“Doctor, my tummy is bloated. I think it’s heartburn. It’s been going on for months. What’s causing it?”
Good question. Let’s dive in.
What is dyspepsia?
Upper abdominal pain or discomfort originating in the upper GI tract that is episodic or persistent and often associated with belching, bloating, heartburn, and nausea or vomiting.
What is the difference between dyspepsia and GERD?
What are the DDx of dyspepsia?
Albeit some overlap, the organic causes can be categorized as follows:
| Metabolic | Peptic Ulcer Disease (PUD) Gastroesophageal reflux disease (GERD) Hypercalcemia, hyperkalemia |
| Malabsorption | Carbohydrate malabsorption |
| Neurogenic | Gastroparesis |
| Neoplastic | Gastric or Esophageal Cancer Hepatocellular Carcinoma Pancreatic Cancer |
| Inflammatory | Pancreatitis |
| Infectious | Bacterial: H. Pylori (resulting in GERD) Parasites: Giardia, Strongyloides |
| Medication-induced | antinflammatories: NSAIDs, glucocorticoids, colchicine supplements: potassium, iron, niacin oral antibiotics: esp ampicillin, erythromycin narcotics digitalis, theophylline gemfibrozil quinidine estrogens levodopa |
| Systemic | Diabetes Mellitus Thyroid and Parathyroid disorders Connective Tissue Diseases Infiltrative diseases ex. Crohns, Sarcoidosis |
| Vascular | Ischemic bowel disease Celiac artery compression syndrome Superior mesenteric artery syndrome |
| Referred Pain | Biliary pain Chronic abdominal wall pain |
What are alarm symptoms of dyspepsia?
Certain factors in the HPI / ROS should raise a red flag.
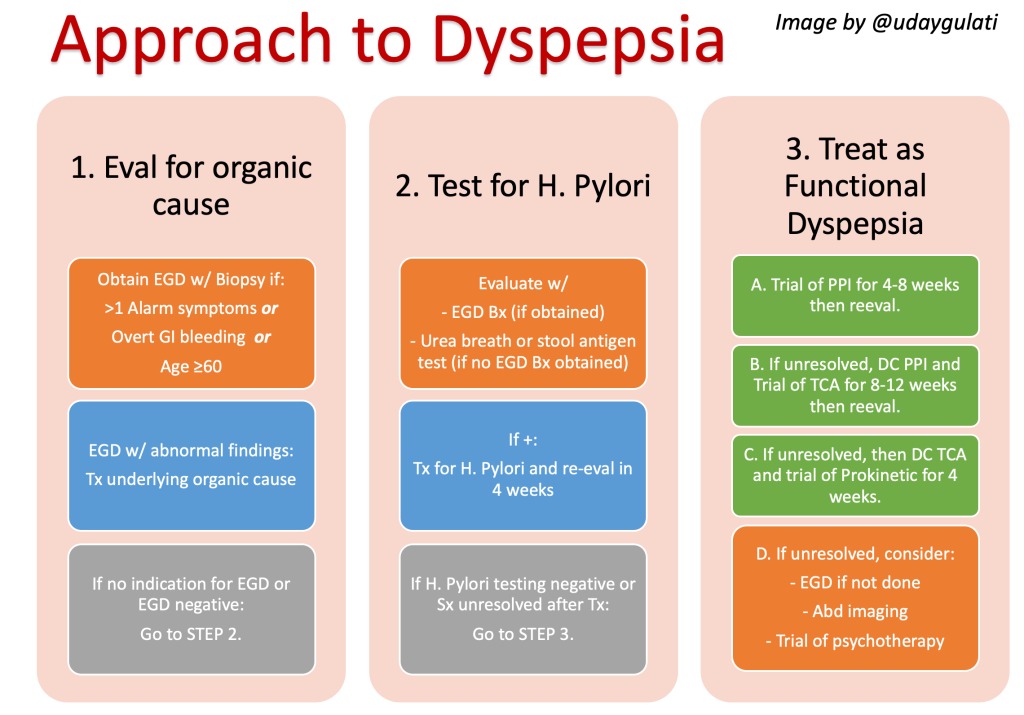
These alarm symptoms, along with age ≥60, warrant a further invasive workup with an EGD and biopsy to rule out one of the above organic causes, specifically the neoplastic causes. This should be performed earlier than later.
| Dysphagia (difficulty swallowing) |
| Odynophagia (painful swallowing) |
| Persistent vomitting |
| Unintentional weight loss |
| FHx of Upper GI Malignancy |
| Unexplained iron deficiency anemia (IDA) |
| Palpable mass or lymphadenopathy |
What about H. Pylori testing?
