Approach Considerations
Indications
The indications for central lines in children parallel those in adults.
Central venous access devices (CVADs) are used to deliver larger volumes of irritating solutions, such as antibiotics, blood products, parenteral nutrition media, and sclerosing chemotherapeutic agents. If patients need prolonged intravenous (IV) access, a CVAD is preferred to a peripheral IV line. Central access is also indicated when peripheral access cannot be achieved; however, in an emergency situation (eg, trauma), when peripheral and central access cannot be expeditiously obtained, the intraosseous route is the next best choice for obtaining vascular access.
Peripherally inserted central catheters
Peripherally inserted central catheters (PICCs) have been used with great success in neonatal intensive care units (NICUs) and are considered a mainstay of vascular access in this setting. Although the lines are inserted peripherally, usually via the cephalic vein in the upper extremity or the saphenous vein in the lower extremity, the distal tip is placed in a large central vein.
In NICUs specifically, PICC placement has largely supplanted the routine placement of higher-risk central venous catheters (CVCs), both percutaneous and cutdown. PICC lines are indicated in children who require intermediate-term IV access for prolonged home or hospital therapy, such as patients with chronic infections, cancer, and parenteral nutrition dependency.
The success of placing a PICC line is improved if attempts to insert peripheral IV lines are avoided. Therefore, PICC placement should be attempted as soon as the need for intermediate-term access is apparent.
Central venous catheters
CVCs are inserted at femoral, subclavian, and internal jugular sites. These devices are preferred in children who have no peripheral access and in those who require long-term IV access. The subclavian route has been the preferred route for many years and affords the patient the greatest mobility. The internal jugular vein (IJV), either via cutdown or via percutaneous access, is also a popular site in children that is amenable to placement under ultrasonographic (US) guidance. [16]
The femoral vein is not often used as the primary site for central venous access. The rare occasions for using the femoral site include the following [17] :
-
Placement of a temporary hemodialysis or pheresis catheter
-
Inaccessibility of other primary central veins as a consequence of thrombosis or stenosis
-
During cardiopulmonary resuscitation (CPR), in that this approach does not interfere with chest compressions or defibrillation
Implantable access ports
Implantable access ports (IAPs), such as Mediport and Port-A-Cath, have become the most popular vascular access device in children for the following reasons [18, 19] :
-
Lower risk of infection
-
Little to no hindrance of daily activities
-
Minimal alterations in body image
-
No routine dressing changes
IAP devices are surgically implanted in the operating room (OR), usually under fluoroscopic guidance (though US guidance has also been described [20] ).
The most common indications for port placement in children include the following:
-
Patients with cancer
-
Patients who need long-term antibiotics
-
Patients in whom long-term IV access is needed (eg, those with cystic fibrosis and sickle cell disease)
Concerns have been expressed about whether these devices are safe in very young children (infants < 1 y); however, a study by Ross et al found IAP placement to be safe for most infants, with low or acceptable rates of intra- or postoperative complications. [21]
Umbilical artery catheters and umbilical vein catheters
Accessing the umbilical vascular system is useful in the first few days of life. The umbilical vein can be used for access during the first 5-7 days but is rarely used beyond 7 days.
Both umbilical artery catheters (UACs) and umbilical vein catheters (UVCs) can be used. The UAC courses from the umbilical artery to the internal iliac artery and is used for hemodynamic monitoring. The UVC courses through the ductus venosus and the inferior vena cava (IVC) and can be used for delivering fluids, pressors, and IV medications, as well as for central venous pressure monitoring.
The umbilical vascular access site is commonly used in the early neonatal period and is subsequently discontinued after longer-term vascular access is established.
Contraindications
Contraindications for inserting a CVC include the following:
-
Infection or burn over the desired insertion site
-
Known venous thrombosis of the vessel
-
Uncorrected coagulopathy
-
Obstruction of the vein by a tumor or mass
-
Abnormal vessels
-
Ability to achieve the same objectives with a peripheral line
-
Lack of consent in a nonemergency setting
Among patients who are receiving chemotherapy, those who are neutropenic with a low absolute neutrophil count (ANC) are also advised to wait prior to central line placement.
A relative contraindication is bacterial bloodstream infection (BSI); it is generally recommended that cultures be sterile for 36-48 hours before a CVC is inserted.
Preparation for Procedure
The preparation for inserting a CVC is similar for all of the techniques described below, with some distinct and important differences.
All patients should be properly secured, sedated, or both to ensure minimal movement. With the exception of placing a central line in the NICU or the pediatric intensive care unit (PICU), virtually all children undergo general anesthesia for line placement, which differs from the use of local anesthesia and sedation in adults. It is critical that patients, especially small children, remain completely still during the accessing of the vein; movement of just a few millimeters of the needle can be the difference between success and failure.
