Pamela Dibblee, Meynard Enriquez, Cameron Hui, Robert Lontz, Nancy Mulligan, Peter Trujillo
Glenohumeral Osteoarthritis: Introduction and Background

The incidence of glenohumeral osteoarthritis is 4.6% of all shoulder pain and 0.4% of all orthopedic conditions. The incidence of glenohumeral osteoarthritis in adults over the age of 65 is 16-20%.2 Post anterior stabilization procedure of the shoulder, the incidence of glenohumeral osteoarthritis increases to 15-20% in all patients with shoulder pain.2
Glenohumeral osteoarthritis is characterized by progressive narrowing of the joint, narrowing of the articular cartilage and osteophyte formation. In late stage glenohumeral osteoarthritis, there is a loss of articular cartilage and bony destruction.8 Various causes may lead to the onset of glenohumeral osteoarthritis, including primary osteoarthritis and secondary causes such as trauma leading to dislocation/subluxation, post-inflammatory conditions, iatrogenic factors.18
Risk factors for glenohumeral osteoarthritis, or shoulder arthritis, include age, greater than 60 years old, excessive joint loading and joint injury.8 Recurrent dislocation or subluxations can lead to articular cartilage damage.18 Proximal humeral fractures can lead to early degenerative changes at the glenohumeral joint.18 A small percentage of patients with massive rotator cuff tears develop arthropathy.3 Patients with a history of sickle cell, radiation therapy, oral steroid use and lipid metabolism disorders are at risk for higher rates of OA.18
The rate of glenohumeral osteoarthritis progression has not been determined.2 The amount of cartilage loss is not directly related to patient symptoms.2 The impact of glenohumeral osteoarthritis on quality of life has been documented as depression at 15.2% and anxiety at 19.5% in a cohort of patients with glenohumeral osteoarthritis.6
It is recommended that physical therapy should be part of a multidisciplinary approach to the treatment of complex shoulder pain from glenohumeral osteoarthritis. There is no consensus or specific recommendations on treatment model with respect to frequency of dosage.
Glenohumeral Osteoarthritis: Shoulder Anatomy/Physiology
The shoulder is a complex ball and socket joint responsible for articulation of the upper extremities with the axial skeleton.4 The glenohumeral joint is highly reliant on soft tissue for stability. The glenohumeral joint consists of bony anatomy involving the scapula, glenoid fossa and humeral head. Nearby/surrounding structures of the glenohumeral joint include the labrum, capsule, and anterior ligaments (superior, middle, inferior), which provide restraints for humeral head translation.
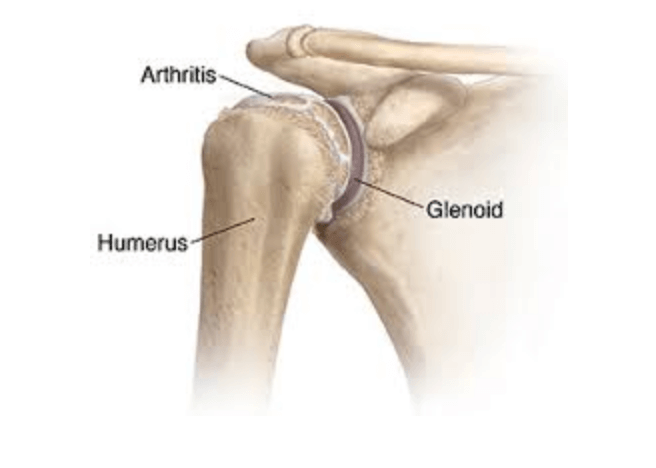
Cartilage thickness varies on both the glenoid and humeral head. The glenoid has thicker cartilage along its edges, greatest at the anterior inferior edge while the humeral head has the thickest hyaline cartilage at the center; this leads to increased congruency of the joint.2 In glenohumeral osteoarthritis, or shoulder arthritis, the first area affected is the posterior glenoid and center of the humeral head.2 Due to capsular thickening and possible contracture and internal rotation deficit may occur with glenohumeral osteoarthritis, leading to increased erosion of the posterior glenoid. The lack of joint congruency leads to abnormal loading of the cartilage and increased degeneration.2
The glenohumeral joint relies on muscular force couples for stability leading to balance of the humeral head within the glenoid.11 The rotator cuff acts to stabilize the humeral head in the glenoid via compression as well as depresses the humeral head during elevation.9 Approximately 4% of patients with massive rotator cuff tears develop arthropathy.3 Characteristics of rotator cuff arthropathy are rotator cuff insufficiency, glenohumeral joint degeneration, and superior migration of the humeral head.3 Superior migration of the humeral head results in incongruence of the joint and increased wear on the glenoid fossa.3
Glenohumeral Osteoarthritis: Diagnosis, Signs, Symptoms, and Common Impairments
Patients with glenohumeral osteoarthritis typically chronic pain that has been present for > 6 months, described as deep pain in the joint, related to activity, progressive, often localized posteriorly, that can be present at night that interferes with sleep. In more advanced stages, chronic swelling and joint stiffness are present that may limit functional limitations. The presence of glenohumeral osteoarthritis should be suspected with patients greater than 50 years old with chronic shoulder pain, stiffness that worsens with activity and improves with rest, swelling and joint enlargement, tenderness at shoulder joint line with or without crepitus, decreased mobility of the shoulder, particularly in external rotation and abduction.5, 16