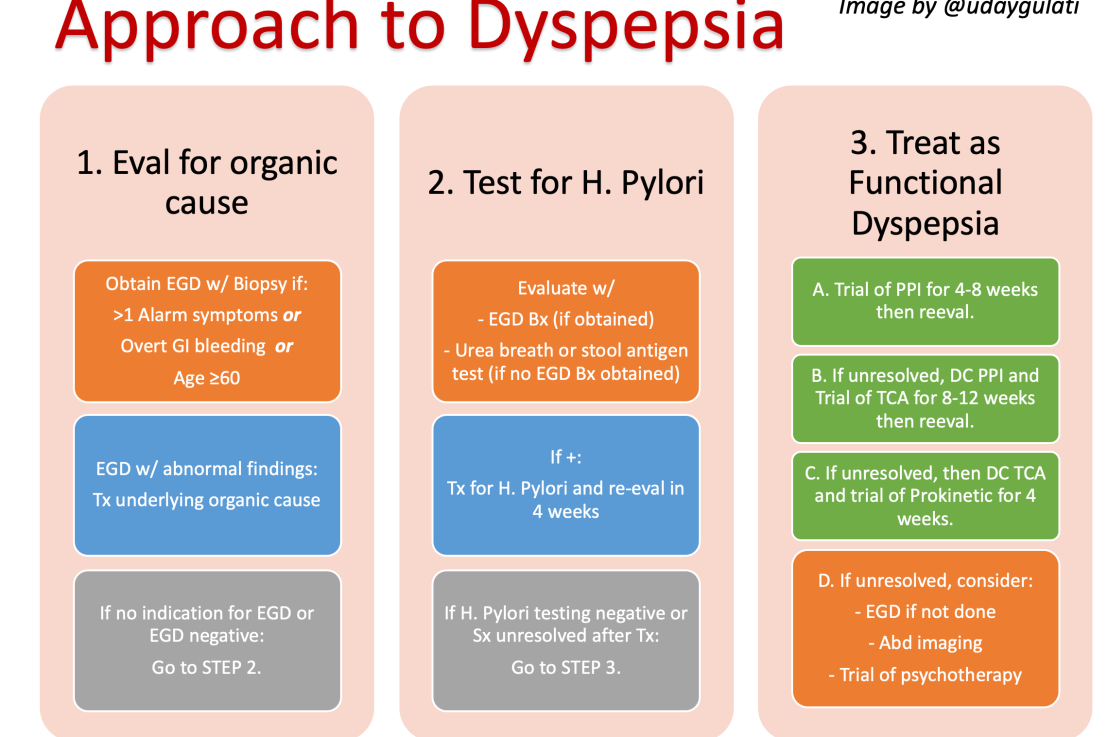
Helicobacter pylori is a common cause of PUD and treatable. Therefore, we test for it. If the EGD w/ biopsy was obtained, treat if positive. If it wasn’t obtained, still test for it with a urea breath test or stool antigen assay. Recall, the serologic test has a low PPV so do not order it.
If positive, treat with quadruple (Bismuth, metronidazole, tetracycline, PPI) or triple therapy (Clarithromycin, amoxicillin or metronidazole, PPI). Retest 4 weeks after treatment to confirm eradication.
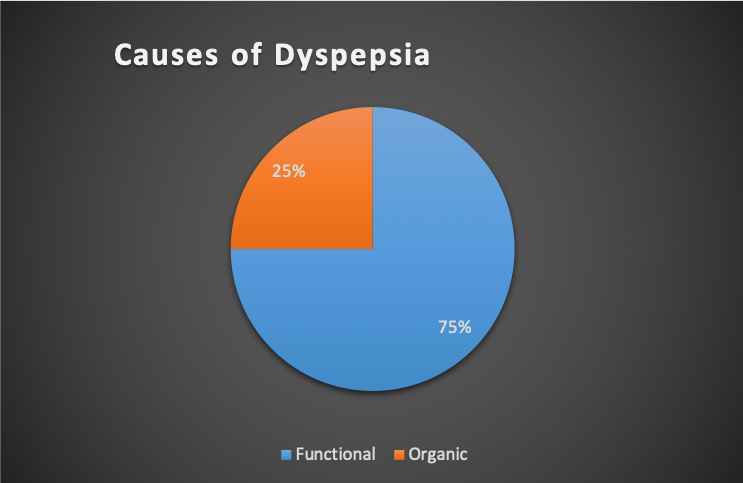
What about functional dyspepsia?
It’s a diagnosis of exclusion but doesn’t require full organic exclusion. If there are no alarm symptoms and are <60, you can proceed with H.Pylori testing. If negative, it’s likely functional.
Specifically, the American College of Gastroenterology (ACEG) recommends using the following standard for Diagnosis of Functional Dyspepsia.