The skin is cleansed with an antiseptic solution (eg, chlorhexidine-alcohol), and the entire area should be draped with sterile towels. A local anesthetic, such as 1% lidocaine (maximum dose, 5 mg/kg), can be used. Specific positioning for particular approaches is described below (see Approaches for Gaining Central Venous Access). A properly sized catheter should be chosen on the basis of the location of the catheter and the patient's age and weight (see Table 1 below).
Table 1. Central Venous Access Device Sizes Based on Age and Weight (Open Table in a new window)
Age (y) |
Weight (kg) |
Gauge |
French |
Length (cm) |
< 1, newborn |
4-8 |
24 |
3.0 |
5-12 |
< 1 |
5-10 |
22 |
3.0-3.5 |
5-12 |
1-3 |
10-15 |
20 |
4.0 |
5-15 |
3-8 |
15-30 |
18-20 |
4.0-5.0 |
5-25 |
>8 |
30-70 |
16-20 |
5.0-8.0 |
5-30 |
Approaches for Gaining Central Venous Access
Internal jugular approach
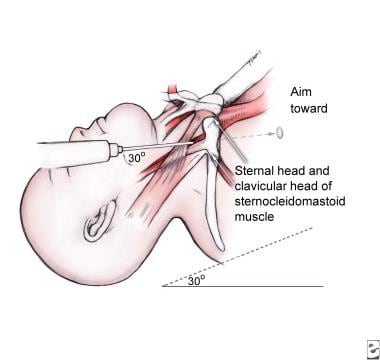
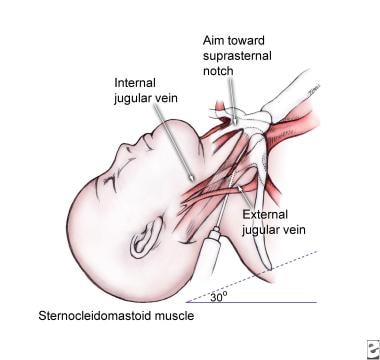
The patient's head is rotated to the side opposite the insertion area. The three common internal jugular approaches are the central, anterior, and posterior methods. (See the images below.)
The central approach is performed by finding the superior apex of the triangle formed by the two heads of the sternocleidomastoid (SCM) and the clavicle. The needle advances at this apex and continues toward the ipsilateral nipple. A shallow angle is needed because of the small diameter of veins in children.
The anterior approach is performed by introducing the needle at the medial edge of the SCM at the level of the thyroid cartilage and aimed toward the ipsilateral nipple.
The posterior approach uses the lateral edge of the SCM approximately two thirds of the way from the mastoid process to the clavicle to insert the needle, which is aimed toward the sternal notch.
Once the catheter needle has pierced the skin, it is introduced and advanced with continuous negative pressure until enough blood is obtained, at which point it is secured in place. If a needle-over-wire or Seldinger technique is used, it should be advanced so that the catheter reaches the junction of the superior vena cava (SVC) and the right atrium.
The Seldinger technique is as follows. After blood has been withdrawn, the syringe is removed, and a wire is inserted into the needle. This should be advanced with minimal resistance to the proximal vein. If the procedure is being performed in the OR, fluoroscopy is generally used to guide the procedure and ensure proper wire placement into the right side of the heart.
Then, the needle (with the wire in place) is removed. A small (2-mm) incision is made over the wire with a No. 11 blade to allow passage of a dilator over the wire. The dilator is removed, and the preflushed catheter is advanced over the wire and secured. The wire is then removed. All ports should be drawn back to show blood, then flushed. A sterile dressing, preferably a transparent one, should be placed.
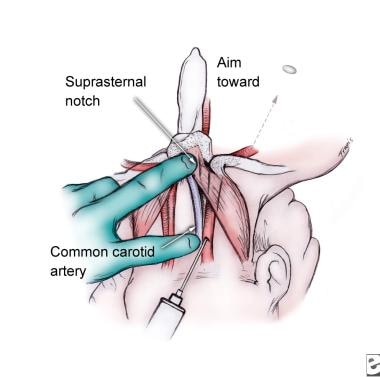
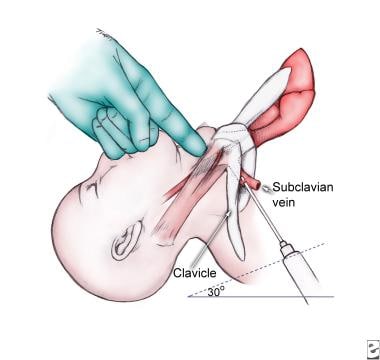
Subclavian approach
In a child, the subclavian vein approach differs from what it would be in an adult. (See the image below.)
