Definition Top
Blastocystosis is a disease of the large intestine caused by the protozoal parasite Blastocystis hominis.
EpidemiologyTop
B hominis is a cosmopolitan parasite, but invasions are most common in low-income countries with low sanitary standards. The parasite is often identified in individuals with HIV infection, patients in psychiatric wards, and children attending preschool facilities.
Etiology and PathogenesisTop
1. Etiologic agent: Protozoal parasite B hominis. The parasite has undetermined taxonomy and not fully known life cycle. Individual development stages of B hominis are highly diversified, with various morphologic forms including vacuolar, granular, multivacuolar, avacuolar, ameboid, and cyst forms. The predominant form found in stool specimens is the round or oval-shaped vacuolar form (Figure 1) sized 6 to 40 microm in diameter, with a large central vacuole surrounded by cell nuclei and other peripherally located organelles. The thick-wall cyst is postulated to be the invasive form for humans.
The pathogenesis of blastocystosis remains unclear. Cases with intestinal mucosal edema and inflammation and cases with colonic ulcerations have been reported.
2. Reservoir and transmission: The primary reservoir of B hominis is humans. Transmission occurs through the fecal-oral route, typically through ingestion of water or foods contaminated with human feces.
Clinical FeaturesTop
The infection is frequently asymptomatic (carriers).
Types of symptomatic disease:
1) Mild blastocystosis: The most common type; manifests with diarrhea (without blood in stool), abdominal pain, nausea, weight loss, and sometimes fine macular rash.
2) Acute blastocystosis: Very rare; typically manifests with watery diarrhea, spastic abdominal pain, and occasionally fever; may lead to gastrointestinal (GI) bleeding.
Irritable bowel syndrome (IBS) has been associated with blastocystosis in some studies, although a causal relationship has not been proven.Evidence 1Low Quality of Evidence (low confidence that we know true effects of the intervention). Quality of Evidence lowered due to imprecision the risk of bias and indirectness. Nourrisson C, Scanzi J, Pereira B, et al. Blastocystis is associated with decrease of fecal microbiota protective bacteria: comparative analysis between patients with irritable bowel syndrome and control subjects. PLoS One. 2014 Nov 3;9(11):e111868. doi: 10.1371/journal.pone.0111868. PMID: 25365580; PMCID: PMC4218853.
DiagnosisTop
Diagnosis is made based on microscopic identification of any morphologic forms of B coli in stool. Repeat stool sampling is usually recommended, several days apart, as the parasite is excreted in shifted temporal patterns and in varying amounts.
Because of the morphologic diversity of the different forms of B hominis, standard direct stool examination should be accompanied by the analysis of permanent trichrome-stained smears.
Polymerase chain reaction (PCR) assays are now available and have high sensitivity and specificity. However, as B hominis is frequently found in asymptomatic individuals and its pathogenicity is not fully known, the significance of a positive PCR test result is debatable.
1. Other GI parasitic diseases.
2. Infectious diarrhea.
3. Functional bowel disorders, including IBS.
TreatmentTop
1. Symptomatic treatment: As in infectious diarrhea.
2. Antiprotozoal treatment: B hominis is a saprophytic protozoan and the infection usually does not require specific treatment. Specific treatment is indicated in patients with comorbid conditions such as ulcerative colitis or Crohn disease, in immunosuppressed individuals, and in massive infections.
1) First-line treatment: Metronidazole 500 to 750 mg tid for 10 days or 1.5 g once daily for 7 days; or cotrimoxazole 320/1600 mg once daily or bid in divided doses for 7 days. Some specialists recommend higher doses of cotrimoxazole, 320/1600 mg bid.
2) Alternative treatment: Iodoquinol 650 mg tid for 10 to 20 days, nitazoxanide 500 mg bid for 3 days, paromomycin 500 mg tid for 7 days or 25 mg/kg tid for 10 days, tinidazole 2 g once daily for 5 days.
COMPLICATIONSTop
Invasive colonic disease and GI bleeding may occur in the very rare cases of acute infection. B hominis may cause exacerbations of ulcerative colitis.
PROGNOSISTop
In general the prognosis is good.
