Advertisement
Advertisement
July 2020
CEAP 2020: Understanding and Applying the Updated Chronic Venous Disease Classifications
Dr. Teresa Carman interviews Dr. Fedor Lurie to explore the processes by which the 2020 CEAP classification revisions were arrived upon and gain insights into their application.

Dr. Carman: Congratulations on the completion of a very extensive, nearly 3-year process revising the CEAP classification system. With CEAP last updated in 2004 and well ingrained into venous disease practice, why did the American Venous Forum (AVF) feel it needed an update after 15 years?
Dr. Lurie: Thank you for providing me the opportunity to talk about the revised classification. The CEAP classification is based on our current understanding of venous pathology and manifestations of the chronic venous disorders, which of course changes over time. Therefore, CEAP classification requires periodic revisions. The first revisions were done in 2004 after CEAP had existed for 7 years, and it took longer for the second update. The AVF felt that it was necessary to analyze whether the classification needed revision. There were a number of suggestions over time that pointed to deficiencies and shortcomings of the existing CEAP classification. A task force first had to examine whether those revisions were needed, and if so, suggest which ones were reasonable for updating.
Dr. Carman: Can you briefly explain how the revision process began and the four key considerations used for the revision?
Dr. Lurie: That’s a very important question. Every time you revise a classification, although necessary, new issues are created. With this in mind, we decided that this revision should be done very carefully to not impact the previous uses of CEAP classification. One major consideration was that a revised or updated classification would be backward compatible. Any publications or reports that were using CEAP before can continue to be analyzed without interruption; whether we have achieved this is yet to be seen. We also decided that those changes should be evidence-based. If a revision seems to be reasonable but does not have data to support it, those revisions would probably be not accepted. The other important part was that there are practitioners who feel the CEAP classification is not very practical. What we considered very seriously for each suggested change was how practical the change was, whether it would increase the use of CEAP classification, or make it more difficult to implement.
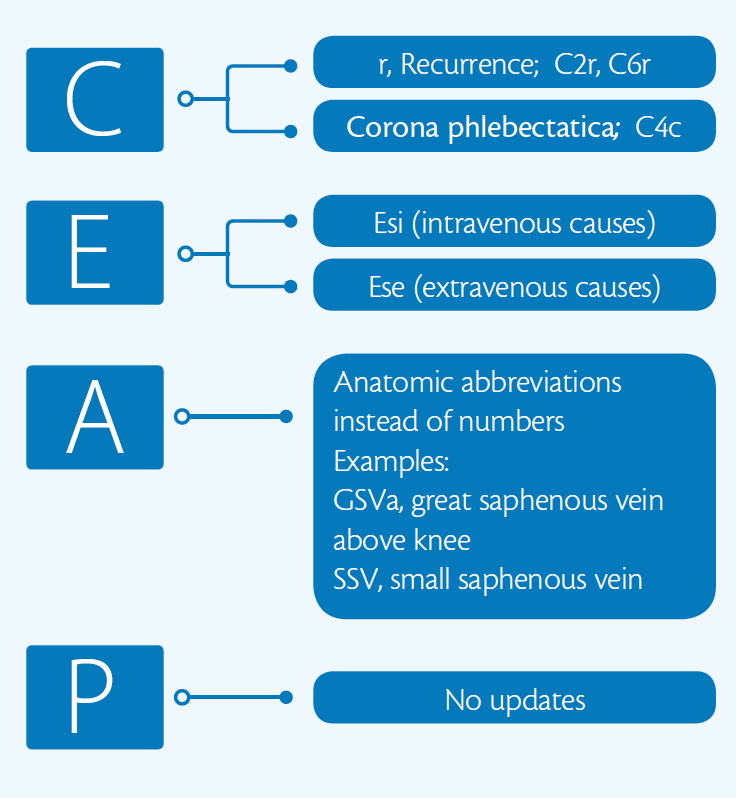
We understand that a classification system is basically a consensus document. It’s not a systematic analysis, although it includes this. As a consensus document, we follow the most appropriate methodology, which is the modified Delphi process. We initially split the task into four groups for each of the components of CEAP classification: clinical, etiology, anatomy, and pathology. There were several rounds of discussion for every suggestion made. A brief summary of changes can be seen in Figure 1.
