CHIRONIAN NEW YORK MEDICAL COLLEGE SUMMER / FALL 2015
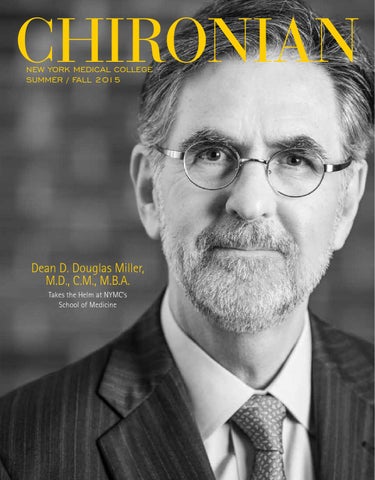
Dean D. Douglas Miller, M.D., C.M., M.B.A. Takes the Helm at NYMC’s School of Medicine
Message from the Chancellor AN INSTRUCTIVE VACATION IN CURAÇAO The trouble with humanity, Richard Weaver commented, is that it keeps forgetting to read the minutes of the last meeting.1 Academic health care has the same problem. One hundred and five years ago, Abraham Flexner published a withering and trenchant analysis of American medical education. The so-called “Flexner Report” decried for-profit medical education and lead to the disappearance of for-profit medical schools in the U.S.2 Recently Mrs. Halperin and I spent a few days of vacation in Curaçao, located just north of the Venezuelan coast. Curaçao is an island, approximately 23 miles long and 5 miles wide. It has a relatively autonomous government with its own governor, prime minister, and parliament, while remaining under Dutch rule in certain areas of governance. The population of 150,000 is equivalent to the population of cities such as Paterson, N.J. or Pomona, Calif. There is a 375-bed hospital on the island. There are four for-profit medical schools on the island of Curaçao marketing themselves to U.S. students. None require applicants to take the Medical College Admissions Test (MCAT), one does not require a bachelor’s degree, and interviews are conducted by telephone. Depending on how and when you count, there are between 35 and 60 for-profit medical schools in the Caribbean offering seats to U.S. citizens who cannot gain admission to U.S. M.D. or D.O. schools. Most U.S. schools admit between 40 and 250 students per year. One of the Caribbean schools admits 1,000 students per year. Students at the for-profit Caribbean schools pass Step 1 of the U.S. national medical boards on the first attempt at a rate of 19 percent to 84 percent, depending upon the school.3 New York Medical College (NYMC) M.D. students pass Step 1 of the boards at a rate of 96 percent to 97 percent. You might say, “Well, for the for-profit school that has a pass rate of 84 percent, that’s not so bad.” You would be wrong. Only about 60 percent of the students at the for-profit Caribbean schools ever take the boards and, if they ever pass them, only about 50 percent get a residency in the match. Do the math: 60 percent take the boards, 19 percent to 84 percent pass the boards, and 50 percent get a residency in the match. 60% x 84% x 50%=25% and 60% x 19% x 50%=6%. In return for $200,000 to $400,000 in student loan debt, funded by U.S. federally supported student loans most of the time, the chance of these young people ever getting a residency is 6 percent to 25 percent. Why should we care about these for-profit schools? Because 90 percent of their students are borrowing money from U.S. federallysupported student loans. The Caribbean schools then pocket the money in tuition, and then they turn around and buy third- and fourth-year clinical rotations for their medical students at U.S. hospitals for $400 to $1,000 per student per week.4 U.S. medical students, including those at NYMC, are either threatened with losing—or are actually bumped out of—clinical rotations at hospitals by the Caribbean for-profit schools. The for-profit schools also dangle monetary offers and the opportunity of living for a few months on a Caribbean island to M.D.’s and Ph.D’s who are willing to teach at their schools. (While in Curaçao, I met a man who worked at one of the for-profit schools and asked if either I wanted a job or knew someone who did.) Physicians of my generation were taught that educating the next generation of physicians was an honor and a privilege. The Caribbean for-profit schools have monetized the system and turned it into a laissez-faire wild west. Texas recently enacted a law to end the imposition of the for-profit schools on medical education in Texas and federal legislation to tackle the problem has been introduced in the U.S. House of Representatives and Senate. At NYMC, we have confronted these challenges by defending our existing hospital relationships and aggressively expanding our affiliations with new hospitals. We have also actively partnered with other health sciences schools to seek legislative relief from the challenge. Most importantly, however, we have engaged in continuous quality-improvement in all of our academic programs to make seats in our College desirable while raising academic standards for admissions. In the middle of the 19th century, John Cardinal Newman taught that, “A University is … an Alma Mater, knowing her children one by one, not a foundry, or a mint, or a treadmill.”5 For-profit health science education is everything that Newman abhorred: a foundry, and mint, and a treadmill. The most important thing we can do in responding to this challenge is what we have always done: Ensure that the world knows the quality and value of a degree from NYMC.
Edward C. Halperin, m.d., m.a. chancellor and chief executive officer
References: 1. Weaver RM. Ideas have consequences. Chicago: University of Chicago Press, 1948. 2. H alperin EC, Perman JA, Wilson EA. Abraham Flexner of Kentucky, His Report, Medical Education in the United States and Canada, and the Historical Questions Raised By the Report. Academic Medicine 2010;85:203-210. 3. Hartocollis A. Second-chance med school. NY Times July 31, 2014. 4. L orin J. DeVry lures medical school rejects as taxpayers fund debt: Bloomberg business September 11, 2013. 5. Newman J. The idea of a university. Washington: Regnery Publishing, Inc., 1999.
C H I R O N I A N • New York Medical College
1
NEWS Briefs New Academic Affiliations Announced NEW YORK MEDICAL COLLEGE HAS ENTERED INTO ACADEMIC AFFILIATIONS WITH TWO NEW TEACHING SITES FOR ITS MEDICAL EDUCATION PROGRAM.
I
n November 2014, NYMC announced an agreement with Beckley Veterans Affairs Medical Center (Beckley VAMC) in Beckley, W. Va., designating Beckley VAMC as a teaching site for the purposes of enhancing education, research and patient care. NYMC has a longstanding relationship with the VA Hudson Valley Health Care System and is expanding its ties with the VA through this new affiliation. With Beckley VAMC as a partner, NYMC will be better able to provide outstanding clinical care and service to the community; incorporate the latest advances in medical knowledge into health care practices; and improve patient care at its clinical affiliates through advances in education and research. Beckley VAMC is a 40-bed general medical and surgical facility with a 50bed community living center. The medical center is a Joint Commission-accredited complexity level III rural access facility which provides inpatient and outpatient services to more than 14,700 Veterans in 11 counties in southern West Virginia.
In March 2015, NYMC announced an academic affiliation with Good Samaritan Regional Medical Center (GSRMC) in Suffern, N.Y., designating the hospital as a teaching site. The agreement outlines a mutual obligation to create and maintain a learning environment that promotes the highest standards of medical professionalism. NYMC and GSRMC will establish a clerkship program at the hospital for the training and education of NYMC’s undergraduate medical students on required and elective rotations in pediatrics, emergency medicine and critical care. NYMC and the hospital will cooperate to regularly evaluate and enhance the learning environment and to ensure professional standards and conduct are met. GSRMC is a non-profit, 286-bed hospital providing emergency, medical, surgical, obstetrical/ gynecological and acute care services to residents of Rockland and southern Orange counties in N.Y. and northern Bergen County, N.J. ■
“Meet the Doctor” Lecture Series Introduced
N
ew York Medical College partnered with the local Mount Pleasant Public Library to present a monthly “Meet the Doctor” lecture series. NYMC faculty members presented relevant topics in medicine and public health to the local community, followed by question and answer sessions. The first lectures covered the topics of Autism Spectrum Disorders; Speech, Language, and Feeding Milestones; Reversing Midlife Weight Gain; Baby Boomers and The Family Caregiving Gap; and Childhood Vaccines. ■
2
SUMMER/ FALL 2015
Master of Science in Medical Ethics Program Begins Fall 2015
B
eginning this fall, New York Medical College will offer a Master of Science in Medical Ethics. In keeping with the College’s mission of educating outstanding health care professionals for the multicultural world of the 21st century, the new master’s degree and certificate program will use historical, philosophical, legal and social-scientific approaches and models to address bioethical challenges. The program will provide students with rigorous methodological and substantive training and emphasize clinical medical ethics, compassionate care, religio-cultural competence, ethical implications pertaining to emerging technologies and the different notions of justice that influence ideas of public health. Classes will initially be offered in the evening and online. Students will study with a broad range of faculty, allowing them to
draw on the diverse expertise and resources that NYMC has to offer. Ira Bedzow, Ph.D., serves as director of the program. Dr. Bedzow has a Ph.D. in Religion from Emory University, a Master of Arts degree from University of Chicago, a Master of Arts degree from Touro’s Graduate School of Jewish Studies and a Bachelor of Arts degree from Princeton University. He is an ordained Orthodox rabbi and the Senior Scholar at the Aspen Center for Social Values. This program is targeted to medical students, health professional students and practicing health care providers who are interested in expanding their training in this area. The program is also of interest to rabbinical students who want to work in chaplaincy in a medical setting. ■
Ira Bedzow, Ph.D.
SHSP Launches New Programs
T
he School of Health Sciences and Practice (SHSP) is introducing two new programs: an accelerated Master of Public Health in Health Policy and Management and a Master of Science in Biostatistics. The new accelerated M.P.H. in Health Policy and Management began June 2015 and is designed to be completed in one year. The accelerated M.P.H. is offered on-campus and online over three consecutive semesters (summer, fall and spring). The 46-credit program is designed to complement the education of physicians and other health care practitioners by providing a deeper understanding of concepts and principles
of public health, community outreach and systems management. Graduates of the program will develop the skills needed to derive and implement solutions affecting health care from a policy, management and planning perspective and be able to deliver solutions to all areas of local, national or global health care settings. Starting fall 2015, the SHSP will also offer a new Master of Science in Biostatistics, a 36-credit program with an emphasis on health analytics designed to teach students to: • apply the principles of probability and inference to predict outcomes of health care models; • mine “big data” to inform the design and delivery of health care systems;
develops systems to maintain and improve health care outcomes. As the health care system evolves there is an increasing need for health analytics, the methodology that underlies the analysis and application of evidence-based research to assess health outcomes and to infer optimal health care delivery. Students will learn sophisticated techniques in biostatistics and gain an understanding of decisionmaking based on probability and risk. The program will give graduates the tools and techniques to build and analyze decisionmaking models for providers and insurers as well as business-related and communitybased initiatives. Students who pursue the program full-time will be poised to complete the degree in four semesters or may choose to pursue the program part-time. ■
• add value to a team that analyzes and
C H I R O N I A N • New York Medical College
3
NEWS Briefs 2015 Match Day is an Unequivocal Success different measures or outcomes that define the success of a medical school. New York Medical College’s success is clearly defined by the successes of our medical students. This Match proves it,” Gladys M. Ayala, M.D., M.P.H., vice chancellor of university student affairs, told the crowd. “Every year people ask me to sum up the Match. Was it successful? Is it the best? Believe it or not, I would absolutely say unequivocally this Match is outstanding. In fact, I would say this Match was the best.”
J
ust before noon on Friday, March 20, 2015, Match Day, the Medical Education Center was loud and boisterous as the School of Medicine Class of 2015 anxiously waited to find out where their residency training would be. “There are many
There were 202 NYMC students who matched this year, including five who matched in military programs, two who matched in the American Urological Association Urology Residency Match Program in January and three who matched in the San Francisco
Match in ophthalmology in January. The most popular specialty choices were internal medicine (21%), radiology (13%), pediatrics (11%) and anesthesiology (9%). More than 42 percent of the class chose programs in primary care—internal medicine, pediatrics, family medicine or ob/gyn. New York and California were the most popular states for residency training (35% and 15%) respectively, followed by Pennsylvania (8%), Connecticut (6%) and Maryland (6%). Graduates will go on to NYMC residency programs at Westchester Medical Center, Lenox Hill Hospital, Metropolitan Hospital Center, Norwalk Hospital, Greenwich Hospital, St. Joseph’s Healthcare System and Phelps Memorial Hospital Center. ■
Pre-Internship Program Graduates Celebrate at Completion Ceremony
C
ertificates of completion were presented to graduates of the Pre-Internship Program at a celebratory ceremony with families and friends on December 11, 2014, marking the completion of one year of supervised clinical training before moving on to residency training. The Pre-Internship Program began as the Fifth Pathway Program in 1974 and, since then, more than 2,700 students have successfully completed the training and gone on to practice medicine throughout the U.S. This year, 26 students trained at Richmond University Medical Center in Staten Island, N.Y., Saint Joseph’s Medical Center in Yonkers, N.Y., and Wyckoff Heights Medical Center in Brooklyn, N.Y. Lawrence Eisenstein, M.D., Fifth Pathway ’01, Nassau County Commissioner of Health, was the guest speaker and received the Distinguished Alumnus Award. Sophia Kathy Mendieta, M.D., PreInternship Program ’14, who completed her training at Richmond University Medical Center, received the Award for Academic Excellence for achieving the highest academic record, receiving honors in every
4
SUMMER/ FALL 2015
rotation. Saverio S. Bentivegna, M.D. ’50, who served as senior associate dean for the Pre-Internship Program, was recognized with a Certificate of Appreciation for his 40 years of service, mentorship and leadership, to the students of the Fifth Pathway and Pre-Internship programs. ■
NYMC Proudly Hosted U.S. Holocaust Memorial Museum Exhibit “ DEADLY MEDICINE, CREATING THE MASTER RACE,” A TRAVELING EXHIBIT FROM THE U.S. HOLOCAUST MEMORIAL MUSEUM, DREW MORE THAN 3,000 VISITORS TO NYMC’S CAMPUS.
D
isplayed at the Skyline Building from July 15 through September 3, 2014, the exhibit traces the history of the early 20th century international eugenics movement which culminated, most notably, in Nazi Germany’s establishment of a “science of race,” and its campaign to “cleanse” German society of the people deemed biologically threatening to the nation’s “health.”
Their Implications for Medical Ethics in the Midst of a War on Terror,” by Dr. Halperin. Dr. Kadish moderated a panel discussion with Sharon Halperin, director of the Holocaust Speakers Bureau; Dr. Mark Hasten, Holocaust survivor and chairman of the Board of Trustees; and Harry Reicher, professor at Touro Law School and an expert on the Holocaust and human rights.
More than 150 members of NYMC leadership, faculty, staff, students, government officials, as well as the local community, attended the exhibit’s opening, which featured docent-led tours.
Events also included book signings and discussions by Anthony J. Sciolino, who wrote The Holocaust, the Church, and the Law of Unintended Consequences, which explores Christianity’s involvement in widespread anti-Jewish sentiment and Steven Pressman, author of 50 Children: One Ordinary American Couple’s Extraordinary Rescue Mission into the Heart of Nazi Germany. Pressman discussed his true account of Gilbert and Eleanor Krauss, an American couple who traveled to Nazioccupied Austria in 1939 in an effort to transport a group of unaccompanied Jewish children to the U.S.
“This is a profoundly important collection that physicians, scientists, public health professionals, and everyone in the community should see,” Edward C. Halperin, M.D., M.A., chancellor and CEO, said of the show, which examines how Nazi leadership, in collaboration with physicians, medically-trained geneticists, psychiatrists, and anthropologists used their alleged science to rationalize the mass sterilization of “hereditarily diseased” persons leading to persecution, murder, and ultimately, genocide. In addition to Dr. Halperin, Alan Kadish, M.D., president, Kevin J. Plunkett, Westchester County deputy executive, and Michael J. Smith, Westchester County legislator, addressed the crowd. Numerous lectures and panel discussions accompanied the seven-week exhibit, including “Eugenics, the Holocaust, and
Although the exhibit spans a period in history that has passed, it calls attention to the current fascination with the human genome and genetic technologies, the latest means, some argue, of exploring notions of human perfection. Thus, in addition to portraying the ghastly misuse of medicine more than 70 years ago, the exhibit suggests that in the wrong hands, the healing power of medicine and science can be deadly. ■
C H I R O N I A N • New York Medical College
5
BREAKING BARRIERS
E
Founded in 1973 to address the “urban pipeline” dilemma, the Sophie Davis School of Biomedical Education encourages students who are underrepresented in the medical field—minorities and the economically disadvantaged—to study primary care fields in order to one day practice medicine in areas with a shortage of physicians. NYMC is one of six partner schools to welcome them.
to increase the number of primary care physicians—there is great alignment with NYMC, whose mission hasn’t deviated from maintaining a richly diverse student body and helping the underserved,” says Gladys M. Ayala, M.D., M.P.H., vice chancellor of university student affairs and senior associate dean for the School of Medicine. “That’s important not only for educational purposes—learning from others and building relationships—but also for producing outstanding physicians for today’s multicultural world.”
