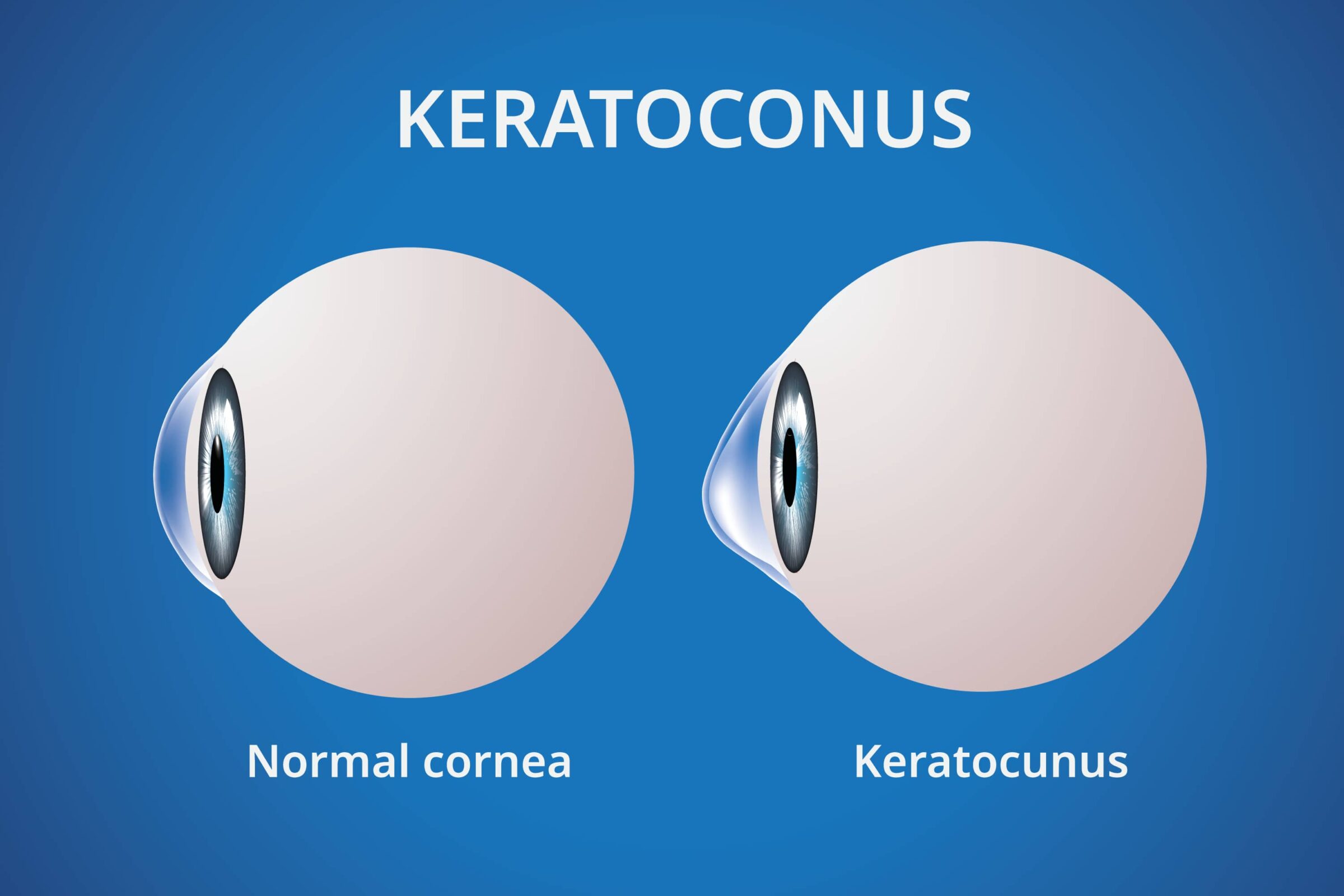
Keratoconus is a progressive eye condition resulting in a cone-shaped cornea which can cause poor vision and blurriness. Fortunately, there are several keratoconus treatments available to help manage the condition. These include corneal cross-linking, which strengthens the cornea and helps prevent further deterioration; intacs, which reshape the cornea; and contact lenses or glasses, which can help improve vision.
For those who have already experienced significant vision loss due to keratoconus, a corneal transplant may be an option. No matter what treatment you choose, it’s important to work with your doctor to find the best solution for your individual needs.
Who is At Risk for Developing Keratoconus?