PreventionTop
1. Avoiding consumption of contaminated water or food (particularly in tropical areas).
2. Maintaining good personal hygiene.
FiguresTop
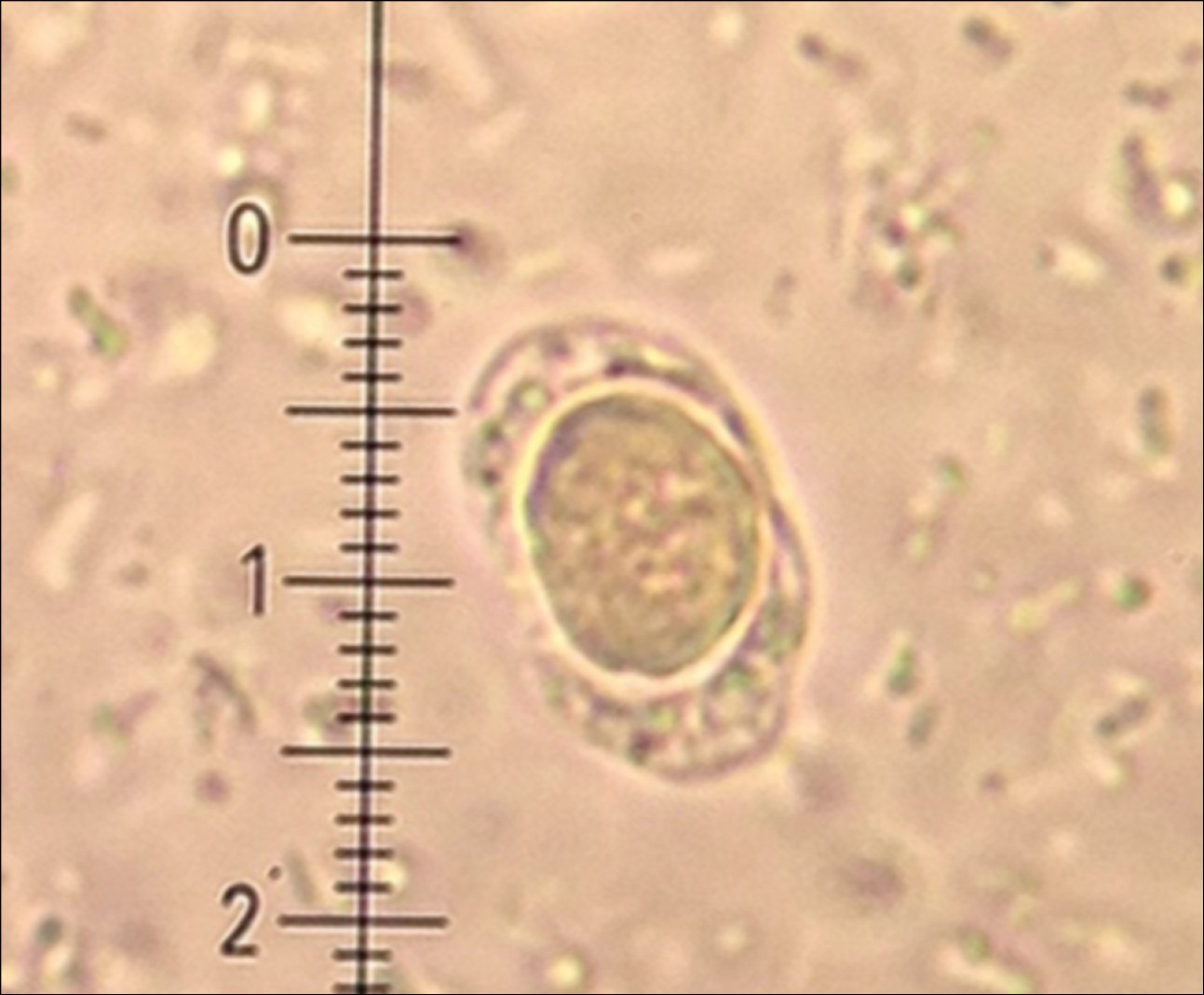
Figure 10.9-1.
Vacuolar form of Blastocystis hominis.