“If you look at the mission of the Sophie Davis School—to recruit students who are underrepresented in medicine and
At CUNY, Sophie Davis students do not follow a traditional
ach year, a select group of seven to nine driven students transfer into New York Medical College for their final two years of medical school from the City University of New York’s (CUNY) Sophie Davis School of Biomedical Education at the City College of New York campus in Manhattan.
6
SUMMER/ FALL 2015
undergraduate course of study, nor take the MCAT. Instead, they complete accelerated science courses followed by a multi-year unit in “community health and social medicine,” serving at clinics and community centers to provide care to patients.
Countering physician shortages in at-risk areas, NYMC partners with the City University of New York Sophie Davis School of Biomedical Education to broaden access to medicine by
Melissa F. Pheterson The way I see it, a humanistic approach to medicine is just good medicine. Great physicians listen to their patients (no matter what language is being spoken), advocate for their concerns, and create an environment that is conducive to healing, even when the prognosis is bleak. Know that, as a physician, you are seeing patients in their most vulnerable states; they are usually ill, uncomfortable, and unfamiliar in their surroundings. Don’t forget how impactful a smile, eye contact, a comforting touch, or time taken to listen and answer questions can be. Always remember that your patient is someone’s mother/father, sister/brother, partner or best friend. Linda Alvarez, M.D. ’15, a Sophie Davis Student
HOLISTIC APPROACH “In low-income areas you can see the broad spectrum of care, including the barriers,” says Patrice Pryce, M.D. ’15, of her experience at the Ryan/Chelsea-Clinton Community Health Center in Manhattan. “It’s not only treating the patient clinically, applying what we’ve learned in textbooks; it’s making sure the patient is socially, financially, and emotionally prepared to receive and access the care.” Harry Lee, M.D. ’90, was a Sophie Davis student who graduated from New York Medical College. Today, he is an ob/ gyn attending physician at Mount Sinai Roosevelt Hospital and Mount Sinai St. Luke’s Hospital in Manhattan. “In high school, I was idealistic about putting in work in underserved areas,” says Dr. Lee. “I didn’t really know what it
entailed.” But as a Sophie Davis student, he cared for the homeless who lived in single room occupancy housing in the Chelsea neighborhood of Manhattan. “It made me realize these groups of people are disadvantaged and really do need health care; they need us.” Dr. Lee’s practice includes coverage at city clinics, reflecting the Sophie Davis and NYMC emphases on “building your career with an awareness of the underserved, as opposed to excluding them.”
“In certain situations, patients are more apt to open up or ask difficult questions when I come into the room,” says Pryce, who is Caribbean-American. “Seeing me puts them at ease.” Dr. Ayala agrees that sharing a native tongue or ethnic background can support the doctor-patient relationship in delivering quality care. “Disparities and barriers often stem from patients’ fear, so having doctors that are culturally similar to their patients does
EMPHASIZING ETHOS
help to bring down those barriers,” says
With today’s emphasis on cultural humility in understanding and respecting a patient’s traditions and health care beliefs, there is a benefit to training physicians who are deeply versed in a patient’s culture.
Dr. Ayala. “It would be naïve to say only physicians who come from underserved areas are prepared to serve there, but there’s no doubt patients get a sense that, ‘here is a person who can understand me.’” ■ C H I R O N I A N • New York Medical College
7
GREEN REVOLUTION SWEEPS NEW YORK MEDICAL COLLEGE By Andrea Kott, M.P.H.
DAY BY DAY, NYMC’S CARBON FOOTPRINT IS GETTING SMALLER. In fact, for the past several years, the College has been going green: stepping up efforts to promote sustainability and environmental protection. Sarah Cottet, director of Environmental Health and Safety, says the efforts were ramped up significantly with the renovation of 7 Dana Road—home of NYMC’s Clinical Skills and Disaster Medicine Training Center and BioInc@NYMC—to qualify for LEED (Leadership in Energy and Environmental Design) certification at the “gold” level. LEED is a certification program that recognizes green building strategies and practices with silver, gold or platinum honors. Its certification standards apply to energy use, water efficiency and indoor air quality. Today, the newly-renovated building—built with responsiblyharvested wood and recycled materials—is a model of environmental stewardship. Its paint, toilets, adhesives and tiles have either no amount, or trace amounts, of volatile organic compounds which emit noxious vapors, meaning the building’s indoor air should be free of respiratory irritants. Additionally, all cleaning products are non-toxic, and HEPA filter vacuums are used in the building. The facility’s plumbing fixtures feature water-conserving technology. The building also uses low-mercury, high-efficiency lighting, energy-efficient appliances and recycling stations. “This is our showcase project, demonstrating how we would like to build across campus going forward,” says Cottet, who is currently working on decreasing the energy usage of existing laboratories on campus, utilizing information from energy studies
8
SUMMER/ FALL 2015
funded by the New York State Energy Research and Development Authority.
SUSTAINABILITY Another force in NYMC’s green revolution has been a campus sustainability program, “GreenNYMC,” which began as a joint capstone project among the students of Michael Shakarjian, Ph.D., assistant professor of environmental health sciences and director of M.P.H. studies; Anna-Marie Vetrano, Ph.D., assistant professor of environmental health sciences; and Denise C. Tahara, M.B.A., M.Phil., Ph.D., associate professor of public health practice and interim chair of the Department of Health Policy and Management. Launched in the spring of 2014, the project aimed to improve the College’s recycling practices and create multiple composting sites on the College campus. It began with an environmental assessment study, which Dr. Shakarjian’s and Dr. Vetrano’s students conducted to determine where to best locate and how to maintain a compost pile. They also produced educational and training materials as well as signage for composting sites and recycling bins around campus. Dr. Tahara’s students, meanwhile, wrote a business plan that featured a cost analysis for creating and maintaining the composting site and
improving recycling practices campus-wide. In preparing the plan, they reviewed NYMC’s sustainability procedures, as well as recycling, composting, education and training best practices at institutions around the country. Their research revealed seven common elements in the most successful sustainability programs: program logo, collaboration, single stream recycling, prominent signage and guidelines, education and training, sustainability coordinator, and tracking and metrics. At the completion of the capstone project, several students co-authored a paper, Sustainability: On the Road to a Green NYMC, which a journal is currently reviewing. The capstone project paved the way for NYMC’s current sustainability efforts, now under the direction of Elizabeth Monahan, project coordinator for the Department of Environmental Health and Safety. Monahan mobilized a composting and sustainability committee, whose members include second-year medical student Peter Spyrou; third-year medical students Zaza Atanelov, Erin Byrt and Jessica Oh; recent SHSP graduate Jillian Annunziata, M.P.H. ’15, and M.P.H. student Drew Lidster. The committee has been educating the NYMC community about general composting recommendations; for example, discouraging the inclusion of bones, meat, dairy and oils, whose decay produces too much odor. It has also distributed more than 25 bins to students and faculty and strategically placed six 35-gallon tubs around campus—three in student housing areas, two outside of the cafeteria, and one between the School of Health Sciences and Practice building and the Medical Education Center. The committee ensures that composted materials contain the proper blend of carbon, nitrogen and moisture, so that everything reacts correctly. “It is important to remember the 1-part-green to 3-parts-brown ratio when adding to the composting bins,” Monahan explains. “When you add your
veggie scraps (green), you also have to add leaves, paper shreds, or woodchips (brown) to balance the chemical reaction.” Composting underscores how much food goes to waste, while converting this unwanted food into soil for the student garden and as mulch for fertilizer on campus. “We have had huge success already,” says Monahan, who credits dedicated student involvement, in addition to the supportive cafeteria staff and facilities department for providing composting bins and diverting ample food waste to them. She and the team are now exploring other methods for increasing composting participation throughout the NYMC campus, and possibly partnering with Westchester County in the coming years for increased support.
GOING GREENER Other ongoing green initiatives on campus include turning off the lights in rooms when not in use; making dual-sided copying the default setting on all college copiers and printers; promoting the electronic transmission of all documents; recycling used batteries and car sharing through Zipcar. Additionally, NYMC publications, including Chironian, are now produced with recycled paper and soy inks, and are certified by the Forest Stewardship Council. Dr. Tahara says she requires all students to print double-sided papers and submit them online. Plus, she only allows reusable water bottles in her classroom. “We are training the next generation of health care leaders and it’s incumbent on us to practice what we preach. It’s got to be at the front of everybody’s mind.” ■
“We are training the next generation of health care leaders and it’s incumbent on us to practice what we preach. It’s got to be at the front of everybody’s mind.” Denise C. Tahara, M.B.A., M.Phil., Ph.D., associate professor of public health practice and interim chair of the Department of Health Policy and Management
C H I R O N I A N • New York Medical College
9
STRIKING GOLD in the “Sandbox” of Science
10
SUMMER/ FALL 2015
On-campus incubator — BioInc@NYMC — unites biotech research with academic resource to stoke growth, enterprise and innovation B M F. P y
elissa
heterson
It wasn’t just business as usual. It was something better.
beyond the typical reach of a start-up venture.”
In the last days of October 2014, a new facility officially opened its doors at New York Medical College—not just with turnkey office suites and modern laboratory space, but with a new prototype of enterprise for the campus and region. Its name: BioInc@NYMC. Its claim to fame: the Hudson Valley’s only biotechnology incubator located on a health science college campus.
The result: a platform for innovation, breakthrough and synergy among entrepreneurs whose discoveries have the potential to save lives, promote health and improve quality of life for millions.
As an “incubator,” BioInc@NYMC attracts entrepreneurs and start-ups within the region’s growing biotechnology sector that seek the critical resources to pursue promising research, develop life-saving medical devices, and thrive as full-fledged companies advancing life science. The firms who have moved in enjoy not only state-of-the-art equipment and workforce training suites; they also have ready access to facilities on campus and the chance to collaborate with the College’s researchers, academics and thought leaders. “There are many ways to get a sink or a hood when you have a new idea,” says Robert W. Amler, M.D., M.B.A., vice president for government affairs and dean of the School of Health Sciences and Practice. “But it is very difficult to access a deep bench of advisors and colleagues with whom you can have a free-exchange on a medical school campus. Having a biotechnology incubator on our health sciences campus gives you that free exchange, along with facilities that are
IT TAKES A VILLAGE BioInc@NYMC is a public-private venture, combining resources from the federal government, New York State, Westchester County and NYMC. Approved as a taxfree zone from the business development initiative called START-UP NY, the incubator has also received the multi-year Mid-Hudson Innovation Hot Spot award granted by the New York State Regional Economic Development Council (REDC), designed to foster innovation by offering business support services to start-ups and by promoting collaboration between enterprise and academia. According to Amler, these state awards position the incubator at the heart of the Hudson Valley’s growing “biotech corridor.” “Through START-UP NY, we are linking the talent base and experience of our faculty with the energy and innovative spirit of the private sector,” Amler says. “Partnership between academic and commercial enterprise is vital for developing new biomedical research advances that rapidly translate into improvements in public health and patient care. The new biotech incubator was designed to do exactly that; to create a
C H I R O N I A N • New York Medical College
11
space where university researchers and a community of scientists can collaborate to fuel the next generation of biomedical advances,” said President Alan Kadish, M.D. “Grant support from New York State and the presence of the START-UP NY program at New York Medical College are integral to growing this program into a successful and sustainable venture.” While serving on the REDC, Dr. Marsha Gordon, CEO of the Business Council of Westchester, helped Governor Andrew Cuomo identify 80 companies in the Hudson Valley related to biotech to help secure $5 million in funding for BioInc@NYMC. “Biotech is growing fast and we are fortunate to have New York Medical College’s interest in developing a biotech incubator,” she says. “This is a segment of the economy that we want to grow and prosper here.” Randi D. Schwartz, M.B.A., interim director of BioInc@NYMC and associate dean for academic administration at New York Medical College, has noticed thriving synergies between the building’s resident licensees and College faculty since the incubator opened for business. “Collaboration with our public health and science clinicians, entries into clinical trials, working with clinicians at our affiliate hospitals—those are all in the works to be developed further,” she says. Faculty and students derive momentum from the entrepreneurs as well—especially as funding from sources like the National
Institutes of Health becomes harder to obtain. “Partnering with entrepreneurs is a way for our own clinicians and faculty to pursue new opportunities, generate sources of revenue and foster growth,” says Schwartz. “It will help students too; our graduates have ideas to develop and are interested in space at the incubator, which bodes well for our School of Health Sciences and Practice.”
ONE STOP SHOP Sarah Cottet, director of Environmental Health and Safety for the College, welcomes her new role as the incubator’s director of laboratory operations. Cottet has been involved in BioInc@NYMC from the drawing board, working with architects to develop the office suites and shared laboratory space. “We thought about what a biotech incubator should provide to support its occupants, and provided the capital equipment that’s necessary to early-stage research,” she says. That means CO2 incubators, shakers, freezer space, fume hoods and centrifuges. Floor-toceiling windows in most lab spaces and clean, bright finishes make for “a facility characterized by its openness and light.”
“Having core services and collaborative faculty on staff is a major selling point,” she says. “Because I come from a research background, pairing licensees with services at the College is a nice way for me to return to where I started. In that way, BioInc is my little nest egg. I feel energized by the creativity.” And she says the additional amenities— equipment, security, access to the Health Sciences Library, plus a cafeteria and bookstore in the Basic Sciences Building— render the leases “far more than just a real estate deal.” “The hope is for our licensees to outgrow the space in one year to five years,” she says, “when they license the technology to a larger company. We’re more of a nursery. We get companies on their feet.”
STARTING UP
One such company is MOE Medical Devices, whose founder Marc Zemel chose BioInc@NYMC when his company outgrew its first “office”—his basement. In their new space on campus, he and his two partners harness advances in optics and electrical plasma to develop targeted therapies for maladies from cancer cells to toenail In her frequent visits, Cottet arranges for entrepreneurs to partake in the core services fungus. the College makes available in its Basic “We’ve got electrical testing, building Sciences Building—including a vivarium, device technology and biochemical high-containment lab, bioimaging services, facilities, all at our disposal,” he says. molecular modeling and mass spectrometry. Cottet says she also plays “matchmaker” by That means his team can build electrodes pairing the start-ups with possible resources and generate electrical plasma to kill fungi on NYMC’s faculty and staff. and other microbes, continuing the pre-
“ Through START-UP NY, we are linking the talent base and experience of our faculty with the energy and innovative spirit of the private sector. ” ROBERT W. AMLER, M.D., M.B.A., vice president for government affairs and dean of the School of Health Sciences and Practice
12
SUMMER/ FALL 2015
“Partnership between academic and commercial enterprise is vital for developing new biomedical research advances that rapidly translate into improvements in public health and patient care. The new biotech incubator was designed to do exactly that; to create a space where university researchers and a community of scientists can collaborate to fuel the next generation of biomedical advances.” President ALAN KADISH, M.D. clinical and clinical research that has already attracted millions of dollars in funding.”
for the region’s biotech sector, including the cluster known as BioHud Valley.
“I’ve learned that, like raising a child, starting a company takes a village, too,” Zemel says. “Here, we’re surrounded by talented individuals with novel ideas and vast resources. That proximity to research, people and ideas is great. The College has created the supportive, collaborative ecosystem we need to get this company off the ground.”
“The two main goals of our mission are job creation and economic development for Westchester and the lower Hudson Valley,” Schwartz says. “We’ve been fortunate to get interest from people who live in the region but might work in New York City; we have the bucolic setting with ample parking, and we’re close to home.”
