This case is written by Dr. Lindsey McMurray. She is a PGY4 Emergency Medicine resident from the University of Toronto who is currently doing a Resuscitation and Reanimation fellowship at Queen’s University.
Why it Matters
When the cause of acute respiratory distress is clear, its management can feel routine. However, as many senior physicians can attest, sometimes the cause is quite uncertain. It is important for junior learners to work through this differential because:
- Acute respiratory distress is a relatively common patient presentation
- Simultaneous initiation of investigations and treatment requires significant resource management skills
- Delays to treatment in the critically ill patient can lead to poor outcomes
Clinical Vignette
You are on the Gynecology service and have been paged by the ward nurse to attend to a 78 year old woman who is having trouble breathing. She is POD #0 from a 4 hour TAH+BSO operation for ovarian CA. She just got to the ward about 1 hour ago. You enter the patient’s room she is hooked up to an IV with NS running at 150cc/hr.
Case Summary
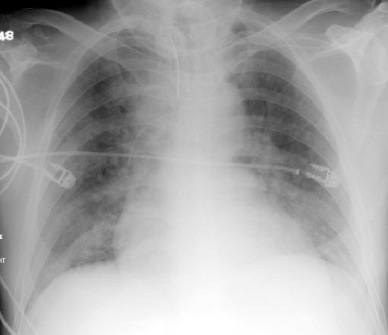
A 78 year old woman post-op from a TAH+ BSO for ovarian CA has just been transferred to the ward when she develops acute shortness of breath. When the resident arrives, the patient is in significant respiratory distress saturating 80% on RA. Oxygen and medical therapy will not adequately relieve the patient’s distress. The resident will need to recognize that the patient has a Grade 3-4 LV and received 2L of fluid intra-operatively. When BiPAP is called for, it will be unavailable. Ultimately, the patient will require intubation.
Download the case here: Acute Respiratory Distress
ECG for case found here:
(ECG source: https://thejarvik7.files.wordpress.com/2012/02/inferior-wall-stemi-2005-05-27-08.jpg)
CXR for case found here:
(CXR source: https://www.med-ed.virginia.edu/courses/rad/cxr/pathology2chest.html)