the presence of confluence. These views can also help define the side of the aortic arch and assess the patency of the ductus arteriosus.
-
A right-sided aortic arch is frequently defined using the suprasternal notch view.
-
Echocardiography is sensitive for detection of aortopulmonary collaterals, but it is inadequate for complete delineation.
-
Defining all the collateral arteries with echocardiography is difficult.
-
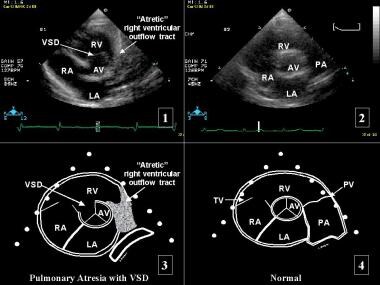
Short-axis parasternal (see the image below) and subcostal views are used to detect coronary artery abnormalities.
-
 Pulmonary Atresia With Ventricular Septal Defect. Short-axis parasternal view (1) and diagram (3) in a patient with pulmonary atresia and ventricular septal defect (PA-VSD). Short-axis parasternal view (2) and diagram (4) in a patient with normal anatomy. LA = left atrium; PA = pulmonary artery; PV = pulmonary valve; RA = right atrium; RV = right ventricle; and TR = tricuspid valve.
Pulmonary Atresia With Ventricular Septal Defect. Short-axis parasternal view (1) and diagram (3) in a patient with pulmonary atresia and ventricular septal defect (PA-VSD). Short-axis parasternal view (2) and diagram (4) in a patient with normal anatomy. LA = left atrium; PA = pulmonary artery; PV = pulmonary valve; RA = right atrium; RV = right ventricle; and TR = tricuspid valve.
Magnetic resonance imaging (MRI)
MRI is a less invasive technique used to help define the surgically relevant pulmonary artery anatomy, but MRIs are inadequate for defining peripheral pulmonary arterial distribution. [9]
Procedures
Cardiac catheterization and angiography are essential in evaluating the size and distribution of the native pulmonary arteries and the collateral arteries. Findings may include the following:
-
Right atrial pressure is normal unless tricuspid incompetence is present.
-
Pressures in the right ventricles (RVs) are at a systemic level because of the nonrestricted ventricular septal defect.
-
Evaluation of the native pulmonary arterial system may be difficult unless there is a ductal-dependent pulmonary circulation or a connection between a collateral vessel and the native pulmonary arterial system.
-
The presence of elevated distal pressures within the collateral arteries (mean pressures greater than 20-25 mm Hg) suggests significant pulmonary vascular obstructive disease (PVOD) within the affected lung segments.
-
Evaluation of the RV systolic pressure (RVSP) is important in assessing ventricular septal defect (VSD) closure in patients who have been managed with unifocalization and an RV-PA (right ventricle to pulmonary artery) conduit without VSD closure; an RVSP less than 70% systemic suggests that the VSD can be closed.
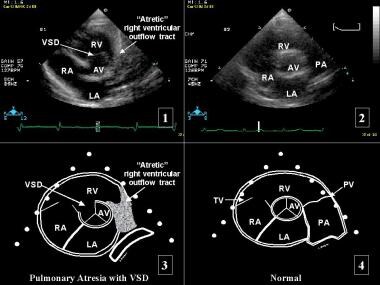
See the following angiograms.
 Pulmonary Atresia With Ventricular Septal Defect. Left anterior oblique ventriculogram in a patient (same patient as in the next image) with pulmonary atresia with ventricular septal defect (PA-VSD). The angiogram shows the left and right ventricles with a large malalignment VSD between them. The only outflow from the heart is the aorta. No evidence of pulmonary blood flow is observed arising from the ventricles directly to the lungs. Asc Ao = ascending aorta; Desc Ao = descending aorta; LV = left ventricle; and RV = right ventricle.
Pulmonary Atresia With Ventricular Septal Defect. Left anterior oblique ventriculogram in a patient (same patient as in the next image) with pulmonary atresia with ventricular septal defect (PA-VSD). The angiogram shows the left and right ventricles with a large malalignment VSD between them. The only outflow from the heart is the aorta. No evidence of pulmonary blood flow is observed arising from the ventricles directly to the lungs. Asc Ao = ascending aorta; Desc Ao = descending aorta; LV = left ventricle; and RV = right ventricle.
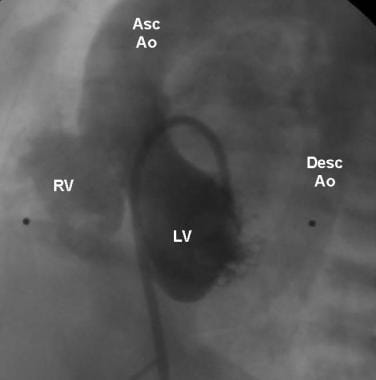
 Pulmonary Atresia With Ventricular Septal Defect. Anteroposterior view of an aortogram in a patient (same patient as in the previous image) with pulmonary atresia with ventricular septal defect (PA-VSD). The pulmonary circulation is supplied by collateral vessels (Collaterals) that arise from the descending aorta (Desc Ao).
Pulmonary Atresia With Ventricular Septal Defect. Anteroposterior view of an aortogram in a patient (same patient as in the previous image) with pulmonary atresia with ventricular septal defect (PA-VSD). The pulmonary circulation is supplied by collateral vessels (Collaterals) that arise from the descending aorta (Desc Ao).