Down the hall, the biotech firm Conversion Energy Enterprises (CEE) sources material from corium to make a soluble collagen that, when exposed to laser light, acts as a glue to join tissue. Having shown promise in coating a hernia repair mesh and in killing bacteria, the technology continues to evolve under the roof of the incubator. “This space had all the basics we were looking for in terms of location, wet lab facility, and potential for collaboration,” says Bob Soltz, vice president of engineering at CEE. “We’ve felt quite welcome. We see a strong synergism with our technology.” Soltz and his wife Barbara, the company’s CEO, have their own centrifuges, sinks, and racks for drying test tubes as well as chemical hoods, powerful freezers and distilled water provided by the facility in the common spaces. The Soltzes are discussing partnerships with researchers at the College’s vivarium, among other departments. In addition to supporting its licensees, BioInc@NYMC has received federal funding to become a training and resource center
Marissa Brett, president of the Westchester County Association and executive director of the BLUEPRINT for Westchester, characterizes BioInc@NYMC as a “tremendous asset” in stimulating the local “innovation economy” of biotech companies in the critical incubation stage.
Corporation, joined the College in efforts to secure state funding. Building on the metaphor of the “incubator,” he likens the space to both a “sandbox” and a “nurturing ground” for companies to play, fail (if necessary), dust themselves off, and grow to maturity in Westchester’s fertile soil. And the synergy radiating from that sandbox, yoking business enterprise with academic research, is also poised to bring about a healthier—and happier—world. ■
As Dean Amler puts it, the incubator is “the right project at the right time at the right place.” “It’s the right project because it draws from the intrinsic talent base of our highly educated population, and it’s poised to be a game changer that opens up new markets,” he says. “It’s the right time because New York Medical College is on the upswing with new facilities, new academic programs and new, talented leadership structures. And it’s the right place because it’s close to New York City but enjoys lower cost structures; and we’re part of the Touro College and University System with a broad geographic base,” including a presence in San Francisco’s Silicon Valley. Larry Gottlieb, president and CEO of the Hudson Valley Economic Development C H I R O N I A N • New York Medical College
13
FAMILY MATTERS NYMC’s family medicine residency programs are taking the lead in meeting the critical need for family physicians By Robert S. Benchley You might say that London Muse, M.D. ’12, chief resident in the NYMC Phelps Family Medicine Residency Program, was born to be a family physician, because the theme of birth has been a constant from her childhood through this early stage of her medical career. The product of a close-knit Iowa family, she decided to become a doctor at age 12 after being present when her younger sister was born. As the first chief resident, and a member of the first class to go through Phelps, she has truly helped give birth to the program. And her interview for this article had to be rescheduled because she was busy … delivering a baby. But despite what many would consider a symbolic perfect fit, Muse says specializing in ob/gyn just felt too limiting. “I chose family medicine so I could do everything,” she says. “I volunteered in the local E.R. while I was an undergraduate at the University of Notre Dame, and also at my hometown hospital back in Des Moines during college summers. I saw how many different ways one could make a difference in people’s lives.” Phelps is the newest of the four family medicine residency programs in New York Medical College’s Department of Family 14
SUMMER/ FALL 2015
and Community Medicine (see sidebar). When it received accreditation in 2011, it became the first new family medicine program in New York State since 1995. Located in the suburban Westchester County village of Sleepy Hollow, it is a partnership with Phelps Memorial Hospital Center, a 238-bed teaching hospital, and the Open Door Family Medical Centers, a federally-qualified community health center with several locations that provides a broad spectrum of care regardless of a patient’s ability to pay.
MODEL FOR THE FUTURE “The Phelps program is unusual because it is a collaboration between a hospital and a community-based family medical center,” says Richard G. McCarrick, M.D., vice dean for graduate medical education in the School of Medicine. “For the residents, the hospital provides in-patient experience; Open Door provides experience with ambulatory patients. It’s a model for the future. “Family medicine is the broadest of all medical specialties,” he adds. “It’s very challenging to stay current in so many different areas of medicine. The diversity of metropolitan New York increases the complexity. As a physician, you treat people from all over the world, so in addition to clinical skills, you also have to have cultural competency.”
For Muse, that included learning Spanish, which she did not speak when she arrived. “We have a large Spanish-speaking population,” she says, “mostly from the Dominican Republic and Ecuador. Now I speak Spanish 75 to 80 percent of the time with outpatients, 50 percent with inpatients.” Muse has the independent, can-do attitude that NYMC faculty looked for when selecting the first group of family medicine residents for Phelps. “The first class had a real esprit de corps from the beginning— they had to,” says Shantie Harkisoon, M.D., assistant professor of family and community medicine and program director of the Phelps residency program. “They were instrumental in making the program what it is. Not just the rotations, but meeting people, fundraising and teaching the community what family medicine is—and they were in it alone; they didn’t have senior residents to guide them.” “We realized pretty quickly that we were all go-getters, problem-solvers and decision-makers,” says Muse. “We worked mostly with attending physicians, and with each other, and we had to grow up fast.” lthough the first-year residents had to provide some of their A own support, there were benefits to launching a brand-new residency program. “ We have been able to spend a lot of time innovating and partnering with people in the community to develop a curriculum geared toward training doctors for the future,” says Harkisoon.
A TEAM APPROACH Much of the focus has been on training the residents for practicing in a “patient-centered medical home” environment—a team-based approach that is intended to make primary care more accessible, comprehensive and coordinated in order to improve patient outcomes while lowering overall health care costs. “Under this model, the whole team is responsible for the patient’s outcome,” says Harkisoon. “Everybody shares ideas
“ Family medicine is the broadest of all medical specialties. It’s very challenging to stay current in so many different areas of medicine.” Richard G. McCarrick, M.D., vice dean for graduate medical education
ALL IN THE FAMILY New York Medical College’s other family medicine residency programs—one in Westchester and two in New Jersey—are part of a proud tradition of physician training dating back more than 40 years. Each is different and special in its own way. SAINT JOSEPH’S MEDICAL CENTER, YONKERS, N.Y. New York Medical College’s oldest family medicine residency program, founded in 1974, is at Saint Joseph’s Medical Center in Yonkers, a 532-bed general medical and surgical community hospital. It is also the largest program, with 30 residents directed by Sonia A. Velez, M.D., J.D. “We are the only residency program within this hospital,” she says. “As such, our residents are the first responders to all clinical situations, admissions and codes, and they are first assists when on surgical rotations. They become proficient with intubations and line placements, among other procedures, and they cover the I.C.U. and intermediate care units throughout their second-year night float rotations, which provides them with extensive clinical experience.”
ST. JOSEPH’S REGIONAL MEDICAL CENTER, PATERSON, N.J. The program at 700-bed St. Joseph’s Regional Medical Center in Paterson, is NYMC’s second youngest, having begun in 2004, and smallest, with 12 residents. Michael Delisi, M.D., who is also chairman of family medicine for the St. Joseph’s Healthcare System, is its director. “We’re the only major medical center in the program, and we have more than 200 other trainees present,” he says. “We also probably have the most diverse patient population. Prior to the Affordable Care Act, about 30 percent were charity-care patients, and another 30 to 35 percent are Medicaid patients. People talk about doing medical rotations outside the United States, but here the experience comes to you—malaria, T.B. and other medical problems not seen in much of the U.S. are common here. It is also common for patients, often from other countries, to arrive with advanced states of disease. It’s a small residency within a very large medical center that offers the opportunity to see complex challenges on a continuous basis.”
HOBOKEN UNIVERSITY MEDICAL CENTER, HOBOKEN, N.J. The program at Hoboken University Medical Center, a 333-bed hospital, dates back to 1991, and became affiliated with NYMC in 2010. Hoboken is a very diverse two-square-mile urban community, says program director Abbie Jacobs, M.D., who supervises 24 family medicine residents. “Our biggest patient segment is Hudson County’s Hispanic population,” she says. “We also serve a large group of young urban professionals, and many of our patients are immigrants. We’re very much a part of the community—we act as the team physicians for the local school system— and we’re the only program with a sports medicine fellowship. We’re also excited about offering new behavioral health and therapy services.”
C H I R O N I A N • New York Medical College
15
and focuses on delivering extraordinary care. We train our residents to be both partners and team leaders when they go out and practice in the community. Our hope, of course, is that the community will be here in Westchester.” “Medical schools and hospitals share that hope—that graduates will be a pipeline to their own faculty and medical staff, and will be a source of referrals if they settle in the area,” says McCarrick. It’s more than a hope; it’s a real need. There is a nationwide shortage of family physicians, in large measure because a previous generation of medical school graduates saw greater appeal in other specialties. The result: the average age of family physicians in the U.S. is 48, and nearly 20 percent of those in practice are over 60, with retirement looming. New York Medical College, with four family medicine residency programs, is doing more than its share to refill the practice pipeline.
“ We have 86 family medical residents in our programs— more than any other medical school in the state.” Montgomery B. Douglas, M.D., associate professor and chair of the Department of Family and Community Medicine
AGGRESSIVE GROWTH STRATEGY “We have 86 family medicine residents in our programs—more than any other medical school in the state,” says Montgomery B. Douglas, M.D., associate professor and chair of the Department of Family and Community Medicine. “We have been quite aggressive in seeking to grow the department. Our strategy, as well as our mission, is to provide more family physicians for the downstate area. The easiest way to do that is to have programs you can promote from.” “The need is real,” he says. Although metropolitan New York City is the nation’s largest family medicine training area, with 11 medical schools and 15 family medicine residency programs, New York State as a whole loses more than 50 percent of its graduates to other states, primarily for financial reasons. “I founded the Downstate Family Medicine Consortium of all 15 programs and the six medical school Departments of Family Medicine,” says Douglas. “We have conferences and programs, and we talk about how we can keep our graduates here. When we are screening applicants, we often look for those who already have ties to the area.” The strategy seems to be working across all four family medicine programs. Of the pioneers—the six Phelps third-years—two are joining the NYMC Phelps residency faculty, one will stay at Phelps, one is joining Open Door as a provider, one is entering an ob/gyn fellowship, and one will likely be working at the local VA medical center. Muse has felt destined to teach medicine. “I’ve been teaching my whole life,” she says. “I tutored in high school, college and medical school. As chief resident, I’ve been working with the other residents, in groups and one-on-one. Now I want to teach residents and medical students.” ut she still plans to care for patients, whether it’s delivering B babies or whatever else they may need. “The great thing about family medicine is we teach our patients, and they teach us,” she says. ■
16
SUMMER/ FALL 2015
FIGHTING BIOTERRORISM IN THE LABORATORY Dozens of industrial chemicals are deadly to humans, have no antidote and could be potent weapons of terror. Michael Shakarjian, Ph.D., and his research team are focused on one already in misuse on the other side of the world. By Robert S. Benchley If you wish to harm other people, there are many ways to do it. Any number of industrial chemicals, introduced into the water supply or distributed through some other method that causes mass exposure, could become a potent weapon of terror. They can be highly toxic to humans, typically have no antidote and are cheap and easy to obtain. The exposure, however, doesn’t have to be deliberate. A freight train accident that causes the contents of a tanker car to be released into the nearby environment or a weather event that compromises a storage facility could have a similar impact. According to the Environmental Protection Agency, approximately 10,000 children in the U.S. suffer accidental exposure to mouse and rat baits each year, and one percent of them require medical attention. That’s 100 kids—a small-sounding number unless one of them is a loved one. Together with his research team, Michael Shakarjian, Ph.D., assistant professor of environmental health science and director of the M.P.H. program, is attempting to find an antidote to one of the most deadly of those rodenticides—tetramethylenedisulfotetramine (known commonly as TMDT or tetramine). TMDT is a neurotoxic agent that can cause seizures, permanent brain injury or death in humans, and its use is illegal in the U.S. and most western nations, but widespread in Africa. Nonetheless, it is on the U.S. government’s list of chemicals that could be used intentionally by terrorists. In fact, small-scale deliberate
C H I R O N I A N • New York Medical College
17
poisonings using TMDT have already happened in other parts of the world, such as China, where it is also illegal. Funded by a two-year, $805,000 grant from the National Institutes of Health’s CounterACT (Countermeasures Against Chemical Threats) program, the investigators are working to learn more about the toxic effects of TMDT. For Shakarjian, whose principal research interests include developing countermeasures against dermatological and neurological poisons, and who has a strong concern for how environmental factors can have a negative impact on human health, the TMDT grant is a perfect fit.
A SYSTEMATIC APPROACH “We are systematically examining a series of commerciallyavailable prescription medicines for their ability to treat seizures produced by TMDT,” says Shakarjian. “This work is novel because no one has taken a systematic approach to finding TMDT countermeasures before. “We are looking at combinations of drugs too. One standard treatment for seizures is the drug diazepam, better known as Valium. The way TMDT works, however, is that the longer the seizures have lasted, the more resistant the patient can be to Valium treatment. We are exploring other agents used in combination with Valium to see if we can achieve a better result.” Shakarjian and his team, in fact, just published an article in the May 2015 issue of the journal NeuroToxicology, in which they described how the use of diazepam with another drug, dizocilpine, reduced seizures and improved overall outcome. CounterACT supports basic, translational and clinical research aimed at the discovery or identification of better therapeutic medical countermeasures and/or diagnostic technologies against chemical threat agents. The results of successful investigations are then fast-tracked through the federal drug development and regulatory processes. Special consideration is given to research relevant to people who are particularly vulnerable, including pregnant women, infants, children, senior citizens and individuals with pre-existing medical conditions. Toxic chemicals in the hands of terrorists don’t discriminate unless a specific group is targeted. To date, all recorded TMDT exposures in the U.S. have been accidental. The deadly rodenticide has been used in China to mark a school or business as unsafe, and one of Shakarjian’s team members, Shabir Ferdows, a graduate student pursuing a master’s degree in epidemiology and infectious diseases, has seen chemicals like it used by the Taliban in his home country of Afghanistan to force the closing of schools. 18
SUMMER/ FALL 2015
“In Afghanistan, science was often taken out of education,” says Ferdows, who worked as a translator for the American military before coming to the U.S.; he earned an undergraduate degree at Cornell prior to entering NYMC. “Being here and having the opportunity to pursue science is a true blessing. If I can help school children anywhere in the world through my research, I will be very grateful.”
UNRAVELING THE MYSTERIES Another member of Shakarjian’s international team, post-doctoral fellow Marcela Laukova, Ph.D., who received her master’s and doctoral degrees in her native Slovakia, enjoys the challenging goal of being one of the first researchers to understand how TMDT works. But, she observes, two years is a short time to try to unravel all of its mysteries. “This compound is very dangerous to human beings,” she says. “It is water-soluble and has no taste or odor, so it poses a real threat for mass poisoning. That means we need the most effective countermeasure. Once we learn the mechanism of how it works, we can develop an appropriate treatment option to save people who have been exposed.” Also closely involved with Shakarjian’s project are Libor Velisek, M.D., Ph.D.; Jana Veliskova, M.D., Ph.D.; and Patric Stanton, Ph.D., neuroscientists and seizure experts from the Department of Cell Biology and Anatomy. “The ability to assemble a team such as this,” says Shakarjian, “is a great example of the excellent collaborative environment on our campus.” Shakarjian was recruited to New York Medical College by Diane Heck, Ph.D., professor and chair of the Department of Environmental Science in the School of Health Sciences and Practice. Heck’s research interests are focused on understanding mechanisms of inflammation and toxicity mediating chemicalinduced injury, wound healing and carcinogenesis. Her current projects involve developing countermeasures, treatments and therapeutics to address the effects of chemical toxicants and agents of mass destruction on civilian populations. Heck and Shakarjian met at Rutgers University in New Jersey, which houses one of the four CounterACT centers of excellence worldwide, and where Shakarjian conducted research under one of Heck’s grants. After he followed her to NYMC, Heck, who remains director of drug development and pharmacology at the Rutgers center, encouraged Shakarjian to apply for his own CounterACT grant.
“ Toxic industrial chemicals travel by us in trains, cars and trucks; they’re everywhere. Many people who are exposed are unaware of the potential threat to them. Having a way to address that threat is of extraordinary importance.” Diane E. Heck, Ph.D.
“Michael has moved into non-traditional counterterrorism— industrial chemicals, which can be incredibly dangerous if misused,” she says. “Toxic industrial chemicals travel by us in train cars and trucks; they’re everywhere. Many people who are exposed are unaware of the potential threat to them. Having a way to address that threat is of extraordinary importance. “If we have no way of intervening or mitigating injury, it’s a serious problem. Chlorine gas is an excellent example. We use it to purify water, yet it is deadly to humans, and we don’t have anything to counteract it. The TMDT that Michael is studying is on Homeland Security’s list of agents of concern because of its potential for misuse. It doesn’t take a lot of expertise or effort. It’s too easy to use not to be investigated.”