Keratoconus is a degenerative condition that affects the curvature of the cornea, thinning and distorting its shape. It can cause blurry vision, light sensitivity, and other vision problems. People of all ages can be at risk for developing keratoconus, but it is most common in those between the ages of 10 and 25. Those with a family history of the condition are also more likely to develop it.
Early diagnosis and keratoconus treatments are essential in order to prevent further vision loss. If left untreated, the condition can worsen over time, leading to more severe vision problems. It is important to visit an eye doctor regularly so he can detect any changes in your vision. Early detection and treatment can help slow the progression of the condition and improve your quality of life. Additionally, it is important to follow any recommended treatments from your doctor in order to maintain optimal vision health.
Keratoconus Treatments
1. Intacs Inserts
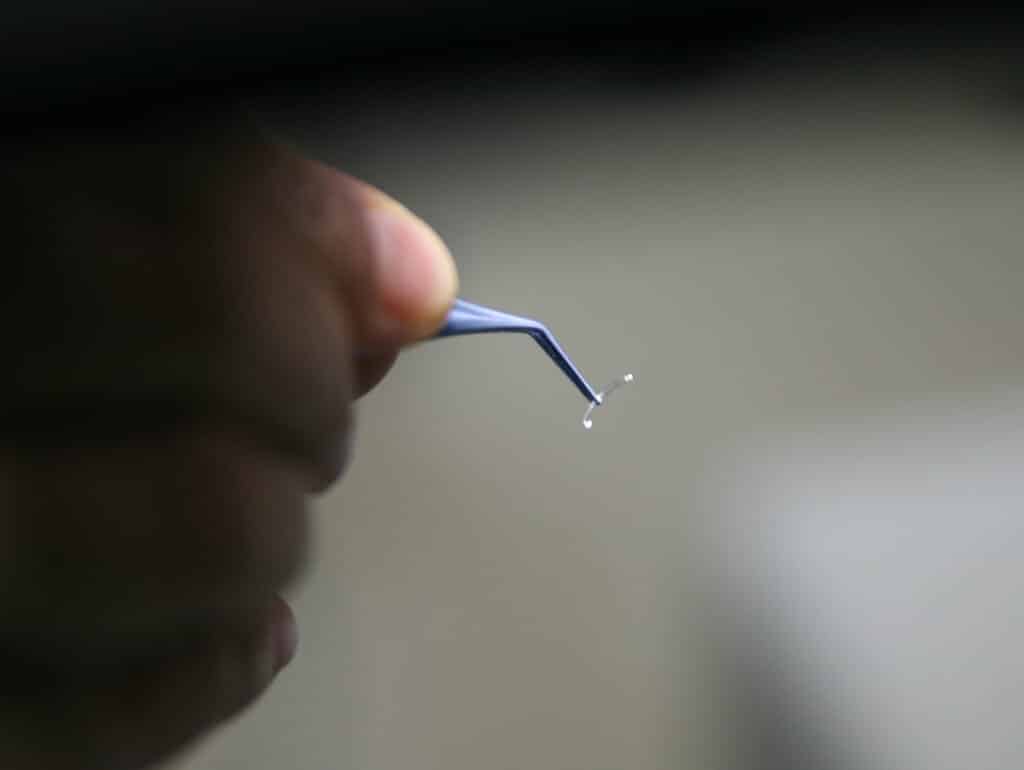
Intacs, or intracorneal rings, are small donor cornea tissue implants approved by the FDA for treating keratoconus. The surgeon insert these rings just below the epithelium and works by helping to shape the cornea back to its original form, allowing light to be appropriately focused on the retina. This can lead to improved vision with no need for glasses or contact lenses.
Intacs are a great option for those with keratoconus who want to avoid surgery. They can be inserted in a relatively short procedure and have been shown to enhance vision in many cases. The results of Intacs can last up to five years, and they can be replaced if necessary. Additionally, the risks associated with this procedure are minimal, making it an attractive option for those looking for vision correction without undergoing more invasive treatments.
Intacs results can last for up to five years and can be replaced if required Intacs can provide improved vision in a fast, simple procedure and have been proven successful in numerous cases
2. Corneal cross-linking (CXL)
Corneal cross-linking (CXL) is a treatment option for keratoconus patients who are experiencing light sensitivity, blurred vision, and other vision problems due to a diseased cornea. This procedure involves using ultraviolet light and riboflavin to strengthen the collagen fibers in the cornea, which helps to stabilize it and improve vision.