It requires:
≥1 of the following for 3 months prior w/ Sx onset ≥6 months ago:
- bothersome postprandial fullness
- bothersome early satiation
- bothersome epigastric pain
- bothersome epigastric burning
AND no evidence of organic, systemic, metabolic or structural disease to explain symptoms i.e. negative EGD.
Pearl: look out for other GI conditions that mimic dyspepsia, such as IBS, that can also coexist with functional dyspepsia.
How do you treat functional dyspepsia?
Its a simple ladder. If the first does not work, discontinue and try the next.
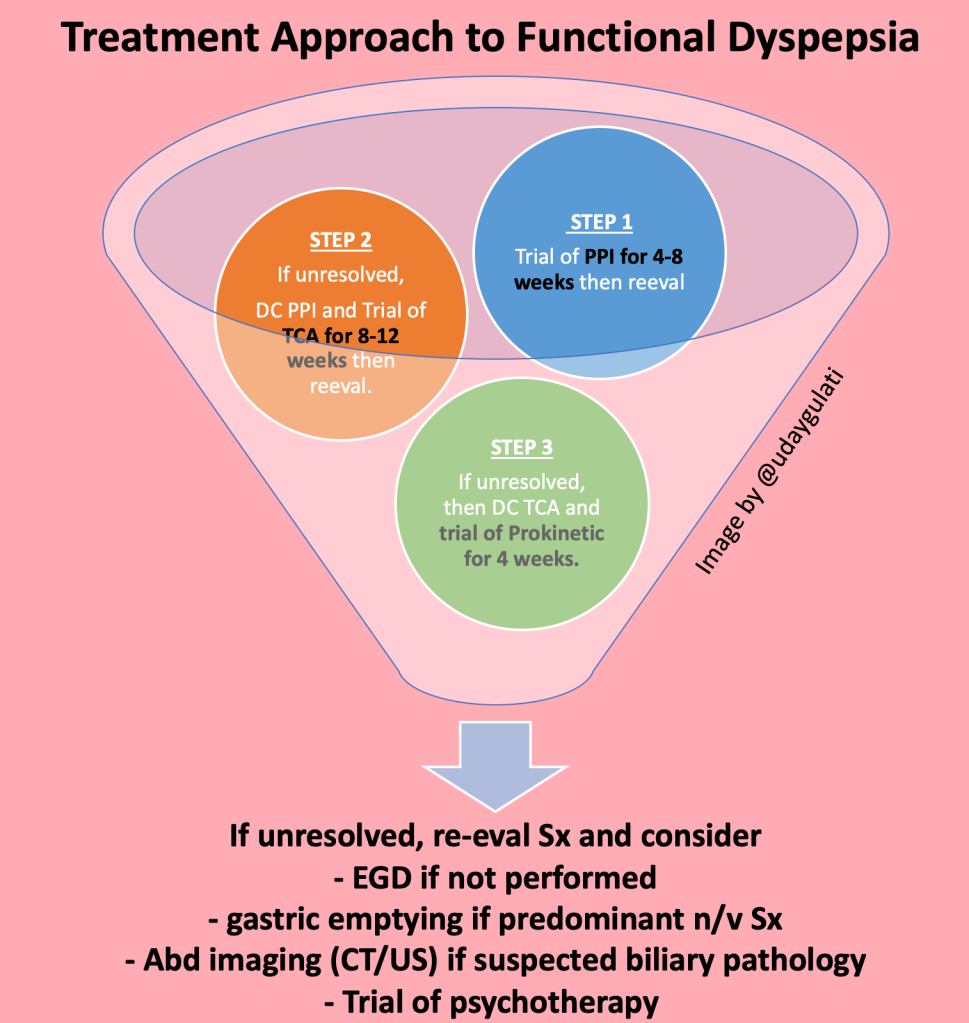
In Summary…
- consider organic causes in your differentials
- rule out red flags symptoms and consider the need to obtain an EGD
- rule out H. pylori if EGD negative or not obtained
- Treat functional dyspepsia using the PPI > TCA > Prokinetic ladder
References
*American College of Gastroenterology and Canadian Association of Gastroenterology guidelines Reference -> Moayyedi P, Lacy BE, Andrews CN, et al. ACG and CAG Clinical Guideline: Management of Dyspepsia. Am J Gastroenterol 2017; 112:988.
Bytzer P, Talley NJ. Dyspepsia. Ann Intern Med 2001; 134:815.
Heading RC. Definitions of dyspepsia. Scand J Gastroenterol (Suppl). 1991;182:1–6.
Stanghellini V, Chan FK, Hasler WL, et al. Gastroduodenal Disorders. Gastroenterology 2016; 150:1380.
Post reviewed and edited by @udaygulati