A RESEARCH STRATEGY Robert W. Amler, M.D., M.B.A., dean of the School of Health Sciences and Practice and vice president for government affairs, says it’s no accident that scholars with Heck’s and Shakarjian’s research interests are joining the College’s faculty. In fact, having the College become a go-to institution for biomedical research related to counterterrorism is one of his strategic goals. “The work they do is critically important, not only in the community in which we live but also for the nation as a whole,” says Amler, whose extensive federal emergency preparedness background includes a stint as chief medical officer at the Centers for Disease Control’s Agency for Toxic Substances and Disease Registry, where he coordinated medical monitoring for anthrax response teams and launched a nationwide program to protect children from chemical hazards. “Since the dawn of the 20th century, some 80,000 new chemicals have been discovered or invented. Some, of course, have been fantastically helpful, some are fantastically dangerous and some can be a little of each
depending on the dose or quantity. For many, the full range of health effects is not yet completely understood. “The work of researchers like Dr. Shakarjian contributes giant steps toward better understanding, safer use and safer disposal of these types of agents. In particular, when very noxious substances get into the wrong hands, we need to be ready with a safe and effective countermeasure.” Amler cites the related work of the College’s Center for Disaster Medicine, which opened in 2005, and which conducts interdisciplinary research, training, technical assistance and educational activities related to emergency preparedness for disasters, terrorism and public health emergencies. In addition, NYMC’s M.P.H. program includes a graduate certificate program in emergency preparedness—one of the first in the U.S. and available on campus or online.
NEXT STEPS Shakarjian says that promising results would prompt larger follow-up studies. Also, he notes, childhood seizures and treatments differ from adult seizures and treatments, so some of the research is focused on determining whether any of the antidotes are age-related. “My father was a pharmacist, and that’s how I got exposed to the health sciences field,” he says. “I was fascinated by how drugs work, and that led me to pharmacology. I never thought, however, that I would study a rat poison so that I could help prevent human beings from deliberately poisoning one another. But that’s what I’m doing now, and it’s important that we have antidotes that will successfully treat exposure to toxic chemicals, whether deliberate or accidental. If we can develop an antidote for TMDT, I will feel that my fellow researchers and I have made a valuable contribution to mankind.” ■
C H I R O N I A N • New York Medical College
19
D. Douglas Miller, M.D., C.M., M.B.A. Internationally-Renowned Cardiologist, Clinician-Scientist and Leader in Academic Medicine Takes the Helm as NYMC’s Dean of the School of Medicine
20
SUMMER/ FALL 2015
Dean Miller arrived in late 2014 to guide the School of Medicine beyond transition and through re-accreditation. Having been dean of two medical schools in two different countries, he is now poised to lead the School into a new era. By Melissa F. Pheterson Though a distinguished title, the word “dean” rarely becomes an action verb. But D. Douglas Miller, M.D., C.M., M.B.A., dean of the School of Medicine at New York Medical College, considers “deaning” the mission that animates his job: sustaining achievements among faculty, honing the vision of the School of Medicine, and ensuring that students take full advantage of technological breakthroughs while staying attuned to the human side of medicine and constant fluctuations in the business side of health care. “Coming to New York Medical College was an opportunity to accept the challenge of moving the organization forward, and apply my skills to navigating transition,” Dean Miller says. “I am using the prerogative of a ‘New Dean’ to look at everything afresh, re-examining our strategic plan and the ways it can drive strategic investment.” As the School of Medicine delves into a comprehensive self-study to prepare for its re-accreditation by the Liaison Committee on Medical Education (LCME) next year, other leaders are tapping into that energy. “Dr. Miller has been exceptional in rekindling excitement in each senior leader,” says Jennifer L. Koestler, M.D., senior associate dean for medical education.
TWO COUNTRIES, MANY INTERESTS A native of Canada, Dean Miller received his medical degree from McGill University in Montreal. As a resident and fellow, he pursued clinical cardiology and cardiology research in Montreal, and later, at Emory and Harvard Universities. In 1986, he joined the faculty of University of Texas Health Sciences Center in San Antonio, and then moved on to Saint Louis University. While teaching and chairing its Department of Internal Medicine, he completed an executive M.B.A. at the John Cook SLU School of Business and Administration, driven by an interest in health care and the business of medicine. “I was always a well-mentored academic clinician and scientist,” he says. “I was fortunate to benefit from a remarkable string of leaders who always encouraged me to do more with my time and energy—to advance the field of cardiology and to pursue my other career interests.”
From Saint Louis, Dean Miller joined the Medical College of Georgia (MCG) as dean of its School of Medicine in 2006. In 2010 he was appointed the Robert G. Petersdorf Scholar-in-Residence at the Association of American Medical Colleges (AAMC) in Washington, D.C., where he explored associations among national economies, health care policies and the physician workforce. John E. Prescott, M.D., AAMC’s chief academic officer, recalls the “sophisticated analysis and interdisciplinary focus” that Dean Miller brought to bear on the research, enhanced with the “unique international perspective” that comes from fluency in two different national health systems. “I have always been struck by his incredible dedication as an academic leader—an individual that wants to have an impact not as an ego thing, but because it’s the right thing to do,” Dr. Prescott says. “He’s a builder, constantly looking for opportunities to change things for the better.” In 2012, Dean Miller returned to Canada to serve as the dean of medicine and dentistry at the University of Alberta. Though he enjoyed it, Edmonton felt far from his family in Georgia—his daughter is a clothing designer in Atlanta and his son is a college student. “Professional opportunity here, plus personal decisions, led to my career move to NYMC.” For NYMC, Dean Miller was undisputedly the strongest candidate to lead the School of Medicine. He arrived in December 2014, diving into the challenge of steering the School of Medicine through several transitions, from the intense self-reflective process of re-accreditation to the ongoing immersion into the Touro University System—all while navigating currents of rapid change in the health care field as a whole. “When an organization has gone through a transition and is poised to move forward, it’s reassuring for us to have someone as Dean who absolutely knows the drill,” says Edward C. Halperin, M.D., M.A., chancellor and chief executive officer of NYMC, who served as interim dean of the School of Medicine following the retirement of Ralph A. O’Connell, M.D., and during the comprehensive search process. “The hospital market is fluid because of mergers, but we still need to keep our academic affiliations strong
C H I R O N I A N • New York Medical College
21
and preserve a space in which our students can learn. There’s a conscious effort to grow our research portfolio, despite the slowdown in federal funding. And in today’s era, clinical education is changing dramatically,” Chancellor Halperin adds. “These are the biggest issues Dr. Miller faces as Dean.” In Dr. Koestler’s role as faculty re-accreditation leader, collating information from across the School of Medicine, she draws confidence from Dean Miller’s experience as a 2014 voting member of LCME. “He’s in a position to know from experience what it takes to make this an outstanding medical school,” Dr. Koestler says, “and his presence will help us further enhance our mission and advance toward excellence.”
“Being comfortable with technology and being comfortable with holding someone’s hand at the bedside are equally important. We are still changing the way we think about humanism—starting with the qualities we look for in accepting students into medical school, and then in how we shape them professionally during their time here. The students I’ve met here are a professional, humanistic and thoughtful group; it’s been a pleasure as Dean to see how students bring such strong commitment to their learning environment, whether in the classroom, simulation center or clinic.” D. Douglas Miller, M.D., C.M., M.B.A.
“A JUMP STARTER” William Angus Steadman II, senior associate dean for the School of Medicine and vice president for strategic planning, credits Dean Miller with sustaining the momentum that Chancellor Halperin had steadily built during his three years as interim dean. “Dr. Miller arrived in the position of a jump-starter,” Mr. Steadman says. “He came in and said, ‘Let’s fire it up and really get it going.’ We were all working hard in our areas of expertise, and Dr. Miller brought the focus and vision that we needed to move forward as a school of medicine.” That unity of purpose—spanning from the scrutiny of self-study to help chart a path toward realignment— has inspired confidence in his colleagues. “Dean Miller can raise the school’s research profile, the quality of its curriculum, and the desirability of its graduates to the point that they are job-ready on day one, with more clinical experience under their belt than many residents,” says Chancellor Halperin.
CAREER DEVELOPMENT In Dean Miller’s view, the position of dean is less “ivory tower” than “keystone,” supporting and supported by those around him. “When I first took on administrative responsibilities in Saint Louis, I realized the main job description for a chair and dean is the career development of others,” Dean Miller says. “At the same time you’re running an organization, you’re shaping the careers of people who work with you.” Through frequent meetings and thought-provoking inquiries, Dean Miller has demonstrated his commitment to growth, professional and personal, among his colleagues. Says Mr. Steadman: “At one of the early meetings he had with
22
SUMMER/ FALL 2015
“Dean Miller can raise the school’s research profile, the quality of its curriculum, and the desirability of its graduates to the point that they are job-ready on day one, with more clinical experience under their belt than many residents.” Edward C. Halperin, M.D., M.A., chancellor and chief executive officer of NYMC
several senior leaders, he said: ‘We are going to develop your careers. What do you want to do—in terms of publications, research—to make your career more interesting and to make your CV better?’ That thinking got everyone realizing, ‘I can do more.’”
PASSION FOR TEACHING In addition to “deaning,” Dean Miller will be teaching at the School of Medicine. His course on “Health Policy for Health Professionals” reflects his abiding interest in policy. The new course evolved in response to nationwide student interest and feedback at MCG and the University of Alberta. “When I began working on the course in 2011, the Affordable Care Act had just brought the health care systems of the U.S. and Canada closer together than they had ever been. I described it to a colleague as a tectonic shift.” Widening his horizons, Dean Miller maintains a blog called “GlobalHealthSquare” and recently completed a Global Health Leadership Forum at University of California, Berkeley, “to understand what about health care is exportable; which principles of quality and access, whether from Nigeria, Singapore, or Canada, can be shared around the world. This will help infuse the curriculum with fresh content.” “My goal is to make students better informed about how health care works,” he adds, “so they can better advocate for patients in a healthcare system, even as it changes.” To that end, Dean Miller aims to ensure the School of Medicine curriculum includes both the technological advances that enhance student learning—including patient simulators and 3-D imaging— and the skills of interaction without a handheld device. “It’s exciting how all the ‘little data’ from FitBits and personal health metrics adds up to big data sets used to predict and model care, with precision medicine tools identifying the best care possible,” he says. “It’s more helpful than previous eras, when you relied on epidemiology and patients were simply part of a cohort. That’s where I think technology will have the biggest impact on medicine going forward.” But, he adds, the whole patient—not just his or her little or big data—remains at the core of patient care. “Being comfortable with technology and being comfortable with holding someone’s hand at the bedside are equally important,” Dean Miller says. “We are still changing the way we think about humanism—starting with the qualities we look for in accepting students into medical school, and then in how we shape them professionally during their time here. The students I’ve met here are a professional, humanistic and thoughtful group; it’s been a pleasure as Dean to see how students bring such strong
commitment to their learning environment, whether in the classroom, simulation center or clinic.” From health policy to clinical skills to biomedical ethics, Dr. Koestler applauds Dean Miller’s support of “self-directed learning” initiatives in the School of Medicine. “The amount of material students have to know is expanding,” she says, “and we want to make sure students are enhancing their knowledge constantly: being pro-active rather than re-active.”
BUILDING ON TRADITION Colleagues agree: it is Dean Miller’s blend of experience and fresh perspective—plus the balance of careful listening and resolute acting—that will forge a new path for the School of Medicine. “Doug has made his mark at every institution for which he’s provided leadership,” says AAMC’s Dr. Prescott. “Colleagues search him out for advice and counsel. I’ve found him to be an excellent listener, which is a key attribute for any dean: to listen carefully and learn. On top of that, he brings expertise, drive and the will to make a difference. If he feels strongly enough to do it, he will do it right.” And so Dean Miller’s newcomer status on campus could serve as his greatest asset. Chancellor Halperin observes that “neither Dean Miller nor I attended medical school at NYMC, were house officers in NYMC residencies, or were members of the faculty at NYMC before assuming our administrative roles. We are a chancellor and a dean who have come from the outside and cannot say, ‘Let’s do things the way we have become accustomed to doing things at NYMC.’ This outsider status has advantages and disadvantages. An outsider entering into a new institutional culture must be a good listener. As Dean Miller assimilates into the NYMC culture, he must strive to take the school to a new level: a world-class institution true to its past, building on its traditions, and poised for a great future.” It’s a long-term strategy that has the advantage of unfolding day by day. There’s no doubt Dean Miller is already moving and thinking ahead. On a personal note, he appreciates that Valhalla has placed him once again in the same country as his wife, Heather, and his children, Caroline and Brendan, who live in Georgia. Next step: finding a family home within driving distance of the College campus. “My skills are based on learning how to move forward with team-based approaches to the challenges we face,” he says. “The advantage of our smaller school size allows us to make changes and decisions rapidly without a tremendous amount of bureaucracy. We can be more nimble in seizing on future opportunities.” ■ C H I R O N I A N • New York Medical College
23
HUNGERING FOR JUSTICE IN HEALTH CARE
24 24 SPRING/ SUMMER SUMMER/ FALL SUMMER/ FALL2015 2015 2015
Rebecca McAteer, M.D. ’08,
Brings Healing to Nepal, Before and After the Earthquake By Andrea Kott, M.P.H. Under the best of circumstances, practicing medicine in Nepal would have been challenging. Rebecca McAteer, M.D. ’08, knew this. She knew she would be working in one of the world’s impoverished countries, where most people live in remote, rural mountain valleys without adequate food, water or sanitation. She knew that population health was poor, the result of limited access to clinics, reached only by trekking for days on steep, jagged footpaths. Yet, a “hunger for justice” compelled the family medicine physician to work in this inhospitable landscape arriving in September 2013. In late April of 2015, things became more challenging when a 7.8 magnitude earthquake struck near the capital city of Kathmandu. Dr. McAteer didn’t want to be anywhere else. “Being a physician and having the training I have, I felt like I had been given a lot,” she said. “I wanted to help make access to health care more just and fair.” Growing up in White Plains, N.Y., Dr. McAteer always knew she wanted to be a doctor. Two factors motivated her: a fascination with the human body, and her mother, the late Mary Hawkins McAteer, M.D. ’75. “I’ve always been drawn to medicine, and my mother was my model,” she said of the ophthalmologist, whose work with indigent people in Central America and Africa inspired New York Medical College’s Mary Hawkins McAteer, M.D. ’75, Memorial Scholarship Award, which honors graduates who demonstrate their dedication to medical care for the world’s neediest by gathering fourth-year clinical experience in an undeveloped country. “She loved her work and she was excellent at it.” After graduating from the College of William & Mary in Williamsburg, Va., and she earned her medical degree at NYMC with induction into Alpha Omega Alpha, the national medical honor society, Dr. McAteer completed her family medicine internship and residency at Lancaster General Hospital in
C H I R O N I A N • New York Medical College
25
“ Being a physician and having the training I have, I felt like I had been given a lot. I wanted to help make access to health care more just and fair.” Rebecca McAteer, M.D. ’08 Pennsylvania. The year before she moved to Nepal, she finished an academic faculty development fellowship in medical humanities at Georgetown University Medical School in Washington, D.C. A woman of deep faith, and long intrigued with Asian culture (“I even belonged to the Asian cultural society in high school!”), Dr. McAteer joined United Mission to Nepal (UMN), which assigned her to Tansen Mission Hospital. The 60-year-old, 165-bed facility is located in the Palpa District of western Nepal, a nine-hour car ride from Kathmandu. She made a two-year commitment to the hospital, and spent three months studying intensive Nepali—four hours a day, five days a week. The language lessons helped, but what ultimately made her fluent was working and living in Nepal. “It’s amazing how you learn the language by hearing it constantly,” she said during a phone interview from her apartment in Tansen. “It’s full immersion, sink or swim.” Shortly after her arrival in Nepal in September 2013—and once she had the language under her belt—she began logging 12hour days, five to six days a week. She rotated between the pediatric, maternity and adult medical units, working with a team of physicians to treat a steady overflow of patients suffering from hypertension, diabetes, stroke, myocardial infarctions, viral gastroenteritis, pneumonia, iron deficiency anemia, urinary tract infections, rheumatoid arthritis and more.