CXL is an effective keratoconus treatment, with many patients achieving excellent vision after the procedure. It is also less invasive than other treatment options such as corneal transplant surgery, making it an attractive option for those looking to improve their vision without undergoing a more invasive procedure. CXL can also be used in combination with Intacs or scleral lenses to further improve vision in those with advanced cases of keratoconus.
For those who have severe keratoconus, CXL can be used with Intacs or scleral lenses to optimize vision Corneal cross-linking strengthens the cornea through a UV light and riboflavin combination, improving eyesight

3. Corneal Transplant Surgery
Cornea transplants are a viable option for those struggling with vision loss due to advanced keratoconus. The procedure involves replacing the irregularly shaped cornea with donor tissue from a healthy eye, which can help restore clarity of vision. Eye doctors typically recommend this surgical procedure when other treatments such as soft contact lenses and scleral lenses fail to improve vision.
During the procedure, an eye surgeon will remove the diseased cornea and replace it with corneal tissue from a healthy eye. The success rate of corneal transplantation is high, but it is important to note that any type of surgery has its risks associated.
Additionally, the recovery process can be lengthy and may require multiple follow-up visits to ensure optimal results. It is also important to keep in mind that even after successful corneal transplantation, some patients may still need to wear glasses or contact lenses in order to achieve clear vision. For these reasons, it is important to discuss all treatment options with your corneal surgeon before deciding on a course of action.
4. Phototherapeutic keratectomy (PTK)
Phototherapeutic keratectomy (PTK) is a non-surgical treatment option for those with keratoconus who are experiencing decreased vision due to progressive eye disease. This procedure uses a laser to reshape the cornea and improve its shape, which can help improve vision. During the procedure, an ophthalmologist will use corneal topography to map out the corneal surface and then use a laser to remove any areas of irregularity or scarring. The goal of this procedure is to restore the normal curvature of the cornea and improve vision.
PTK has been shown to be an effective treatment for keratoconus, as it can help reduce light sensitivity, blurriness, and other symptoms associated with this eye condition. It is important to note that this procedure does not stop the progression of keratoconus but can help slow it down by improving the corneal shape.
5. Conductive Keratoplasty (CK)
Conductive Keratoplasty (CK) is a minimally invasive procedure to treat keratoconus. This procedure uses radiofrequency energy to reshape the entire cornea and improve vision. During the procedure, an ophthalmologist will use a special device to apply heat to specific areas of the cornea in order to reshape it and improve its curvature. The goal of this procedure is to reduce astigmatism and improve vision.
Before undergoing CK, patients should have a comprehensive eye exam to ensure that they are good candidates for the procedure. It is also important to discuss all potential risks and benefits of the surgery with your doctor before making any decisions about treatment. After the surgery, patients may need to wear glasses or contact lenses in order to achieve optimal vision results. Additionally, regular follow-up visits with an eye doctor are necessary in order to monitor progress and ensure that the reshaped cornea is functioning properly.
6. Soft Contact Lenses
Soft contact lenses are a non-surgical option for those with keratoconus. These lenses fit over the irregularly shaped cornea and provide improved vision. Hybrid lenses, which combine both soft and rigid materials, are necessary in cases of advanced keratoconus as they can provide better vision than traditional soft contact lenses. Soft contact lenses come in a variety of shapes and sizes to accommodate different corneal diseases. Depending on the severity of the condition, patients may need to wear special contact lens shapes specifically designed for keratoconus.
In addition to providing improved vision, soft contact lenses can also help reduce light sensitivity and blurriness associated with keratoconus. They can work in combination with other keratoconus treatments such as Intacs or scleral lenses to further improve vision in those with advanced cases of keratoconus. It is important to note that while soft contact lenses can help improve vision, they do not stop the progression of the disease but can help slow it down by providing better vision.
For those struggling with vision loss due to keratoconus, a soft contact lens may be an effective treatment option. While these lenses cannot cure the condition, they can provide improved vision and reduce light sensitivity and blurriness.