Common positive exam findings indicating potential for glenohumeral osteoarthritis include painful crepitus, joint enlargement, tenderness at the joint line, swelling and possible audible and palpable grinding when a mechanical stress is placed on the joint.5, 16 Decreased passive and active range of motion especially with external rotation and abduction, and palpable grinding when a mechanical stress is placed on the joint during advanced progression of glenohumeral osteoarthritis.16

A negative shrug sign may rule out glenohumeral osteoarthritis. A positive shrug sign is noted when a patient is unable to abduct the arm to 90 degrees without elevating the entire scapula or shoulder girdle. The shrug sign had a sensitivity of 90.5% with a negative likelihood ratio of 0.167 and a specificity of 56.8% with a positive likelihood ratio of 2.092 in determining glenohumeral osteoarthritis. It is important to note that the shrug test also has high sensitivity (94.7%) and low specificity (49.5%) in confirming frozen shoulder;12 therefore, skilled differential diagnosis is important. Differential diagnosis with complex shoulder pain and glenohumeral osteoarthritis includes bursitis, rotator cuff disease, bicep tendonitis, calcific tendonitis, idiopathic adhesive capsulitis, rheumatoid arthritis, gout or a septic joint. Radiograph is the primary test used to confirm glenohumeral osteoarthritis.16
Glenohumeral Osteoarthritis: Multidisciplinary Considerations
Concerning multidisciplinary management of the osteoarthritic shoulder, three main areas emerge in the research; imaging, pharmacological interventions and surgical interventions.
Imaging
According to Millet et al, the primary imaging confirming diagnosis of shoulder osteoarthritis or glenohumeral osteoarthritis is axial radiography. In this view, the authors state that it is the best way to accurately determine the severity of joint space narrowing as well as rule out dislocation. The severity of joint space narrowing with glenohumeral osteoarthritis becomes important in any future determinations of appropriate surgical interventions. Spencer et al compared MRI with arthroscopy in detecting cartilage abnormalities of the glenohumeral joint. In detecting humeral lesions, the sensitivity is 32% and specificity is 80%. The sensitivity in detecting glenoid lesions was 31% and the specificity was 86% indicating moderate accuracy of the MRI in detecting articular damage in patients diagnosed with subacromial pathology is moderate.
Pharmaceutical
The American Academy of Orthopaedic Surgeons state that they are “inconclusive” on the use of medications and injections for managing glenohumeral osteoarthritis. Meaning, they cannot confirm nor deny the effectiveness based on the current evidence. However, there are studies that advocate the use of oral acetaminophen, COX-2 selective inhibitors and potentially, glucosamine.
In a review by Takamura et al, dosages of 1g of acetaminophen 3-4 times per day resulted in decreased pain versus placebo. Also, NSAIDs were found to be superior to acetaminophen, but had increased gastrointestinal and cardiovascular side-effects. They were unable to recommend glucosamine, chondroitin sulfate, vitamins and herbal treatments due to the scarcity of supporting evidence. Millet et al had similar findings in that acetaminophen was to be considered a first line of defense medication due to its relative effectiveness and minimal risk. Millet et al further supported the use of COX-2 selective inhibitors if the patient was free of cardiovascular disease, as they showed an equal outcome to NSAIDs with less gastrointestinal side-effects. Millet et al supports some glucosamine use as the outcomes were slightly better than placebo but cautions as there is no solid evidence purporting its use. Interestingly, Ansok et al reported the use of topical capsaicin had beneficial effects over placebo in treatment of osteoarthritis of the knee with very few side effects and considering the low risk, recommended potential use for shoulder osteoarthritis pending further research.
In considering injections, Ansok et al found that hyaluronic acid injections resulted in a statistically significant increase in ROM and decrease in pain. However, these findings were derived from small study sizes and complications were demonstrated with diabetic patients and with the development of septic arthritis. Concerning corticosteroid injections, Takamura et al reported that these injections had a short-term decrease in pain, but a potential 17% chance of tendon weakening in 3 months. Additionally, they found that visco-supplementation resulted in some improvement in pain and ROM at six months and found no solid support currently for the use of protein-rich plasma nor stem cell injections.