Dr. Carman: Can you explain and discuss the differences between discriminative instruments and evaluative instruments? How does a discriminative instrument like CEAP improve our clinical practice?
Dr. Lurie: Discriminative instruments are designed to describe a condition, patient, or disease that is different from others. Using this instrument, you can place a patient into a certain category, which is different from another patient. The category that is assigned to a patient can and does change over time. At each point, a discriminative instrument helps to determine if this patient’s condition is different or the same. These instruments cannot be used to gauge the magnitude of a difference, to assess the severity of the condition, or to measure outcomes. They simply show if the condition is the same or if it is different. Evaluative instruments measure the severity of a condition, and its change over time or as a result of a treatment. They include quality-of-life questionnaires and severity scores, such as the Venous Clinical Severity Score.
CEAP classification is a discriminative instrument. Examination of a patient with chronic venous disease has to include a detailed description for each of the lower extremities. The CEAP classification provides a structure, helping to address all important aspects of the manifestations of chronic venous disease. The signs and the symptomatic status are components of the clinical class, or “C.” A complete description of a limb affected by chronic venous disease should always include the etiology, as well as the anatomic distribution of the changes, and whether it’s reflux obstruction or a combination of those. This is done routinely in each practice, but when you do it systematically, applying a CEAP classification, it will give you a structure and a simple way to communicate the results.
Dr. Carman: Possibly the most often used component of CEAP is the C or the clinical component. However, in the last two revisions, the etiology, anatomy, and physiology components are the ones that have really been expanded the most and have become more inclusive and descriptive in nature. From your perspective, do you find this more helpful clinically or from a reporting purpose? When we report expanded portions, particularly the anatomic and physiologic portions, we don’t really report those in a research fashion. What is the practicality of these ongoing extensions?
Dr. Lurie: That has been a contentious issue through the history of the CEAP classification. Let me address this from two perspectives—the research perspective and then the clinical perspective. As a clinical researcher, I incur the same issue repeatedly: We have a good question and we know we have enough experience with patients to address the question, but when we look at the medical records, we find gaps every time; we are not perfect. When we write the clinic note, we frequently miss something that becomes very important in the future. This is the most serious limitation of all retrospective studies; we do not systematically collect information.
Now, let me address this from the clinical perspective. For example, when we examine a patient with chronic venous disease with lipodermatosclerosis, we start looking at possible causes. We want to know whether it is a primary disease limited to superficial reflux, an obstructive disease in the femoropopliteal segment, or an obstruction in the iliac vein, because the treatment will be different for each setting. Identification and documentation of this information are components of appropriate clinical care. Those are the E, A, and P components of CEAP classification. Instead of writing an entire description of the patient and describing the ultrasound or other imaging findings every time, we simply can write a CEAP formula that has all this information included. In practice, it creates an easy structure to address the most important part of the disease.
Dr. Carman: What do you think are the top three strengths of the 2020 CEAP classification update?
Dr. Lurie: First, I think the most important update was done for etiology: a separate distinction for extravenous and intravenous causes of secondary disease. These conditions may look similar, with patients having the same signs and symptoms, but they require very different treatments. Sometimes clinical reports in the journals do not make sense because we do not know how many of the enrolled patients in a study have a disease caused by obesity or external compression versus how many were caused by as a sequela of deep vein thrombosis. I believe including the two subcategories of secondary chronic venous disease is one of the big strengths of the revised classification.
Second is the decision to replace the numbers in the anatomic description with commonly used abbreviations, which makes it a more natural language for the clinicians and makes CEAP easier to use. I do not believe that many practitioners remember that A4 in CEAP stands for the small saphenous vein. Replacing the number four with the abbreviation “SSV” can be really helpful, especially in combination with the “P” of CEAP. When it is written as “As, PrSSV” it clearly describes that only superficial veins are affected, and specifically that there is reflux in the small saphenous vein.