CULTURE SHOCK Although she tried to prepare herself, she was nonetheless struck by the prevalence of infectious diseases—typhoid fever, leptospirosis, meningitis, malaria, tuberculosis and HIV—many of which are not even routinely treated in the U.S. “It’s difficult to see patients who are suffering and dying from potentially reversible or preventable things that you don’t have the resources to fix,” she lamented. She was also dismayed to see illnesses such as cancer,
26
SUMMER/ FALL 2015
diagnosed at advanced stages because of lack of access to health care; or heart failure, stemming from late presentations of untreated strep throat or congenital heart disease. In her blog, WhereGodCalls (https://wheregodcalls.wordpress.com), she described an 18-yearold woman with “severe systolic heart failure and a massive MCAterritory ischemic stroke with hemiparesis—the tragic, preventable sequela of longstanding rheumatic heart disease.” But her greatest shock came at 11:56 a.m. on April 25, while she was on a spiritual retreat with colleagues in Pokhara, about four hours north of Tansen. “We began to feel the earth shaking and the windows rattling. The ground was swaying and the water in the pool was sloshing over the edges,” she recalled. “Having grown up near trains and under plane flight paths, my first thought was, ‘There must be an airplane overhead or a train nearby.’ Within a second we all realized it was an earthquake.” She couldn’t sleep that night. “My heart was still pounding,” she recounted. Early the next morning, after a 5:30 a.m. aftershock jolted her awake, she and fellow Tansen physician Josh Riggsbee, M.D., responded to a request from UMN to partner with a team from the International Nepal Fellowship (INF) and travel to the Gorkha district, near the epicenter of the earthquake, to assist in medical relief efforts, and assess structural damage and humanitarian needs. A jeep brought them to Pokharidanda and Mailun, villages where 80 to 90 percent of the buildings had been completely demolished. They set up outdoor medical clinics, conducted triage and treated 450 patients who suffered mild-tomoderate crush injuries inside collapsing stone houses, or from falling rocks outside. “The vast majority of problems were anxietyrelated aches and pains,” she noted. “Anyone who was severely injured had been taken out by a road that could accommodate vehicles.”
AFTERMATH No road could take them to the next two villages, however. Located in a more remote part of Gorkha, Keraunja and Runchet were more than a day’s walk from the nearest road. “The geography was so severe, the mountains so steep, and the risk of landslide so great, there was no way to walk or drive there,” Dr. McAteer explained. She and Riggsbee had to take a helicopter. From the air, they surveyed one flattened village after another. Suddenly, they were in the middle of a fierce thunderstorm that forced their pilot to land on the nearest possible spot: the flat ridge of a 6,000–foot mountain cliff. “It was a bit of a white-knuckle ride.” An hour later, they flew to Keraunja, a village perched atop a terrace, carved into the side of a nearly-vertical 7,000-foot mountain. “We were standing in this terraced field on the side of a steep mountain, in the rain, in what was left of the village,” she recounted. “People came out staring at us and we asked, ‘Is there somewhere for us to go?’ They said, ‘No.’ Every building, including the village health post, was leveled.” Additionally, three shepherds along with 20 cows and 90 sheep that had been grazing nearby, had all perished in a giant landslide. Compounding the crisis, the footpaths were all destroyed. “The nearest town was a two-day walk away,” Dr. McAteer said. “These people had a four-to-five-day food supply and no way of getting more.” Facing a night in this mountain village, the two physicians were overjoyed when they discovered that the USAID (U.S. Agency for International Development) supplies their helicopter had dropped off included a sack full of tarps, mats and blankets. “The contents of this plastic sack meant we would not have to sleep out with the leeches in the mud and rain.” Because debris from the earthquake had blocked all the roads, and landslides were likely, Drs. McAteer and Riggsbee needed a helicopter to take them off the mountain. But, they had no cell
phone service and their cell phone batteries were running low. At 6:00 a.m. the next morning, they trudged for an hour up the mountain ridge to a spot where they could get reception, and called the INF and their colleagues in Pokhara. Then, as they climbed down to the next village to assess injuries, they spotted an Indian Army helicopter dropping off supplies. “We saw it circling and coming closer, and we realized this was our one shot,” Dr. McAteer said. Dashing downhill, they flagged the helicopter, and somehow conveyed to the pilots their need to fly back to Pokhara and to evacuate several patients who were too injured to walk. A day later, Dr. McAteer was back at the hospital in Tansen. Gradually, the emotions she experienced during and after the earthquake surfaced. “There was a sense of disconnect,” she said. “You go from being terrified on the side of a mountain in the earthquake’s epicenter, and in a few hours you’re sitting at a restaurant eating beetroot salad.” She paused, then continued: “It’s disturbing to realize that even though I had adequate food and whatever choice of food I wanted, there were people still in the situation that we left.” She added, “I’ve been more tearful and irritable. It must be survivor guilt.” It will take decades for Nepal to heal physically and financially from the earthquake, Dr. McAteer said. Moreover, she stressed, how Nepal goes about healing will influence its long-term health. “While there are needs, there are also enormous resources here in the form of the Nepali people. There is an unflinching endurance about them, and any help must be given in partnership with them to affirm their ability to contribute to their own country.” As she prepares to return to the United States, Dr. McAteer ponders the overwhelming rebuilding that awaits Nepal. She finds comfort in knowing that she can continue to play a role in its repair. “You can’t compare the care you’re giving here to the care you give in America. You have to compare it to the care they would receive if you weren’t there.” ■
C H I R O N I A N • New York Medical College
27
ALUMNI and DONOR Events School of Medicine Alumni Reunion
T
he School of Medicine Alumni Association hosted the 132nd annual Alumni Banquet and Awards on May 17 at the Sheraton New York Hotel and Towers in New York City. Alumni reconnected with classmates and members of the classes of 1965 and 1990 were honored with gold and silver diplomas, respectively.
Chancellor’s Circle Reception
E
dward C. Halperin, M.D., M.A., chancellor and chief executive officer, welcomed donors and guests to a Chancellor’s Circle Reception on June 3 at the Clinical Skills and Disaster Medicine Training Center.
28
SUMMER/ FALL 2015
Founder’s Dinner
M
ore than 300 guests enjoyed an evening of dining and dancing at the Founder’s Dinner on October 26 at the Ritz-Carlton in White Plains, N.Y. The evening raised nearly $430,000 for NYMC.
C H I R O N I A N • New York Medical College
29
CHIRONIAN
ALUMNI PROFILE
BOARD OF TRUSTEES
A Military Medical Leader Outshines Her Personal Best
Summer/Fall 2015
Felicia F. Pehrson, M.D. ’87, FACC
BY ANDREA KOTT, M.P.H.
Dr. Mark Hasten Chairman of the Board Alan Kadish, M.D. Robert Alter, M.D. Mr. Gary Barnett Howard Baruch, M.D. Ben Chouake, M.D. Rabbi Menachem Genack Gary Gettenberg, M.D. ’83 Mr. Michael Karfunkel Mr. Moshe Lichtenstein
Mr. Joseph Mark Stephen J. Nicholas, M.D. ’86 Martin Oliner, Esq. Raymond M. Planell, Esq. Mr. Ronald F. Poe Mr. Stephen Rosenberg Henry Saphier, M.D. ’61 Joseph Schwartz, M.D.
ALUMNI ASSOCIATION BOARD OF GOVERNORS OFFICERS 2014-2015
Officers Henry I. Saphier, M.D. ’61 President
Robert J. Furey, M.D. ’62 Secretary
Charles W. Episalla, M.D. ’88 President-Elect
Jay D. Tartell, M.D. ’82 Archivist
Joseph L. Giamelli, M.D. ’02 Vice President
Eileen M. Dieck, M.D. ’86 Immediate Past President
Jay Y. Lee, M.D. ’86 Treasurer 30
SUMMER/ FALL 2015
From a young age, Felicia F. Pehrson, M.D. ’87, FACC, knew she wanted to be a doctor. But life is full of detours, and Dr. Pehrson took one that forever changed her course when she went into the U.S. Army. There, the 2015 Alumni Association Medal of Honor recipient discovered her love of pediatrics, medical leadership and the chance to accomplish more than she ever imagined. Dr. Pehrson grew up in Maine, the fifth of six children, with parents who survived the Holocaust. Her life plan was straightforward: attend medical school, specialize in surgery and return to Maine to practice. But, during her first year at New York Medical College, her father became ill and she needed tuition assistance. She joined the Army. “My original plan was to pay back my three years of military service and be done,” she says. The Army had other ideas: constantly giving her opportunities that propelled her to the highest levels of military medical leadership, all the way to her current position as director of healthcare delivery in the Office of the Surgeon General. “Here I am, more than 30 years later, still in uniform.” Dr. Pehrson hadn’t dreamed of becoming a pediatrician or a pediatric cardiologist, but she fell in love with the challenges— and the children—during her internship and residency at Washington, D.C.’s Walter Reed Army Medical Center (now Walter Reed National Military Medical Center in Bethesda,
MILESTONES
Alumni Achievements Md.). It was while working at the 121st Medical Evacuation Hospital (now the Brian Allgood Army Community Hospital) in Seoul, South Korea, where she mobilized the air-evacuation of an extremely premature, 540-gram (approximately 1.2 pounds) baby, that she recognized her passion for leading under pressure. The Army recognized it too. S he rose swiftly. In 1994, soon after completing her pediatric cardiology fellowship at the Hospital for Sick Children in Toronto, Ontario, she became a service chief; first at Landstuhl Regional Medical Center, a U.S. overseas military hospital in Germany, then at Tripler Army Medical Center in Honolulu, Hawaii. She advanced to department chief at Womack Army Medical Center at Fort Bragg in North Carolina. “That was when I realized how much I enjoyed the ability to influence health care beyond the individual patient,” she recalls. uring the next decade, she was selected for prestigious D positions, including chief of clinical operations for the MultiNational Force–Iraq, for which she was awarded a Bronze Star Medal. As deputy commander for clinical services and chief medical officer at Walter Reed from 2008 to 2011, she was responsible for the care of hundreds of thousands of patients annually, many with the most complex injuries of war; she oversaw 4,000 military and civilian staff; supervised 66 graduate medical education programs; and balanced hundreds of millions of budgetary dollars, earning a Legion of Merit military medal. r. Pehrson’s numerous honors also include the German Armed D Forces’ Badge for Military Proficiency, a testament to her athletic steeliness: she excelled in track and field events such as shot put, long jump, 100–meter and 2000–meter runs; as well as a 200–meter swim, a pistol competition, and a 10– mile march carrying a 40–pound pack. “I undertook this as a personal challenge at a late age, as a hospital commander and as a role model for my soldiers. I wanted to demonstrate what can be accomplished when you put your heart and mind into something.” T oday, Dr. Pehrson directs health care delivery and clinical policies for the U.S. Army. In addition, she chairs the Women’s Health Task Force, and serves on another task force that is working to make the Military Health System a ‘high reliability’ health care organization. She hopes to return to pediatric cardiology someday. When she does, she will still be a leader. “I have a vision for how to improve organizations, I can see a path to get there, and I have the passion to make it happen.” ■
STAY IN TOUCH We would love to share your most recent news and accomplishments in our next issue of the Chironian. If you have any professional accomplishments or developments, published a book, or have any family news to share, we would love to hear from you. Alumni Relations New York Medical College 40 Sunshine Cottage Road Valhalla, NY 10595
Submit your updates to http://www. nymc.edu/AlumniAndDevelopment/ Secure/address.asp or mail them to:
To stay up-to-date about the latest news about the College and our alumni network; Like us on Facebook. www.facebook.com/nymedcollege Follow us on Twitter. @nymedcollege Connect with us on Linkedin Follow us on Instagram. instagram.com/nymedcollege
The 10s
Karel R. Amaranth, M.P.H. ’10, assumed the position of executive director of Victims Assistance Services, a component of Westchester Community Opportunities Program (WestCOP). Her letter to the editor was published in the May/June 2015 issue of The Nation’s Health, a publication of the American Public Health Association.
Candice A. Kowalewski, M.P.H. ’13, works for Atlantic Environmental providing field surveys in indoor air quality, industrial hygiene, working with asbestos, safety, environmental research, evaluating data, and report writing. She is also a member of the New Jersey American Industrial Hygiene Association. Isabelle M. Matejovsky, D.P.T. ’13, had an abstract accepted in the neurology section at the 2015 American Physical Therapy Association Combined Sections Meeting. Kumar S. Gandhi, M.D. ’11, recently completed his residency in internal medicine and has an urgent care and family medicine position in Orange County, Calif. “I enjoy seeing patients of all ages, from neonates to adults. I look back on my tough New York training and am proud to be a New York Medical College graduate,” he writes. Nickolas C. Teigen, M.D. ’11, will be starting a fellowship in maternal fetal medicine at Montefiore Medical Center in N.Y. to be completed in June 2018.
Allyson L. Chesebro, M.D. ’10, completed her diagnostic radiology residency at Brigham and Women’s Hospital and Harvard Medical School on June 30 with a dedicated fellowship in breast imaging. She began a one year fellowship in oncoradiology at Dana Farber Cancer Institute/ Brigham and Women’s Hospital and Harvard Medical School on July 1.
The 00s Rebecca McAteer, M.D., ’08, is currently serving at Tansen Mission Hospital in Western Nepal, having completed a faculty development fellowship in medical humanities at Georgetown University. Read her blog at https://wheregodcalls. wordpress.com. She also recently had two papers accepted for publication in an upcoming issue of the AAMC’s journal Academic Medicine (accept
C H I R O N I A N • New York Medical College
31
ed, publication pending): Treatment’s Winter: On Cancer Treatment and Its Metaphors (with Melissa Chan, M.D.) and The Art of Observation: A Pedagogical Framework (with Caroline Wellbery, M.D., Ph.D.). Linda Huynh M.P.H. ’07, got married in September 2014 and is now Linda Woo. Miho J. Tanaka, M.D. ’06, reports she spent three years in St. Louis, where she served as director of the Women’s Sports Medicine Initiative and was the first female to be a team physician for the MLB St. Louis Cardinals. She will return to Baltimore this summer as the new director of the Women’s Sports Medicine Program at The Johns Hopkins Hospital.
Marlyn Ramos Lamboy, M.D. (GME ’05), has been named division chief of physical medicine and rehabilitation at Berkshire Medical Center in Pittsfield, Mass., and recently had an article, Clinical Experience With Continuous Intrathecal Baclofen Trials Prior to Pump Implantation, accepted for publication in the journal PM&R. Jason Tenzer, M.P.H. ’04, took office on January 1, 2015 as president of the Healthcare Leaders of New York, the local chapter of the American College of Healthcare Executives. David A. Tompkins, M.D. ’04, received a master of health science degree in clinical investigation from the Johns Hopkins Bloomberg School of Public Health in August 2014 with funds from his NIH-funded Career Development Award. Lynn Bray, M.S. ’01, is working in clinical trial management at Boehringer Ingelheim. David L. Pierce M.D., Pre-Internship ’00, is the chief medical officer at Millard Fillmore Suburban and DeGraff Memorial Hospitals in Williamsville, N.Y.
32
SUMMER/ FALL 2015
The 90s Jeffrey H. Hsu, M.D. ’97, was appointed regional chief of vascular surgery for Kaiser Permanent Southern California, leading approximately 40 vascular surgeons across 14 hospitals. Neil Jacobson, M.S. ’97, formed a new company CHAI Insurance Consulting Group LLC (www.cicg.co) and received four patents in business methods from the United States Patent and Trademark Office. Arthur A. Blain, M.D. ’96, was appointed chief medical officer of Mountain Health and Community Services in Alpine, Calif. Eastlyn Harding-Marin, M.D., Fifth Pathway ’96, is a clinical preceptor for Emory University Medical School and Georgia State University NP Program. Steven A. Urban, M.D. ’94, had a book published in June, 2014, Mere Christianity Study Guide: A Bible Study on the C.S. Lewis Book Mere Christianity (A Study Course for a Thinking Faith). He writes, “Disappointed by the shallowness I often encountered in many Christian circles, I taught two full courses on Lewis’ Mere Christianity going into the depths of what this Oxford and Cambridge scholar wrote. I was surprised by the class responses I received and, when convinced that publishing was more economic than printing, double-surprised that more than 1,000 copies sold in 10 months. I have had good feedback from both Protestants and Catholics.” Col. Roger A. Gallup, M.D. ’91, retired this summer from the U.S. Army, leaving as the deputy commander for clinical services (chief medical officer) of the Carl R. Darnall Army Medical Center, Fort Hood, Tex. He joined the Williamson Pulmonary and Sleep Associates group and has assumed the duties of the ICU medical director at Seton Medical Center Harker Heights in Seton Harker Heights, Tex. Richard Covin, M.D. ’90, writes, “I have a new grandbaby, now up to three. I am living the good life after retirement.” Lidia F. Vitale, M.D. ’90, was named a “Top Doc” in New Jersey Monthly magazine for the fourth consecutive year and she was on the cover of the November 2014 issue.