-
Pulmonary Atresia With Ventricular Septal Defect. Management algorithm for patients with pulmonary atresia with ventricular septal defect (PA-VSD) and major aortopulmonary collateral arteries (MAPCAs), based on the nature of pulmonary vascular supply. PAs = pulmomary arteries. Courtesy of Elsevier (Gupta A, Odim J, Levi D, Chang RK, Laks H. Staged repair of pulmonary atresia with ventricular septal defect and major aortopulmonary collateral arteries: Experience with 104 patients. J Thorac Cardiovasc Surg. 2003;126(6):1746–52).
-
Pulmonary Atresia With Ventricular Septal Defect. Anteroposterior still image obtained from angiography in the aortic arch of a 3-week-old infant born with pulmonary atresia with ventricular septal defect (PA-VSD) who is receiving a prostaglandin E infusion. A patent ductus arteriosus (PDA) is seen supplying confluent branch pulmonary arteries. Courtesy of Dr Thomas Forbes.
-
Pulmonary Atresia With Ventricular Septal Defect. Anteroposterior angiographic view in the aortic arch of a 3-week-old infant born with pulmonary atresia with ventricular septal defect (PA-VSD) who is receiving a prostaglandin E infusion. A patent ductus arteriosus (PDA) is seen supplying confluent branch pulmonary arteries. Courtesy of Dr Thomas Forbes.
-
Pulmonary Atresia With Ventricular Septal Defect. Anteroposterior still image obtained from angiography in a 3.5-mm right modified Blalock–Taussig (BT) shunt in the previous patient at age 4 months. There is a patent BT shunt with mild proximal right upper lobe and right lower lobe branch stenoses. Courtesy of Dr Thomas Forbes.
-
Pulmonary Atresia With Ventricular Septal Defect. Anteroposterior angiographic view in a 3.5-mm right modified Blalock–Taussig (BT) shunt in the previous patient at age 4 months. There is a patent BT shunt with mild proximal right upper lobe and right lower lobe branch stenoses. Courtesy of Dr Thomas Forbes.
-
Pulmonary Atresia With Ventricular Septal Defect. Lateral still image obtained from angiography in the previous patient at age 21 months. The infant underwent Rastelli operation with placement of a 15-mm pulmonary homograft. In this image, there is free homograft insufficiency without stenosis. Courtesy of Dr Thomas Forbes.
-
Pulmonary Atresia With Ventricular Septal Defect. Lateral angiographic view in the previous patient at age 21 months. The infant underwent Rastelli operation with placement of a 15-mm pulmonary homograft. The presence of free homograft insufficiency with no stenosis is observed. Courtesy of Dr Thomas Forbes.
-
Pulmonary Atresia With Ventricular Septal Defect. Lateral still image obtained from angiography in a 7-year-old boy born with pulmonary atresia with ventricular septal defect (PA-VSD) who underwent Rastelli operation with a 17-mm right ventricle to pulmonary artery (RV-PA) homograft. There is mild proximal conduit stenosis and free conduit insufficiency. The right ventricle appears moderately dilated. Courtesy of Dr Thomas Forbes.
-
Pulmonary Atresia With Ventricular Septal Defect. Lateral angiographic view in a 7-year-old boy born with pulmonary atresia with ventricular septal defect (PA-VSD) who underwent Rastelli operation with a 17-mm right ventricle to pulmonary artery (RV-PA) homograft. There is mild proximal conduit stenosis and free conduit insufficiency. The right ventricle appears moderately dilated. Courtesy of Dr Thomas Forbes.
-
Pulmonary Atresia With Ventricular Septal Defect. Lateral still image from angiography in the previous patient at age 8 years following Melody valve placement in the prestented 17-mm right ventricle to pulmonary artery (RV-PA) homograft. The Melody valve appears in good position. There is no Melody valve insufficiency. Courtesy of Dr Thomas Forbes.
-
Pulmonary Atresia With Ventricular Septal Defect. Lateral angiographic view in the previous patient at age 8 years following Melody valve placement in the prestented 17-mm right ventricle to pulmonary artery (RV-PA) homograft. The Melody valve appears in good position. There is no Melody valve insufficiency. Courtesy of Dr Thomas Forbes.
-
Pulmonary Atresia With Ventricular Septal Defect. Left anterior oblique ventriculogram in a patient (same patient as in the next image) with pulmonary atresia with ventricular septal defect (PA-VSD). The angiogram shows the left and right ventricles with a large malalignment VSD between them. The only outflow from the heart is the aorta. No evidence of pulmonary blood flow is observed arising from the ventricles directly to the lungs. Asc Ao = ascending aorta; Desc Ao = descending aorta; LV = left ventricle; and RV = right ventricle.
-
Pulmonary Atresia With Ventricular Septal Defect. Anteroposterior view of an aortogram in a patient (same patient as in the previous image) with pulmonary atresia with ventricular septal defect (PA-VSD). The pulmonary circulation is supplied by collateral vessels (Collaterals) that arise from the descending aorta (Desc Ao).
-
Pulmonary Atresia With Ventricular Septal Defect. Short-axis parasternal view (1) and diagram (3) in a patient with pulmonary atresia and ventricular septal defect (PA-VSD). Short-axis parasternal view (2) and diagram (4) in a patient with normal anatomy. LA = left atrium; PA = pulmonary artery; PV = pulmonary valve; RA = right atrium; RV = right ventricle; and TR = tricuspid valve.