Surgical
According to the American Academy of Orthopaedic Surgeons, there is “limited” evidence in the literature to support the procedures of total shoulder arthroscopy versus hemiarthroplasty, keeled or pegged polyethylene cemented glenoid prosthesis, and whether to avoid a shoulder arthroplasty from a surgeon that performs less than 2 per year. Their position is “inconclusive” with respect to biceps tenotomy / tenodesis, subscapularis versus lesser tuberosity approach for a total shoulder arthroplasty as well as any specific type of humeral prosthesis or fixation method. There is consensus on the total shoulder arthroplasty being superior to hemiarthroplasty as the benefits outweigh the harm.

Millet et al supports this position as they found that total shoulder replacement was superior to hemiarthroplasty in the high survivorship of the implant from long term studies on. Ansok et al reports a total shoulder survival rate of up to 93% in 10 years and 87% in 15 years, compared to hemiarthroplasty revision rates of 30% in 10 years with a 47% unsatisfactory conversion rate to total shoulder replacement.
However, the treatment of the younger population affected by shoulder osteoarthritis, or glenohumeral osteoarthritis, remains controversial. Takamura et al describes several less invasive surgical procedures for the younger patient including arthroscopy, microfracture, osteochondral grafting and autologous chondrocyte implantation.
According to Takamura et al, arthroscopy resulted in a temporary decrease in pain and increase in ROM with an ideal candidate having a small unipolar lesion, adequate joint space, and no large osteophytes. Risk factors for failure of this procedure include < 2mm joint space, grade IV bipolar disease, and presence of > 2cm osteophytes. Chondral replacement procedures include microfracture and grafting. Microfracture was warranted in those with small lesions that had not yet eroded into the subchondral plate, but this substitutes fibrocartilage for hyaline. Osteochondral grafting was conceptually an improved way to replace hyaline cartilage but resulted in high risks of infection and had a reported failure rate of up to 50% in 2 years. Autologous chondrocyte implantation involves harvesting chondrocytes from non-weight bearing areas of other joints, growing them artificially for 4-6 weeks, then implanting the cells in the chondral defect covering the area with a membrane for support. This procedure has high failure rates and requires donor and recipient surgical areas. In summary, the author recognized the need for further outcomes research to substantiate each of these procedures.
Millet et al reported on the CAM procedure as a potential solution to the younger patient suffering with glenohumeral osteoarthritis. The CAM procedure is an arthroscopic joint preserving surgical procedure that is a combination of several procedures including: glenohumeral chondroplasty, loose body removal, microfracture, humeral osteoplasty, capsular release (anterior, inferior, posterior), subacromial decompression, axillary nerve neurolysis and biceps tenodesis. For this procedure, there are reports of up to 85% survivorship at 2 years, indicating a reasonable option for the younger population that meets the criteria for success. Like the traditional arthroscopic procedures, patients with < 2mm joint space had a significantly higher failure rate and were almost 8x as likely to proceed to a total shoulder replacement following the CAM intervention.16
Glenohumeral Osteoarthritis: Physical Therapy Considerations
Glenohumeral Osteoarthritis: Educational Considerations
Based on expert opinion, it is recommended that patients are educated on the arthritic process, overall prognosis, and avoid focusing on the pathoanatomy of glenohumeral osteoarthritis.8,18 Education on shoulder arthritis should also include activity modification, including limiting loading and repetitive motion over head and in other provocative positions.18 Lifestyle interventions may assist with managing glenohumeral osteoarthritis. General guidelines for patients with glenohumeral osteoarthritis include remaining active, maintaining good sleep hygiene, smoking cessation, and regular exercise.14
The pathogenesis of glenohumeral osteoarthritis involves inflammatory and degradative reactions which ultimately lead to and contribute to progressive structural damage to bone and cartilage of the joint.14 Mechanical and infectious insult to chondrocytes in cartilage provoke an inflammatory response, wherein inflammatory cytokines, such as interleakin1-beta, leukotrienes, and nitric oxide synthase contribute to degradation of cartilage.1 The synovium may also produce a similar inflammatory response, further triggering the presence of leukotrienes and proteases which hasten disease progression. As cartilage breaks down from mechanical or enzymatic assault, release of collagenase, an enzyme that further facilitates the body’s response to breaking down tissue, may occur. This contributes to the progression of cartilage degradation.1 The understanding of these processes and the common theme of inflammation are important considerations during treatment and management of glenohumeral osteoarthritis. In the Shoulder Pain and Mobility Deficit: Adhesive Capsulitis Guideline, the authors discuss the concept of irritability guiding treatment intervention.13 Though there are no current recommendations or evidence to support the concept of irritability in glenohumeral osteoarthritis, expert opinion regarding activity modification could be extrapolated to physical therapy interventions for shoulder arthritis; modifying manual therapy and treatment interventions to reflect appropriate tissue loading may help minimize an adverse outcome.