ALUMNI PROFILE
Catherine MacCartney, D.P.T. ’06 Tackle Challenges and Set New Goals BY ANDREA KOTT, M.P.H.
More than once in her life, Catherine MacCartney, D.P.T. ’06, has surprised herself. She declared biology her major in college after barely passing high school science. She fell in love with working in a hospital after setting her sights on outpatient care. And, after years of wishing for the confidence to become a professional body builder, she won her first pro competition. Though these experiences may seem unrelated, each gave the highly-motivated MacCartney a goal to achieve. “If I have something to look toward, I focus better on it,” says the assistant supervisor of acute care at NewYork–Presbyterian Hospital. “I always need a project.” Becoming a physical therapist was not one of MacCartney’s goals, especially during her years at Nyack High School, where she struggled in science. Even at St. Thomas Aquinas College in Sparkill, N.Y., where she began as a fine arts and graphic design major, she veered away from science, until graduation requirements pushed her to take one course in the subject. She took marine biology and was completely enthralled with the course. By junior year, she had changed her major to biology. A longtime athlete and former personal trainer, MacCartney wanted a career that would combine her newfound love for science with her passion for fitness. Physical therapy was a perfect fit. She entered the field with the intention of working in an outpatient orthopedic setting. “I wanted to treat sports injuries,” she explains. “I didn’t want to work in a hospital.” But an opportunity to specialize in acute-care at NewYork– Presbyterian Hospital—her first job offer after graduating from NYMC’s School of Health Sciences and Practice—was not one to pass up. She figured she’d stay for a while, then move on. “Nine years later, I’m still there.” In fact, in 2011, she was promoted to assistant supervisor. “I gave myself five years to have an administrative position, and I got the promotion within a month of my five-year anniversary.” Just as MacCartney fell in love with—and excelled at—science, so did she fall in love with acute inpatient care. “I totally swung in the other direction,” she says, sounding surprised. “I love being in the hospital.” She divides her clinical time between patients in the emergency department, where she is the head physical therapist, the neurology department and among those who have lymphedema.
The 80s Eugene A. Conrad, M.S., Ph.D., M.P.H. ’89, reports that the Stamford men’s caregiver support group that he leads has reached the five-year survival mark. “It started with three members in January 2010 and now we have ten. The men have dementia-diagnosed spouses and are keenly interested in learning, comparing experiences, and socializing. I am also a caregiver for my wife who has AD,” he writes. Katerina A. Zavaras, M.D. (GME ’89), received the Award for Excellence in Clinical Precepting by the University of Pittsburgh, School of Medicine.
“We get the sick of the sick,” she says, referring to patients who are recovering from brain or spinal injury or surgery, stroke, or who have progressive neurological diseases such as Parkinson’s, amyotrophic lateral sclerosis or Huntington’s. “Even if they pass away, their time here was made better because we helped them. That’s what makes my job totally worth it.” In 2014, MacCartney became a certified lymphedema therapist, making her a specialist in the evaluation, education and treatment of the condition, which involves local fluid retention most commonly in the arms or legs. “Becoming a certified lymphedema therapist became my project.” Some projects are personal, like competitive bodybuilding. It was during college, when the former dancer and high school lacrosse player started working out in a gym and lifting weights when the bodybuilding “bug” bit her. “For 12 years, I wanted to compete but I was too afraid,” she recounts. At the end of 2012, she mustered the courage to step on stage. “I won my first two shows,” she says, proudly. MacCartney approaches bodybuilding as she does everything else: with discipline and dedication. She begins every day with an hour-long 5:30 a.m. workout before heading to work, equipped with meals of chicken, vegetables, rice and sweet potatoes. After work, she hits the gym again. “When I’m dedicated to getting something done, it gets done,” she says. “I get home at 7 or 8 p.m., pack up my meals for the next day, and do it all over again.” Such dedication has taught her that taking on challenges is the best remedy for self-doubt. “Don’t ever sell yourself short,” she says. “Don’t ever say you can’t do something.” ■
Law and, this year, Lisa will start Upstate, Brandon will graduate KCC, Sammy will graduate high school and Ronny will graduate middle school.” Jeffrey N. Broder, M.D. ’83, reports his son, Jared, graduated from Lakeside High School in Evans, Ga., and got a scholarship to play lacrosse at Reinhardt University, in Weleska, Ga. Jonathan D. Kunis, M.D. ’82, is an addiction medicine specialist providing outpatient addiction treatment at Manatee Glens East in Bradenton, Fla. Ilene Newman, M.D. ’81, writes, “Hello to my fellow ’80 and ’81 alums. I am now in my 30th year of ob/gyn in San Jose, Calif., and I am still thrilled to be here. Jerry and I are enjoying our first ‘empty nest’ year. I’d love to hear from you, especially if you’re visiting the bay area.”
Robert M. Yacynych, M.D. ’88, reports his son, Eddie, was on the television show America’s Got Talent as part of the Flight Crew jump rope team, his son, David, is a junior at the University of Maryland studying biochemistry; daughter, Janette just graduated from high school; and son, Michael, is enjoying high school soccer. Dr. Yacynych was also elected vice president of the medical staff at MedStar Harbor Hospital in Baltimore.
Steven Shankman, M.D. ’81, was recently inducted as a Fellow in the American College of Radiology.
William J. Kaiser, M.D. ’87, and his wife, Lindsey, welcomed their daughter, Lillian Sophia, into the family on December 16, 2014. Her siblings include Will, Katie, and Walker.
Lisa Borg, M.D. ’80, is medical director for two drug and alcohol rehabilitation programs: Arms Acres in Queens and Daytop Village in Manhattan. She is also in private practice on the upper east side of Manhattan and has three children in college: Bard, NYU and Tulane, and her daughter is pre-med.
Jeanne M. Marconi, M.D. Fifth Pathway ’86, received a Lifetime Achievement Award from the Fairfield County Medical Association. She is a practicing pediatrician currently on the executive committee of the American Academy of Pediatrics section on Administration and Practice Management as well as Executive Advisory Board for the Committee on Coding and Nomenclature. Mitchell S. Kramer, M.D. ’85, has been designated as a COEMIG (Center of Excellence in Minimally Invasive Gynecologic Surgery) surgeon by the American Association of Gynecologic Laparoscopists which includes robotically assisted laparoscopic surgery. He has also received an appointment as assistant clinical professor at NYU Langone School of Medicine. Amy Batterman, M.D. ’83, is still in dermatology practice in Brooklyn and writes, “Rebecca is at Hofstra
Christopher J. Kaczmarski, M.D. ’80, writes, “After 30 years as a general surgeon and specializing in the field of bariatric surgery for the past 16 years, I will soon be making a new career move. As of July 1, I am planning to work for the Vohra PostAcute Physicians organization in the specialty of wound care. I decided that it’s time for a change, hoping to continue practicing in this new field happily for a while longer! If any other graduates who’ve done the same have any advice or comments, I would welcome them!” C H I R O N I A N • New York Medical College
33
The 70s Douglas A. Byrnes, M.D. ’77, has a private solo cardiology practice in Huntington, N.Y., and is assistant clinical professor of medicine at SUNY Stony Brook. He has prior service as president of Huntington Hospital medical staff and board of directors of Huntington Hospital.
Jeffrey Hall Dobken, M.D. ’73, M.P.H. ’15, was awarded an NYMC Academic Excellence Award in Environmental Sciences and was inducted into Delta Omega Honorary Public Health Society. He is also a visiting lecturer in the NYMC School of Health Sciences and Practice.
Jeff A. Kraut, M.D. ’72, recently published invited review on lactic acidosis in the New England Journal Stephen G. Marcus, M.D. ’76, is president of Cantex Pharmaceuticals, of Medicine. He is professor of medicine at UCLA and editor of the acid a clinical stage company developing base feature of American Journal of novel treatments that block critical mechanisms by which cancer spreads Kidney Disease and co-director of the American Society of Nephrology and resists treatment. course on acid base and electrolyte disorders.
Vincent J. Vigorita, M.D. ’76, recently returned to the Miskito Coast of Nicaragua to revisit the sites and medical professionals he worked with during his senior elective in 1976. “It was a very personal and professionally satisfying reunion with many,” he writes. Henry J. Green, M.D. ’75, is now living in both Fresno and Mountain View Calif., and working primarily at Rebekah Children’s Services in Gilroy. His Dad, Michael Green, M.D. ’50, passed away in June 2013 at the age of 93. Margaret M. Grimes, M.D. ’75, has been elected president of the American Board of Pathology for a one-year term. Sarah A. John, M.D. ’75, continues to practice locum tenens urgent care and is the lead physician for We Care to Share, Chantal, a medical relief team in Haiti. www.ChantalHaitiMission.wordpress.com “I invite classmates to join our next trip,” she writes. Dan K. Morhaim, M.D. ’75, was re-elected to his sixth four-year term in the Maryland General Assembly.
34
SUMMER/ FALL 2015
Kathleen G. Nelson, M.D. ’71, is currently clinical professor of pediatrics at Keck School of Medicine of USC/Children’s Hospital in Los Angeles. She will receive the Distinguished Service Award from the Association of American Medical Colleges in November for her service to the Council of Faculty and Academic Societies (CFAS). Robert E. Crootof, M.D. ’70, and his wife, Linda, are both retired, spending summers in Wolfeboro, N.H. and winters in Sarasota, Fla. “Despite major and minor health issues over the last 15 years, Linda and I are both well, enjoying retirement, traveling both overseas and to visit children in Manhattan, Bozeman, Mont. and L.A. Linda assures me that we did both work hard enough to be able to live nicely like this. I am still sad that my first-year apartment mate, Jeff Frank [Martin Jeffrey Frank, M.D. ’70] died two and a half years ago after a long illness,” he writes. Ian Gale, M.D. ’70, has retired and moved to the Phoenix area after 40 years of urology practice in the San Fernando Valley of Los Angeles. “My wife, Lisa, and I plan to travel more extensively than we have in the last five years. We’ve been in 55 countries and six continents. Only Antarctica is left and that will happen in December 2015. Our seven children are scattered throughout the United States and we plan to visit them all between traveling, golf and volunteering for the Wounded Warrior Project. I have a full and busy life,” he writes.
ALUMNI PROFILE Paul Mieyal, Ph.D. ’00
A Scientist-Investment Manager on the Cutting Edge BY ANDREA KOTT, M.P.H.
In the year that Paul Mieyal, Ph.D. ’00, earned his doctorate in pharmacology from New York Medical College, biotechnology stocks were booming. “Any company that had ‘gen’ in its name for ‘genetics’—people couldn’t get enough of it,” Mieyal says. And yet, there was a shortage of people with the scientific training to advise biotech investors. That’s where Mieyal found his niche. Instead of taking the traditional path into academia, Mieyal began using his scientific expertise to counsel firms on biotech investments. Today, as vice president and director of life sciences investments for Wexford Capital in Greenwich, Ct., he evaluates cutting-edge research on new medical devices, drugs and antibodies to determine if investing in their development makes good financial sense. A “hardcore scientist at heart,” Mieyal grew up in laboratories. The son of a pharmacology professor, he spent time in his father’s lab at Case Western Reserve University in Cleveland, Ohio, and worked in those labs during his undergraduate years at the school, where he earned his bachelor’s in chemistry and psychology, and where his father still teaches. “I was very comfortable in the lab from an early period,” he says. “I especially liked the biological sciences, the study of living cells and how the body works.” Mieyal pursued his love of life sciences at NYMC, where he worked as a lab tech before formally entering the doctoral program. He noticed, as internet and biotechnology companies began proliferating, that jobs in research and academia—and the federal grant funding on which they depended—were growing scarce. So, he began reconsidering the academic career he had initially envisioned. “There weren’t a lot of university positions available,” he recalls. “I faced the prospect of finishing my Ph.D. and having an open-ended post-doc period, which would have been highly dependent on getting a first grant. I wanted to explore what alternatives were possible.” As he worked toward his doctorate, Mieyal took night classes in accounting, marketing and economics. Then, he took an internship at an investment firm. “The planets aligned and I was lucky enough to be introduced to a firm that was looking for an entry-level investment analyst who could focus on
Joseph S. Vetrano, M.D. ’70, has decided to retire after 38 years at Riverview Medical Center as associate corporate medical director of Meridian Behavioral Health, medical director of the Booker Behavioral Health Center and chairman of the Department of Psychiatry. He will continue his private practice of psychiatry in Red Bank, N.J. “I look forward to more time with my grandkids, Nick and Deanna, and plan on at least one bucket list trip a year. I would enjoy hearing from you at drjv1945@yahoo.com,” he writes.
Richard Besserman, M.D. ’64, is an operations executive and founding member of the Arizona State University Center for Emergency Management and Homeland Security.
The 60s
Michael J. Feinstein, M.D. ’64, has retired from his urologic practice and is working as a part-time medical director for Excellus, the regional Blue Cross/Blue Shield insurer. “I am still in Rochester, N.Y., but as both my daughters and grandchildren live in California, I spend a fair amount of time out there,” he writes.
Glen Joshpe, M.D. ’69, reports that his latest book, Retirement Reflections, is available on amazon. com. It features a romantic comedy about two people who, independent of each other, meet at the Brooklyn Bridge planning to end it all and contains humorous vignettes. Dr. Joshpe is also the author of Pearls and Pitfalls of Medical Malpractice. John J. Bouvier, M.D. ’66, is “working wonderfully hard at retirement!”
biotech stocks. I accepted the job before I defended my thesis.” He later confirmed his new direction by completing the Chartered Financial Analyst (CFA) program. Today, instead of being at the bench, Mieyal helps his company decide whether to invest in cutting-edge drugs and devices that others are developing. “It’s because of my expertise in pharmacology that I can look at the development of new drugs and understand what hurdles companies will have in clinical trials and what safety issues and risks they may face.” He finds deep satisfaction in helping successful companies that create therapies to benefit people. “It feels good when you see a company succeed,” he says, referring to one that has developed a device for children with scoliosis. “We’re at the front lines of providing capital to entities that are giving kids access to new treatment.” Mieyal has always thrived on scientific innovation, but he doesn’t need to drive the science. “My nature is to look at new things,” he says. “There are new companies being formed every year, and my job is to continue to look at the landscape of what’s evolving to see what we should make an investment in. It’s always exciting and dynamic.” ■
Richard S. Lefleur, M.D. ’66, just turned 75-years old and after 45 years of working in interventional radiology at NYUMC, has decided to ease off and is now just teaching and attending conferences. He has two grown children and two grandchildren. “It is nice to sleep late. I am still married to same wonderful woman, but miss my wild years at NYMC. Looking forward to our 50th reunion in 2016. And so time goes on! You can email me at rlefleurmd@gmail. com,” he writes. Arthur Calick, M.D. ’65, rejoined volunteer faculty at University of California Irvine as clinical professor in the Department of Internal Medicine. Ron J. Cavanagh, M.D. ’65, M.P.H., works for Northern Valley Indian Health in Chico, Calif., concentrating on the integration and collaboration of psychiatry within primary care. Carl R. Saviano, M.D. ’65, writes, “My wife and I had a wonderful time at the 50th reunion but it was too short. I have contacted a few alumni and suggested a get together again in a year or two for the Class of 1965 in New York City. I will look into it further and would appreciate opinions and ideas.”