The patient should be in a steep Trendelenburg position to maintain venous dilation and to prevent an air embolus. A towel roll should be placed between the patient's shoulders, if necessary, to open the anterior aspect of the chest wall. The only disadvantage of this measure is that a shoulder roll may also narrow the space between the clavicle and first rib, thus making passage of the wire more difficult after needle access to the vein is obtained.
The needle should be inserted at the lateral third of the clavicle and 1-2 cm below it (or, in rare cases, more than twice the width of the clavicle). The authors' experience has been that a straight needle directed medially and inferiorly easily passes through the intercostal space into the pleural domes. By manually bending the needle into a gentle curve (ie, without acute angles) and by directing the needle with the tip constantly oriented in the cephalic direction toward the sternal notch, one can keep the tip above the first rib, avoid pneumothoraces, and enter the vein from above.
Stabilization of the needle once the vein has been accessed is a paramount consideration, particularly in smaller patients. A Kelly clamp or a large needle driver can be used to secure the needle's position fully while disconnecting the syringe. This, with the subsequent passage of the Seldinger wire, prevents the tip of the needle from twisting out of the vein. The needle should be directed just superior to the sternal notch under the clavicle. Care should be taken to remove the needle before it is redirected to avoid laceration of the vessels.
Once blood is obtained and the needle is secure, the Seldinger technique is used, as is described in the internal jugular approach.
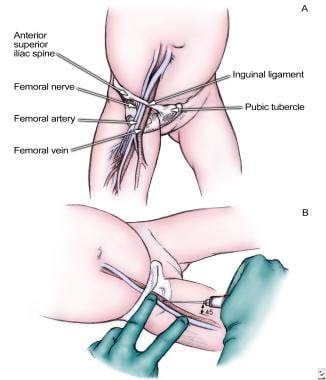
Femoral approach
The femoral approach is performed after the child is placed in a supine position. A frog-leg position may be helpful in smaller children. (See the image below.)
Palpation of the femoral artery (lateral to the vein) is a key feature in this procedure. The femoral artery is palpated with one finger, and the needle is introduced just medial to the finger at an angle of 30-45° at 1 cm below the inguinal ligament. The needle should be directed toward the umbilicus. Once blood is returned, the catheter can be advanced and secured or the Seldinger technique can be used for a longer CVC, as described in the internal jugular approach.
Peripheral approach
The PICC line is inserted at any peripheral site that has direct access to the central circulation. Once a site has been determined and the patient prepared, an 18-gauge needle is used to puncture the skin site to ease insertion of the introducer. The length of these catheters can exceed 30 cm; therefore, one must measure the distance from the insertion site to the right nipple. This measure maintains the catheter tip at the SVC–right atrium junction.
Once the introducer is advanced and blood return is achieved, the catheter is grasped 1 cm proximal to its distal tip and introduced 1 cm at a time until it reaches the preset location. The introducer needle is then withdrawn and peeled away from the catheter. It should be secured and rechecked for its ability to be easily flushed.
Umbilical approach
After the umbilical stump is properly prepared, a purse-string suture is placed at the junction of the skin and the cord to ensure hemostasis and anchoring of the line. (See the image below.)
The cord is cut 1 cm from the skin with the vein and arteries coming into view. The preflushed catheter is advanced into the vein 1-2 cm beyond the point where blood is easily returned; this is a total of 4-5 cm in a full-term infant. If the catheter is pushed further than this, it may enter the ductus venosus and then the IVC. The catheter is then secured in place with tape.
The use of electrocardiography (ECG) to guide umbilical vein catheterization in neonates has been described. [22]
Implantable device
If lines are to be in place for a prolonged period, an implantable venous device (eg, Mediport) can be used. The port catheter is inserted mainly via the subclavian vein and tunneled under the skin to an adjacent site, where the reservoir is inserted in a subcutaneous pocket and anchored to the pectoralis fascia with suture. Such ports contain a silicone diaphragm that may be accessed as many as 2000 times by using a special side-hole needle (Huber needle).
Postprocedural Care
After placement of the central line, meticulous care should be directed toward the line dressing. For externalized lines or accessed ports, a chlorhexidine patch can be used to lower infection rates. An occlusive and transparent dressing is also recommended for infection prevention, as well as for visualizing the exit site and ensuring that there is no ongoing blood loss. Securement devices may be considered for preventing dislodgment. [23, 24] Using extra measures, such as extra tape and arm boards, is vital to prevent the patient from removing the device.
Once the lines are secured, the patient's vital signs should be assessed, and a focused physical examination should be performed to look for complications or iatrogenic injuries. Postoperative radiography should also be performed to rule out pneumothorax and confirm the baseline position of the catheter.
Complications
A full discussion of complications is outside the scope of this article; however, the main problems and useful current therapies for these problems are discussed below.