Third, the modifier R for recurrent varicose veins and recurrent ulcers is an excellent revision. Recurrent ulcers and recurrent varicose veins have different natural history and require different management compared with the first episode of ulceration or untreated varicose veins.
Dr. Carman: From your perspective, you know ulcers do not always recur in the same location. We do see patients who have had multiple episodes but not necessarily in the same location. Was there any consideration as to location of recurrence?
Dr. Lurie: Excellent question, and yes that was discussed several times. My experience is that a recurrent ulcer in the same location may be more of a chronic skin condition and not always associated with correctable venous abnormalities. On the contrary, a recurrence at a different location most often indicates ongoing problems with venous hemodynamics, often correctable by intervention. Including a location of the ulcer into CEAP may be a solution, but it will add to the complexity and make CEAP less usable. You’re absolutely right, chronic venous disease is not a simple disease, and sometimes the complexity should be sacrificed for practical reasons.
Dr. Carman: What do you see as the biggest limitation of the 2020 CEAP update?
Dr. Lurie: There are a couple significant limitations. The first is practicality—there is always a compromise. If you make it very practical, you sacrifice information, but if you are using too much information, it becomes impractical. That balance moves back and forth all the time. It is always going to be a limitation of any classification, including CEAP.
Another limitation is that CEAP is focused only on chronic venous disorders. We know that chronic conditions are sometimes the result of acute events, and acute conditions can complicate chronic disorders. For example, phlebitis can be a complication of varicose veins. It may be reasonable to include some of the complications in future revisions of CEAP. In order to do so, we need more information on the incidence of these conditions in patients with difference clinical classes and how these complications affect the disease natural history. The limitations of CEAP should be seen as an opportunity to explore relevant issues and improve the classifications in the future.
Dr. Carman: For the first consensus publication in 1996, the AVF sought endorsement from the joint council of the Society for Vascular Surgery (SVS) and the North American chapter of the International Society for Cardiovascular Surgery. You previously referred to the CEAP classification as a consensus documents, but given the expanding variety of clinicians involved in venous disease practice, why was this document limited to AVF society members without inclusion of other societies memberships in the panels or endorsements from other societies?
Dr. Lurie: First, I have to disclose that I am not talking on behalf of the AVF right now. You’re exactly correct. The history of CEAP classification is that it was initially developed at the Pacific Vascular Symposium. This went to the commission of the AVF, and it was finalized there as a consensus that did require the time, participation, and endorsement of all societies to make that totally new classification accessible and usable.
That was a very successful effort. Over time, however, the CEAP classification itself is no longer a consensus document; it’s a classification system that has been used for more than 20 years. It’s an instrument that was very well established and practically used, and the AVF owns that instrument. When it came to revision of this classification, there was no desire to have it be a complicated political process that might last a very long time without improving the classification.
The AVF has put together a very diverse task force for revision. Although the members of the task force are members of the AVF, they are also prominent members of other societies internationally and nationally. The task force is also substantial in size. Having said that, publication of this classification is an invitation for other societies and other practitioners to express their opinions and suggestions. More importantly, it is an invitation to actively participate with the AVF, investigate, and publish new evidence that supports suggested revisions.
Dr. Carman: Are there any plans for the AVF to work with larger electronic medical records companies to include the CEAP reporting standard and classification system as a module to facilitate reporting? The clinical researchers have a way to use prospectively collected data, even if it is in a retrospective manner and have the consistency that you are looking for or include it in the SVS database. Do you think that would help, or would that have a detrimental effect on advancing venous disease?
Dr. Lurie: It’s definitely going to be very helpful. We actually started working with the SVS Vascular Quality Initiative (VQI) to integrate the CEAP 2020 in using the venous modules of the VQI. As of June 2020, I learned that the revised CEAP classification was used as the web-based calculator that is very easy to use in Spanish, Italian, Portuguese, and Russian; however, it is not yet available in English.
If you use that calculator on your phone, it will be really practical. I look at a couple of those that I can understand (eg, https://ceap.phlebology-sro.ru/), and it’s really an easy tool to use in a clinical practice. It takes seconds to generate a complete CEAP and it will be very useful if it’s incorporated in the electronic medical records.
Advertisement
Advertisement