Frank P. MacMillan, M.D. ’64, is retired after 46 years in medicine at Pentucket Medical Associates in Haverhill, Mass. He was honored with having a conference room named after him there and was honored as Physician of the Year by Mass Medical Associates, Northern Essex region. He is now playing more golf and enjoying his children and grandchildren. John Brodsky, M.D. ’63, is a member of the board of the Tomkins Institute, applying affect script psychology to motivated behavior and a theory of history. David L. Lanter, M.D. ’63, retired 13 years ago and is living in Delray Beach, Fla., and Potomac, Md. He plays golf and bridge and is enjoying the golden years. James K. McAleer, M.D. ’63, and his wife, Sandee, have returned to northeast Ohio after 12 years in Maine, North Carolina, Florida and San Miguel de Allende, Mexico. Kids, grandkids and friends drew them back. “In January 2015, we traveled to Tanzania with our close African priest friend, Fr. Apolinary Kavische. In June, via Hearts of the World, we are planning their 46th pilgrimage, Medjugorje. Sandee is the director and has taken more than 1,000 pilgrims to the holy place in Bosnia-Herzegovina, where the Blessed Mother continues to appear to three of the six visionaries daily since
C H I R O N I A N • New York Medical College
35
1981. I am the caboose end and the finance guy,” he writes. Charles P. Cavaretta, M.D. ’61, writes he is “fully retired!...almost.” He is a volunteer instructor of clinical medicine at Texas Tech University Paul L. Foster School of Medicine and is reviving the Children’s Insights Science Center at the Old El Paso Alamo School. The original center was imploded to construct a minor league baseball stadium. Robert Kirschner, M.D. ’61, has been retired for several years. Ralph Pelligra, M.D. ’61, is chief medical officer at NASA Ames Research Center, Moffett Field, Calif. He also serves as NASA headquarters medical policy board chair, human research institutional review board chair, radiation safety committee chair, biosafety committee chair and a member of the human occupancy review board. Thaddeus (Ted) Figlock, M.D. ’60, is working at Jamaica Plain VA in Boston in the compensation and pension department as an examiner of spine and joint complaints. He passed the FCC “Amateur Extra” exam and would like to contact alumni ham radio operators and set up a field day station at NYMC.
Sanford Sherman, M.D. ’56, writes his wife, Jane, died in 2008 after returning from an African safari. She had survived a dissection of the ascending aorta three years earlier and was almost back to her old self. A mechanical mitral valve required Warfarin and her death was due to cerebral hemorrhage secondary to the anticlotting agent. “I am thoroughly retired and still attend grand rounds at USCF Benioff Children’s Hospital Oakland. I am reasonably active and healthy and I spent the Christmas holiday with my three adult offspring in Panama and I am planning a trip to Peru in July. My retinologist, Allen Z. Verne, M.D. ’71, is an alum as well so I am well cared for,” he writes. Burton Feinerman, M.D. ’54, is the holder of 16 patents for stem cell and/or gene therapy for ALS, Parkinson’s, Alzheimer’s, Multiple Sclerosis, Scleroderma, COPD, Pulmonary Fibrosis, Macular Degeneration, Kidney Disease, Diabetes, Tay Sachs, Glaucoma, Huntington, Retinitis Pigmentosa, Stargardt and Cystic Fibrosis. He will be competing against major pharmaceutical companies for developing a unique and successful therapy for Alzheimer’s using neuron stem cells and a brain reservoir. Gerald R. Frolow, M.D. ’51, writes, “I still love retirement—golfing, reading, painting, napping. Thankfully I am recovered from a number of surgeries. I still see Joe Taubman [Joseph Taubman, M.D. ’51] often.” Joseph Taubman, M.D. ’51, writes, “After 64 years of the practice of internal medicine, my wife has finally persuaded me to go into retirement this year.”
Stanley Ostern M.D. ’60, writes he is happy to reach the age of 80 and have 11 grandchildren. You can view his video “The Bunker” showing how he survived the Holocaust, hidden for two years from age 7 to 9 at www. youtube.com/watch?v=Q2PN9zRKleM.
The 50s
The 40s Wayne M. Weisner, M.D. ’48, retired in 1999 after 44 years of private practice at the age of 75. “My greatest achievement was being married for 63 years to a wonderful woman, Eugenia. We have seven children, four boys and three girls, 17 grandchildren and two great-grandchildren,” he writes.
Joan G. Easton, M.D. ’57, sends regards to her classmates. “I’m still Felix Wimpfheimer, M.D. ’45, working and enjoying it. I don’t plan retired from private practice in medito stop unless I have to. I’ve also cine on June 30, 2015. been able to do some traveling. My last trip was to Myanmar,” she writes.
36
SUMMER/ FALL 2015
IN MEMORIAM Alumni
Glenn W. Foley, M.D., Fifth Pathway ’91, died on December 3, 2013. William J. Dean III, M.D. ’88, died on May 2, 2015. Robert F. Lasting, M.D. ’84, died on October 2, 2014. He was 55. Stanley E. Caines, M.D. ’81, died on January 9, 2015. Sherwin D. Straus, M.D. ’79, died on January 29, 2015. He was 63. Kenneth L. Rothman, M.D. ’73, died on March 21, 2015. He was 67. Allen C. Marmon, M.D. ’72, died on July 2, 2014. Thomas B. Graboys, M.D. ’70, died on January 5, 2015. Dennis M. Nugent, M.D. ’69, died on February 17, 2015. Alfred N. Butner, M.D. ’65, died on November 27, 2013. Paul S. Mandala, M.D. ’63, died on November 21, 2014. Harvey Rosner, M.D. ’63, died on January 1, 2015. He was 76. Joel A. Hendler, M.D. ’62, died on February 18, 2015. Barry S. Meltzer, M.D. ’62, died on April 14, 2015. He was 78. Charles E. Jenkins, M.D. ’60, died on December 27, 2014. Robert L. McDonald, M.D. ’60, died on January 19, 2015. Andrew J. Peters, M.D. ’60, died on July 18, 2014. He was 80. Roy Stern, M.D. ’60, died on December 26, 2014. Burnell D. Stripling, M.D. ’60, died on December 19, 2014. Eugene A. Doherty, M.D. ’59, died on January 30, 2015. He was 86. Richard B. Knapp, M.D. ’59, died on November 29, 2014. He was 81. Paul A. Stavrolakes, M.D. ’59, died on March 20, 2015. He was 86. Richard H. Aubry, M.D. ’58, M.P.H., died on October 11, 2014. He was 81. Lewis A. Dalburg Jr., M.D. ’58, died on July 29, 2014. He was 84. Edwin J. Smith, M.D. ’58, died on May 18, 2015. He was 81. Vincent J. Speckhart, M.D. ’58, died on February 3, 2015. Owen E. Heninger, M.D. ’57, died on March 4, 2015. He was 85.
James J. Doheny, M.D. ’56, M.P.H., died on February 2, 2015. He was 84. Raymond C. Kinzel, M.D. ’55, died on October 10, 2014. He was 86. Michael L. Fezza, M.D. ’54, died on January 26, 2015. He was 87. Joseph A. Mangano, M.D. ’54, died on November 7, 2014. He was 86. Stephen B. Smith, M.D. ’54, died on April 19, 2015. He was 88. Joseph E. Davis, M.D. ’53, M.P.H. ’86, died on February 2, 2015. He was 84. Aaron J. Marcus, M.D. ’53, died on May 6, 2015. Edward Gerber, M.D. ’51, died on April 28, 2015. He was 91. Philip J. Landry, M.D. ’51, died on March 25, 2015. Robert L. Nutt, M.D. ’51, died on August 24, 2014. He was 92. Bramwell R. Anthony, M.D. ’50, died on September 11, 2014. He was 94. Donald J. Blodgett, M.D. ’50, died on September 18, 2014. He was 95. Hugo J. Gruendel, M.D. ’50, died on February 4, 2015. He was 88. Milton M. Zaret, M.D. ’50, died on May 29, 2012. He was 91. James E. Bowes, M.D. ’49, died on February 11, 2015. He was 94. Anthony T. Carrellas, M.D. ’49, died on December 19, 2014. He was 91. Morton Goldfarb, M.D. ’49, died on March 11, 2015. He was 88. Stanley J. Haberek, M.D. ’49, died on January 31, 2015. He was 90. Henry G. Reinhardt, M.D. ’49, died on August 10, 2014. He was 88. Joseph R. Ackerman, M.D. ’48, died on September 30, 2014. Morton Connor, M.D. ’48, died on July 13, 2014. He was 88. Frederick M. Spitzhoff Sr., M.D. ’48, died on August 5, 2014. William M. Clifford, M.D. ’47, died on January 2, 2013. He was 87. Joseph O. Pistocchi, M.D. ’47, died on May 10, 2015. He was 90. Raymond C. Fergusson, M.D. ’45, died on October 7, 2014. He was 93. J. C. Greenwald, M.D. ’45, died on August 27, 2014. He was 91. Paul J. Basirico, M.D. ’44, died on April 2, 2014. He was 93.
Marcelle B. Bernard, M.D. ’44, died on March 3, 2015. He was 94. Harry Kosovsky, M.D. ’43, died on January 16, 2015. Donald J. Stevens, M.D. ’43, died on February 9, 2015. He was 96. Carl Bornemann, M.D. ’40, died on July 19, 2013. Meyer Zodikoff, M.D. ’38, died on November 19, 2013. He was 99. Joseph A. Budetti, M.D. ’36, died on July 28, 2013. He was 102.
Alumni of NYMC Graduate Medical Education Programs Marco A. Paliotta, M.D., died on August 24, 2014. He was 49.
Faculty
William H. Beinfeld, M.D., former professor of pharmacology, died on March 28, 2014. He was 95. Philip W. Brickner, M.D., adjunct professor of medicine, died on March 24, 2014. He was 85. Vidya Bhushan Gupta, M.D., professor of clinical pediatrics, died on December 12, 2014. He was 65. Lawrence Herman, Ph.D., professor of cell biology and anatomy died on May 16, 2015. He served as chair of the Department of Cell Biology and Anatomy from 1976 to 1985. Catherine N. Hinterbuchner, M.D., professor emeritus of physical medicine and rehabilitation died on January 4, 2015. She was 88. She served as chair of the Department of Rehabilitation Medicine from 1971 to 2003. Herbert Oestreich, M.D., former associate professor of clinical neurosurgery, died on November 12, 2014. He was 82. Jerome Quint, M.D., clinical assistant professor of surgery, died on February 12, 2014. He was 77. Phoebe Saturen, M.D., retired clinical professor of physical medicine and rehabilitation and clinical professor of pediatrics, died March 19, 2015.
NYMC Mourns the Death of Susan Anderson Kline, M.D. BY ANDREA KOTT, M.P.H.
A skilled and compassionate cardiologist, a technological pioneer, an inspiring educator, incisive administrator, and yes, an accomplished sailor. That was Susan Kline, M.D., one of New York Medical College’s most beloved academic medical leaders, who passed away on March 28, 2015. “She made you feel important when you talked to her,” said Anthony M. Sozzo, M.S.Ed., M.A., associate dean for student affairs, and director of student financial planning and student activities, who worked for Dr. Kline for 22 years. “She really listened.” A native of Dallas, Tx., Dr. Kline received her undergraduate degree with highest distinction from Ohio University. She graduated first in her class from the Feinberg School of Medicine at Northwestern University, and even before finishing her residency at Case Western Reserve’s University Hospitals of Cleveland, she won numerous distinctions and awards for leadership and scholarship. Later, she completed a fellowship in cardiology at the NewYork–Presbyterian/Weill Cornell Medical Center. Dr. Kline, the vice provost for university student affairs and executive vice dean for academic affairs until her retirement in 2008, gave new meaning to ‘multi-tasking.’ When she joined the faculty in 1984 as associate professor of medicine and senior associate dean for student affairs, she immersed herself in the College, from managing medical school admissions, financial aid awards and medical education, to overseeing housing, counseling and health services. Central to students’ lives, she was a soughtafter source of guidance on curriculum, scholarships, residencies and financial planning. The numerous handbooks and bulletins she wrote have helped thousands navigate medical school. “She was very innovative,” Sozzo said. “I loved her because she would let you be as creative as you could possibly be.” In 1994, Dr. Kline was appointed interim dean of the School of Medicine and vice president for medical affairs, replacing Karl P. Adler, M.D. Although she held the post for only 18 months before Ralph A. O’Connell, M.D., took over as provost and dean, her achievements were remarkable. She appointed three department chairs, recreated one unit from the Departments of Pathology and Experimental Pathology, and strengthened relations between the College and Westchester Medical Center, among other affiliates. Two years later, Dr. Kline became executive vice dean for academic affairs and vice provost for university student affairs. A fan of technology, she ushered NYMC into the digital age by developing its first computerized student record system, and also helped implement its use of the Association of American Medical College’s Electronic Residency Application Service (ERAS®). Thanks to her, NYMC acquired Harvey, the cardiology patient simulator program in 1999. “She loved the burgeoning tech world,” Sozzo said. “She was ahead of her time.” Dr. Kline’s leadership activities and notable contributions, too numerous to mention, include her six years of service as a member of the Liaison Committee for Medical Education (LCME), her membership on the LCME’s Committee on Review Standards and her management of the intensive preparations for NYMC’s last four accreditation reviews. But she wasn’t all work and no play. In addition to being a distinguished academic medical leader and champion of students, Dr. Kline was a passionate sailor. She embraced the sport as she did her work, becoming one of the first women admitted to the Cruising Club of America in 1994. “This highly intelligent person who was a whiz in medicine would take boat engines apart or hoist a sail if you needed it,” Sozzo said. “She was as classy a professional as you could find.” At a memorial service for Dr. Kline, William H. Frishman, M.D., the Barbara and William Rosenthal Professor and Chairman of the Department of Medicine and professor of pharmacology, recalled knowing her for nearly 40 years. “We first worked together at New York Hospital-Cornell Medical Center where she was one of the first women in the country to direct a cardiac catheterization lab and she was probably the first to perform coronary angiography. I was the first fellow she trained in this new procedure,” said Dr. Frishman. “Under the intense pressure working in the lab during those early years, Susan always showed great competence, poise, equanimity and compassion. She ran the lab like a ship in a storm making sure we always got home safely. She was a wonderful bedside physician and teacher. I feel very fortunate that our paths crossed again at New York Medical College. It was my privilege and honor to have known Dr. Susan Kline.” ■ C H I R O N I A N • New York Medical College
37
Robert Small, M.D. ’77: A Caring, Compassionate Physician Who Was Everyone’s Friend BY ANDREA KOTT, M.P.H. To say that Robert Small, M.D. ’77, was a Renaissance man is to touch the tip of the iceberg. Indeed, he was a brilliant orthopedist and surgeon; an accomplished photographer, gardener and chef. But to those who lost the beloved physician, colleague, husband, father and friend to a tragic bicycle accident in July, he was more: a uniquely kindhearted and generous man; a proud and adoring husband and father; a lover of life; a friend to all. “A great man means more than just being famous,” Catherine B. Small, M.D. ’77, Dr. Small’s wife of 39 years said, quoting her husband’s partner of two decades, Paul Fragner, M.D. She added, “He treated everyone so wonderfully–patients, co-workers, lab technicians, maintenance workers and clerks. Everyone was his friend. He was a great father, friend, surgeon and doctor to everyone who loved him dearly.” Born on June 3, 1952 to the late Dr. Alan and Muriel Small of Easton, Connecticut, Dr. Small, 63, graduated from Tufts University with a major in art history. He met his wife on their first day at New York Medical College. After earning his medical degree, he trained at the country’s top orthopedic institutions. He served as chief resident at New York University’s Hospital for Joint Diseases, and completed a fellowship in hip and knee replacement at the Hospital for Special Surgery in Manhattan. For more than 30 years, Dr. Small was an orthopedic surgeon at White Plains Hospital. He was chief of its Orthopedic Institute, and president of its medical and dental staff. Raised in a family of doctors, Dr. Small took particular pride in being among four generations to have earned their medical degrees from NYMC, beginning with his grandfather, Charles Turtz, M.D. Class of 1915, and including Arnold Turtz, M.D. ’48, Allan Small, M.D. ’48, John Small, M.D. ’54, Lisa Turtz, M.D. ’85, Jeff Small, M.D. ’87, and daughter Alyson Small, M.D./M.P.H. ’15. The Smalls’ eldest daughter, Jennifer Small, M.D./Ph.D., is a second-year internal medicine resident at Columbia University Medical Center and their son William is a second-year medical student at NYU. When Dr. Small began his career, medicine was turning toward managed care. Yet, he never submitted to the growing pressure to spend less time with patients. Fiercely dedicated to every person he treated, he refused to scrimp on the time it took to provide compassionate care. “He was so giving of himself,” said his uncle, Arnold Turtz, M.D. ’48. “He treated his patients with such respect, and he didn’t just treat a bone or a ligament or a joint. He treated the whole person.”