All of the complications described here can be reduced by preparing well, using proper sedation and restraints, applying adequate local anesthesia, following strict aseptic techniques in placing and caring for the line, understanding the associated anatomy, and using ancillary imaging studies (eg, US and fluoroscopy) when available. [25, 2]
Bloodstream infections
BSIs are a risk with any CVC [26, 27, 28] and have been estimated to occur in 7.7 per 1000 patients in the PICU. In the NICU, the BSI rate is 11.3 cases per 1000 babies with birth weights of less than 1000 g and 4 cases per 1000 babies with birth weights of more than 2500 g.
BSIs increase mortality, which is estimated to be in the range of 12-25%. The average cost per episode of BSI is $25,000.
The etiology of most BSIs in children is coagulase-negative staphylococci, which account for approximately 37% of all cases in PICUs. Exposure to lipids has been identified as an independent risk factor for both coagulase-negative staphylococcal bacteremia in very-low-birth-weight infants and candidemia in the NICU. Gram-negative bacteria account for 25% of all BSIs reported in PICUs, whereas enterococci and Candida species account for 10% and 9%, respectively.
In one study, a flush solution containing an antibiotic (vancomycin and ciprofloxacin) and heparin substantially decreased complications, both infectious and thrombotic, compared with heparin alone. [29] The prevalence of resistant organisms did not increase.
Catheters impregnated with chlorhexidine and silver sulfadiazine have been shown to reduce catheter-related infections. Rates decreased from 7.6 cases per 1000 catheter days to 1.6 cases per 1000 catheter days. A systematic review and meta-analysis by Kramer et al found evidence suggesting that antimicrobial PICCs may reduce BSI associated with central lines, especially in high-risk subgroups, but noted that randomized trials would be needed to determine their efficacy across different patient populations. [30]
Venous thrombosis
Thrombotic complications are particularly prevalent in the pediatric population because of the small luminal diameter of the vessels used. More than 3.5 patients per 10,000 hospital admissions develop catheter-related deep vein thrombosis (DVT); cancer is the underlying diagnosis in 50% of these patients. [31] As many as 16% of these patients develop pulmonary embolism (PE); the upper extremities are the predominant areas.
Shin et al reported a 26.3% incidence of venous thrombosis or stenosis in 376 children who underwent PICC placement. [32] They found that patients previously exposed to non-PICC CVCs were nearly twice as likely to develop this complication.
A meta-analysis by Ullman et al reported a 4% incidence of symptomatic venous thromboembolism (VTE) in pediatric patients with CVADs, as well as a 10% incidence of asymptomatic VTE. [33]
Direct thrombolysis with urokinase, using the lumen of a PICC line to facilitate the insertion of an infusion catheter, has been shown to be an easy and effective means to remedy the thrombosis. [34]
A study by McLaughlin et al found that in pediatric trauma patients, the use of the femoral route for catheterization was more likely to give rise to symptomatic catheter-associated thrombosis than the use of subclavian, arm-vein, or internal jugular routes. [35]
Catheter-related occlusions
Catheter-related occlusions can occur in as many as 25% of lines placed in children. The result is an inability to use the catheter to administer vital medications and perform blood draws.
Restoring patency is preferred to replacement because it is faster and less expensive. In Europe, fibrinolytic therapy has been used for decades to restore patency in CVC occlusions. Recombinant tissue-type plasminogen activator (rt-PA) is an alternative to fibrinolytic therapy. In one study of 320 occlusion events, patency was restored in 71% of CVC occlusions after the first infusion, in 86.8% after the second infusion, and in 90.6% after the third infusion. [36]
Doses of 0.02-0.03 mg/kg have been used. Essentially, 1 mL of solution is inserted into the line and left for 4 hours. The fibrinolytic agent is then drawn out of the line, and a flush is attempted with saline. This may be repeated if unsuccessful.
Other complications
Other well-described complications include the following:
-
Pneumothorax
-
Arterial canalization
-
Nerve injury
-
Infection
-
Bleeding
-
Hematoma formation
-
Loss of the wire or catheter intravascularly
-
Air embolization
-
Pain
Central lines can also migrate either into a noncentral vein or even out of the vein altogether.
Long-Term Monitoring
The IV lines should be flushed with a heparinized solution after each blood draw to prevent clotting of the catheter. The lines should be checked on a daily basis to detect early infection and line sepsis. The patient's vital signs should be monitored for this purpose as well.
-
Femoral vein approach. Remember mnemonic NAVEL: nerve, artery, vein, empty space, and lymphatics.
-
Umbilical vein cannulation in newborn.
-
Internal jugular vein, anterior approach.
-
Subclavian vein approach.
-
Internal jugular vein, central approach.
-
Internal jugular vein, posterior approach.