Glenohumeral Osteoarthritis: Exercises and Manual Techniques
Specific exercise prescription for glenohumeral osteoarthritis is not well supported in literature or has some inconsistencies. Saltzman et al notes that evidence on physical therapy for glenohumeral osteoarthritis is scarce and in some cases strengthening exercises may lead to worsening of symptoms. The initial management of shoulder pain can be seen as relatively simple. Millet et al reported that the initial management of shoulder pain should consist of a trial of rest, activity modification, patient education, physical therapy for motion and strengthening exercises, because these modalities are inexpensive, pose minimal risk, and may mitigate patient symptoms. Some consideration should be made to the acuity and irritability of symptoms associated with glenohumeral osteoarthritis for appropriate non-surgical intervention and post-operative exercise prescription.16
Recommendations for physical therapy interventions include focusing on periscapular and shoulder strengthening, stretching,distraction/manual therapy, and range of motion.18 It has been suggested that prescribed home exercises for glenohumeral osteoarthritis should reinforce the aim of manual techniques.8 In acute stages during which movement may not tolerated, strengthening of the contralateral upper extremity has been shown to improve affected limb strength by 9.4%.15 Physical therapy intervention and patient management should also consider inflammatory process occuring with glenohumeral osteoarthritis and utilize an impairment-based approach targeting individual patient impairments.1,8 Furthermore, consideration of regional pain outside the shoulder may be effective in reducing overall symptoms, such as in the thoracic spine.10
The videos below can give the clinician some ideas on exercises and manual treatment, but are not meant to be a protocol for glenohumeral osteoarthritis. Additionally, exercises may not be appropriate for those with total shoulder arthroplasty.
[cycloneslider id=”glenohumeral-osteoarthritis”]
References
- Ansok C, Smith JM. Optimal Management of glenohumeral osteoarthritis. Orthopedic Research and Reviews. 2018;10:9-18.
- Bakhsh W, Nicandri G. Anatomy and Physical Examination of the Shoulder. Sports Med Arthrosc Rev. 2018;26(3):e10-e22.
- Cho CH, Song KS et al. Changes in psychological status and health-related quality of life following shoulder arthroplasty. JBJS am. 2017;99(12)1030-1035.
- Clark J, Sidles JA, Matsen FA. The relationship of the glenohumeral joint capsule to the rotator cuff. Clin Orthop Relat Res. 1990;(254):29-34.
- Crowell M, Tragord B. Orthopedic Manual Physical Therapy for shoulder pain and IMpaired Movement in a patient with Glenohumeral Joint Osetoarthritis: A Case Report. JOSPT
- Howard PD, Comly L, Hetrick J, Kirsch K, Kuczynski L, Veacock D. The Effect of Thoracic Manipulation on Shoulder Pain: A Systematic Review. Orthopaedic Physical Therapy Practice. 2015;27(4):214-219.
- Inman VT, Saunders JB, Abbott LC. Observations on the function of the shoulder joint. 1944. Clin Orthop Relat Res. 1996;(330):3-12.
- Kelley MJ, Shaffer MA, Kuhn JE, et al. Shoulder Pain and Mobility Deficits: Adhesive Capsulitis. Journal of Orthopaedic & Sports Physical Therapy. 2013;43(5). doi:10.2519/jospt.2013.0302.
- Kentaro O, et al. Osteoarthritis: A Critical Review. Crit Rev Phys Rehabil Med. 2012 ; 24(3-4): 251–264
- Manca A, Dragone D, Dvir Z, Deriu F. Cross-education of muscular strength following unilateral resistance training: a meta-analysis. European Journal of Applied Physiology. 2017;117(11):2335-2354.
- Millet PJ, Gobezie R, Boykin RE. Shoulder Osteoarthritis: Diagnosis and Management. Shoulder Osteoarthritis: Diagnosis and Management. 2008; 78 (5).
- O’Brien SJ, Schwartz RS, Warren RF, Torzilli PA. Capsular restraints to anterior-posterior motion of the abducted shoulder: a biomechanical study. J Shoulder Elbow Surg. 1995;4(4):298-308.
- Saltzman B, et al. Glenohumeral Osteoarthritis in the Young Patient. J Am Acad Orthop Surg. 2018;26(17):e360-370.
- Tangtrakulwanich B. Analyses of possible risk factors for subacromial impingement syndrome. World Journal of Orthopedics. 2012;3(1):5. doi:10.5312/wjo.v3.i1.5.