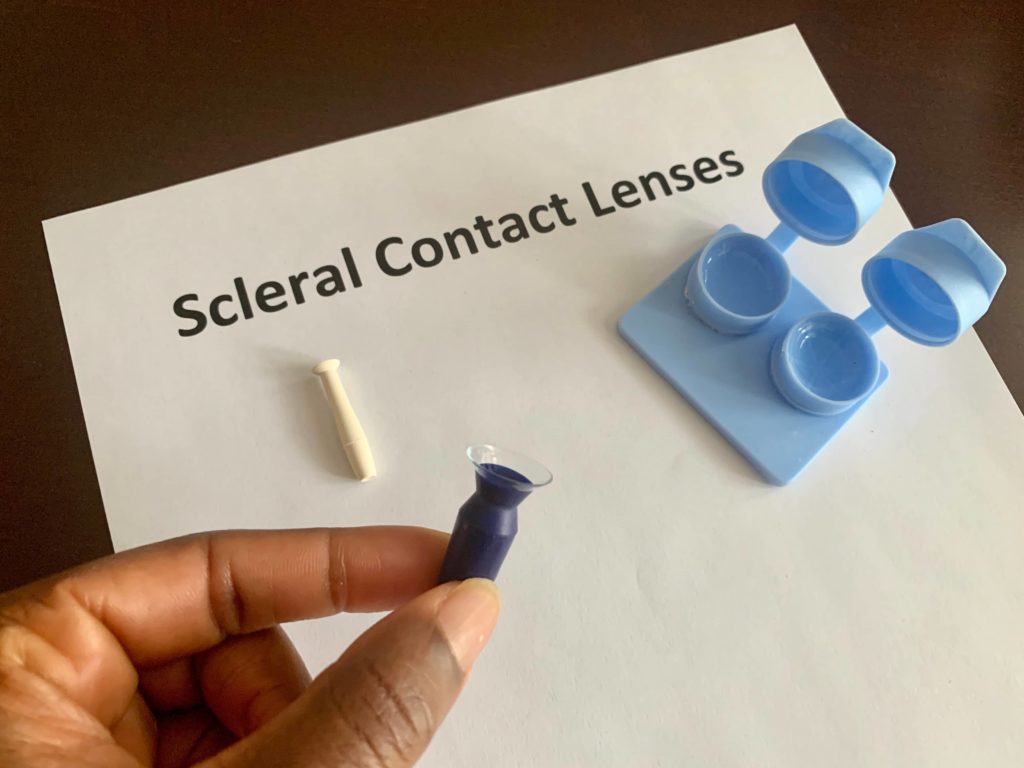
7. Scleral Lenses
Scleral contact lenses are a type of contact lenses that are larger than traditional soft contact lenses and provide improved vision for those with distorted vision due to this condition. These lenses are made from a rigid material that is able to conform to the eye’s irregular shape, providing better vision than traditional soft contact lenses. Additionally, these lenses can help reduce light sensitivity and blurriness associated with keratoconus.
In order to determine if scleral contact lenses are an appropriate treatment option for keratoconus, patients must first undergo an eye exam in order to assess their condition and determine the best type of lens for them. This exam will evaluate signs of keratoconus such as thinning or steepening of the cornea in order to determine if scleral contact lenses are a viable option. If so, then an eye contact lens fitting will be performed in order to ensure that the lens fits properly and provides optimal vision results.
Once fitted correctly, scleral contacts can provide improved vision for those struggling with vision loss due to keratoconus.
Scleral contact lenses are made from a firm material that fits the eye’s shape, improving vision more than regular soft contacts A comprehensive eye exam is required to determine if scleral contact lenses are the best solution for people with keratoconus.
8. Rigid Gas Permeable Contact Lenses
Rigid gas permeable contact lenses fit over the irregularly shaped cornea caused by keratoconus. Additionally, permeable lenses can help reduce light sensitivity and blurriness associated with keratoconus. In order to determine if RGP contact lenses are an appropriate treatment option for keratoconus, patients must first undergo an eye exam in order to assess their condition and determine the best type of lens for them.
The purpose of this test is to assess evidence of keratoconus, like thinning or warping of the cornea, in order to decide if rigid gas-permeable contact lenses are viable options.
Lifestyle Changes Necessary After Keratoconus Treatments
After treatment for keratoconus, it is important to make lifestyle changes in order to ensure the best possible outcome. These changes include avoiding activities that may result in a damaged cornea, such as rubbing or touching the eyes, and wearing protective eyewear when engaging in sports or other activities that may pose a risk of eye injury. Additionally, it is important to follow up with regular eye exams in order to monitor any changes in vision and ensure that the contact lenses are still providing optimal vision.
Finally, it is important to practice good hygiene habits when handling and caring for contact lenses in order to reduce the risk of infection or irritation. By making these lifestyle changes, cornea transplant Hawaii patients can help ensure their vision remains clear and stable.
Ready for a consultation?
If you are looking for treatment options and want state-of-the-art eye treatment for your keratoconus disease, you will need a doctor with experience. The keratoconus specialists at EyeSight Hawaii in Honolulu, HI, and Maui, HI have the knowledge to help. Make an appointment online or call our office to schedule a consultation today!