38
SUMMER/ FALL 2015
Dr. Small was highly respected not only for his skills as a surgeon, but also for his willingness to take on difficult cases, Dr. Turtz said. “In the operating room, he was in complete command. He worked very quickly, and his patients benefited from not needing extensive anesthesia. He did amazing things.” Despite his notoriety, he was deeply humble. Everyone he worked with and knew respected him, said Catherine Small, who is an adjunct associate professor of medicine at NYMC, and the medical director of transplant/oncology and infectious diseases and director of the clinical research trials unit at NYPresbyterian/Weill-Cornell Medical Center in Manhattan. “From being a father to a surgeon to making sure everything worked in the OR, everyone trusted this man.” He had no greater love than that for his family. “No matter how busy he was as a doctor, he was there for his family,” Catherine Small said. “He never missed a football game or crew race,” she said, referring to their children’s college sports. “We flew to Washington University to see Will play in every football game.” In addition to all he did, Dr. Small found time to garden and cook gourmet meals. “It was effortless for him.” At the same time, he maintained his remarkably wry sense of humor. “He replaced my wife’s hip,” Dr. Turtz recalled, “and one day she said to him, ‘What would I ever do without you?’ He said, ‘You’d limp.’ That was Robert.” So many people attended the memorial that White Plains Hospital held for Dr. Small, that they waited in lines out the door to pay their respects, Catherine Small said. “No one realized the impact he had on the community and society because he was so humble.” She recounted a story that Laurence Smith, the chairman of the hospital’s board of directors, shared at the service: “He said he was riding the elevator, where a sign with Rob’s picture was posted, announcing the memorial. Two maintenance men were in the elevator too. One of them pointed to the picture and said to the other, ‘See that guy? He was my friend.’” ■
NEW BOARD OF ADVISORS TO GUIDE THE COLLEGE AS IT GROWS At every turn, NYMC is growing: renovating buildings, creating programs and preparing students for careers in 21st century medicine, research and public health. As part of its expansion, the College has appointed a Board of Advisors, a multidisciplinary group of alumni and friends sought for their professional expertise, leadership and support. By Andrea Kott, M.P.H.
T
he Board of Advisors, which will function cooperatively with the Board of Trustees and the Alumni Board of Governors, currently has 14 members, including alumni and business and community leaders who are addressing issues related to development, academic affairs and community engagement, says Steven Mark, interim director of Development and Alumni Relations. “There’s so much going on at the College right now, between the renovations of the Skyline and Dana Road buildings, the future dental school, and the beginning of the medical ethics program,” Mark says. “The board is a well-rounded professional group with financial and marketing experts who can help with logistics, as well as physicians who can teach students about managing their own practice.”
Currently, the Board of Advisors is making an effort to recruit younger graduates and leaders from the worlds of business and science, Dr. Vigorita says. “It is also important for students to understand the importance and joy of giving back in their professional and personal lives,” he adds. “The Board will strive to find the appropriate forum to convey that to NYMC students.” As NYMC expands and evolves, the Board of Advisors will also work to strengthen collaborations among administration, faculty, students, and alumni, says member Rebecca Marcus, M.D. ’06. “NYMC has always struck me as a particularly humanistic place, and the Board of Advisors will be an important part of maintaining the spirit of teamwork and open communication between all members of the NYMC community.” ■
Among the various tasks for the board are discussions about expanding and enhancing the wellness center available to the NYMC community, closing funding gaps for students with financial need, and teaching medical students about billing and dealing with insurance companies, says chairman Martin Katzenstein, M.D. ’78, associate professor of clinical pediatrics, and director of neonatology at NYMC-affiliate Good Samaritan Regional Medical Center in Suffern, N.Y. Member Vincent Vigorita, M.D. ’76, a private practice bone and joint pathologist who teaches NYMC’s orthopedic residents, says an important role for the board is projecting a positive image of the medical profession. “We’re living in a time when a lot of physicians are cynical about the profession, and may pass that onto young people, which is a huge mistake,” says Dr. Vigorita, whose father, John L. Vigorita, M.D. ’44, was also a College alumnus. “It’s a wonderful and enduring profession.”
From left to right: Sabra Brock, Ph.D., Stuart Paris, John Zimmerman, M.D. ‘78, Neal Mittman, M.D. ‘77, Martin Katzenstein, M.D. ‘78, Norman Maron, M.D.’70, Rebecca Newman, M.D. ‘05, Patricia White, M.D., Bill Camera, Eric Choe, M.D. ‘88 C H I R O N I A N • New York Medical College
39
GREAT THINGS ARE HAPPENING HERE
1
2
3
1
2
The Wicket Geese, NYMC’s official croquet team, made their debut at the inaugural croquet tournament on campus.
4
More than 50 members of the NYMC community, proudly sporting bright red t-shirts, joined together to raise money for the American Heart Association at the Westchester County Heart Walk. 5
3
40
NYMC was honored by the Business Council of Westchester at their annual Business Hall of Fame Gala with the Corporate Citizenship Award. Robert W. Amler, M.D., M.B.A., left, dean of the School of Health Sciences and Practice and vice president for government affairs, was proud to accept the award on behalf of NYMC from Marsha Gordon, M.B.A., D.B.A., president and chief executive officer of the Business Council of Westchester.
SUMMER/ FALL 2015
4
5
6
7
Joel Kupersmith, M.D. ’64, presented “Privacy in Genomic and Other Databases.” Robert W. Amler, M.D., M.B.A., right, dean of the School of Health Sciences and Practice and vice president of government affairs, welcomed Dr. Kupersmith and Judith Friedman Kupersmith, M.D. ’69, to campus for the special Dean’s Lecture. Faculty, administration, medical students and residents gathered for “Music, Medicine and Metropolitan,” at Metropolitan Hospital Center. Guests were enlightened by the presentation, Beethoven’s Creativity and his Deafness, by Stephen Moshman, M.D., professor of clinical medicine, and enjoyed a musical performance by a string quartet from the Conservatory of Music at SUNY Purchase.
6
7
The Class of 2017 hosted the first NYMedTalks, a one-day, interdisciplinary, interprofessional conference to expose students to topics outside of the traditional academic curriculum. The event, formerly known as Student-Physician Awareness Day (SPAD), was held in the format of “TED-style” talks and focused on the theme “Innovations in Medicine: Healthcare in Ten Years.” Six large-scale late 19th century oil paintings of NYMC’s early faculty are now on display in the lobby of the Medical Education Center. They were part of a collection that had been left at Flower and Fifth Avenue Hospital when NYMC moved to Valhalla in the 1970s. The majority of these portraits were discovered and returned to the College through the efforts of Jay Tartell, M.D. ’82, when he was a medical student. Other portraits and historic artifacts were recovered by Dr. Tartell and Edward C. Halperin, M.D., M.A., chancellor and chief executive officer in 2013 and restored with funds from the NYMC Alumni Association and Dr. Tartell.
8
9
10
11
12
13
8
9
Robert C. Seeger, M.D., center, professor, Department of Pediatrics, Keck School of Medicine of USC; section head for research, Division of Hematology, Oncology, and Blood and Marrow Transplantation Center for Cancer and Blood Diseases, Children’s Hospital Los Angeles; and director, Cancer Research Program, Children’s Hospital Los Angeles, Saban Research Institute; delivered the 16th Pediatric Cancer Research Foundation. Mitchell S. Cairo, M.D., left, professor of pediatrics, medicine, pathology, microbiology and immunology and cell biology, and PCRF President Jeffrey A. Dankberg, right, presented Dr. Seeger with a plaque. The College community was proud to show their support for Autism Awareness month in April and participate in the “Light It Up Blue” campaign to raise money for Autism Speaks.
14
10
More than 200 athletes of all ages and abilities participated in the 16th annual Race for Rehab on campus organized by Doctor of Physical Therapy (D.P.T.) students in the School of Health Sciences and Practice. The 5K race raised funds and awareness for Achilles International, a worldwide organization that aims to bring hope, inspiration and the joys of achievement to people with disabilities to promote side-by-side participation by disabled and able-bodied athletes.
12
13 11
Edward C. Halperin, M.D., M.A., chancellor and chief executive officer, displays a letter written by Charles Darwin (1809-1882) and a photo and signature from Edward Jenner (1749-1823), that were discovered in an office closet in the Administration Building. The framed letters and accompanying photographs are believed to be part of the collection of Ernst Wynder, M.D. (19221999), who founded the American Health Foundation (AHF), in 1969 to research the cause and prevention of major chronic diseases.
14
D. Douglas Miller, M.D., C.M., M.B.A., left, dean of the School of Medicine, presented the 2014 Chancellor’s Research Award, formerly the Dean’s Research Award, to Wilbert S. Aronow, M.D., professor of medicine, in recognition of his identification of the adverse effects of exposure to heavy air pollution from freeway traffic on angina pectoris and being first to describe silent myocardial ischemia. Dr. Mark Hasten, left, chairman of the Board of Trustees, and Rabbi Moshe D. Krupka, executive vice president, Touro College and University System, were on hand to celebrate the opening of the new synagogue on campus in the Alumni House. More than 1,000 guests witnessed the Class of 2019 don their white coats for the first time demonstrating their commitment to professionalism, humanism and compassion in medicine at the White Coat Ceremony. C H I R O N I A N • New York Medical College
41
NEW YORK MEDICAL COLLEGE HONOR ROLL OF DONORS For the Period from July 1, 2013 through June 30, 2015
CHANCELLOR’S CIRCLE The Chancellor’s Circle honors those who make a significant gift or commitment within a single year. In this Circle there are four Societies distinguished by the nature and size of contributions to the College.
Sunshine Cottage Society
Bryant Society
This society is comprised of donors whose gifts and commitments are $50,000 or more.
This society is comprised of donors whose gifts and commitments are $25,000 to $49,999.
Robert Alter, M.D. The Jack and Mimi Amsterdam Foundation David E. Asprinio, M.D. Mr. Gary Barnett Howard M. Baruch, M.D. Ms. Susan Bodiker James E. Carter, M.D. ’55 Evan D. Chafitz, D.M.D., D.D.S. Children’s & Women’s Physicians of Westchester, LLP Children’s Cancer Fund Ben Chouake, M.D. Gary S. Gettenberg, M.D. ’83 Dr. Mark Hasten B. H. Homan, Jr. Charitable Trust Hyundai Hope On Wheels Dr. Mervin Jacobs Drs. John and Patricia Kallis Mr. Michael Karfunkel Judith F. Kupersmith, M.D. ’69 and Joel Kupersmith, M.D. ’64 The Bernard and Dorothy Layton Foundation Joseph Levine, M.D. Ms. Shifra Lichtenstein Dr. Meryl Mark and Mr. Joseph Mark Leonard J. Newman, M.D. ’70 and Randi Newman Stephen J. Nicholas, M.D. ’86 A. Mark Novitch, M.D. ’58 Reva and Martin Oliner OvaScience, Inc. Pediatric Cancer Research Foundation Mr. Stephen Rosenberg The Louis and Rachel Rudin Foundation, Inc. Henry I. Saphier, M.D. ’61 Mr. William G. Spears The Westchester Community Foundation Renal Research Fund Joseph M. Wu, Ph.D. 42
SUMMER/ FALL 2015
Mr. William J. Camera, C.P.A. Eric I. Choe, M.D. ’88 Mr. Raymond A. Conta, J.D. Kathleen Case Finzel, M.D. ’87 Estate of Gerhard J. Haas, Ph.D. The Irving A. Hansen Memorial Foundation Martin S. Katzenstein, M.D. ’78 Mitchell G. Kirsch, M.D. ’81 The George Link, Jr. Foundation, Inc. Norman L. Maron, M.D. ’70 Neal Mittman, M.D. ’77 Sujatha Murali, M.D. ’02 NYMC Department of Neurosurgery Mr. Stuart A. Paris Estate of Louis N. Scotti, M.D. ’58 St. Joseph’s Healthcare System Jay D. Tartell, M.D. ’82 Vincent J. Vigorita, M.D. ’76 Robert A. Welke Cancer Research Foundation, Inc. Westchester Medical Center Patricia White, M.D. and Mr. Daniel Flatley John M. Zimmerman, M.D. ’78
1860 Society This society is comprised of donors whose gifts and commitments are $10,000 to $24,999. Estate of Marcelle B. Bernard, M.D. ’44 Mr. and Mrs. Ernesto Capalbo Citibank, N.A. Kaushik Das, M.D. Yvonne L. Figarella, M.D. ’95 and John M. Abrahams, M.D. ’95 Linda Friedman, Ph.D. Jill A. Gradner, M.D. ’94 and Mokarram H. Jafri, M.D. ’94 Eric B. Gurwin, M.D. ’80
Alan Hirschfeld, M.D. Dr. and Mrs. Alan Kadish Drs. Elisa and Steven Kadish James M. Katz, M.D. ’73 The Klang-Bronzo Family Robert G. Lerner, M.D. Joseph Levine, M.D. Christopher J. Linstrom, M.D. Rebecca P. Marcus, M.D. ’06 Chitti R. Moorthy, M.D. Drs. Lakshmi Murali and Raj Murali Mr. Ram Murali Mutual of America Stuart A. Newman, Ph.D. NYMC Department of Clinical Orthopaedic Surgery Dr. Ignatius J. Pappalardo Mr. and Mrs. Ronald F. Poe Mr. Lawrence Roman Seize the Ribbon STL Corporation William J. Walsh, Jr., M.D. ’64 Elias A. Zias, M.D. ’89 Anonymous
Flower and Fifth Society This society is comprised of donors whose gifts and commitments are $2,500 to $9,999 ABM Janitorial Service Nader G. Abraham, Ph.D. Dr. Kelly R. Aguilar Robert W. Amler, M.D. and Sherlita Amler, M.D. Louis V. Angioletti, Jr., M.D. ’66 Michael A. Antonelle, M.D. ’62 ArchCare Gladys M. Ayala, M.D. Hooman Azmi-Ghadimi, M.D. ’99 Robert A. Barish, M.D. ’79 Richard H. Becker, M.D. ’79 Dr. and Mrs. Francis L. Belloni Augusta H. Belmonte, M.D.
Frank Berkowitz, M.D. ’83 Ms. Sylvia Bernstein Black Box Network Services, Inc. Bleakley Platt & Schmidt, LLP Breath for Life Michael J. Bronson, M.D. ’76 Calvary Hospital Ms. Juliana Capalbo Catherine G. Caronia, M.D. ’88 and Ronald M. Caronia, M.D. ’88 Yuping Chen, M.D. and Nan Zhang, Ph.D Albina A. Claps-Paglia, M.D. ’51 Waldemar A. Comas, Esq. Michael B. Corbett, M.D. ’61 Dr. and Mrs. Alan H. Covey Estate of Mabelle A. Cremer, M.D. ’53 Imelda Cruz-Banting, M.D. Estate of Lewis A. Dalburg, Jr., M.D. ’58 Mr. Michel David-Weill Lawrence J. DeLorenzo, M.D. ’76 Mr. Thomas A. DeRosa Kent R. Duffy, M.D. Joseph F. Dursi, M.D. ’59 Mr. and Mrs. Franklin L. Earle Empire BlueCross BlueShield William J. Farr, M.D. Noreen F. Bedini Ferrante, M.D. ’84 Dr. and Mrs. Henry E. Fourcade The Freddie Mac Foundation Nancy J. Freeman, M.D. ’81 Joseph A. Gagliardi, M.D. ’86 Renee Garrick, M.D. Dr. Michael and Mrs. Judy Gewitz Jay P. Goldsmith, D.M.D. Goshen Foundation Ronald H. Hartman, M.D. ’60 Hi-Link Computer Corporation Peter Hoffmann, M.D. ’83 Charles M. Holzner, M.D. ’80 Albert L. Huber, M.D. ’57 J.P. Morgan Clearing Corporation Dr. and Mrs. Yves M. Jodesty Jean F. Jones, M.D. ’51 Harriette Kaley, Ph.D. Kelley Drye & Warren LLP Jamieson D. Kennedy, M.D. ’59 Harry D. Kerr, M.D. ’75 Mr. Brian J. Korb KPMG LLP Jules C. Ladenheim, M.D. ’47
Stanley R. Lane, M.D. ’66 Jay Y. Lee, M.D. ’86 Dr. and Mrs. Zvi Lefkovitz Dr. and Mrs. Lewis M. Levin ’71 Norman Levine, Ph.D. Jocelyn A. Luongo, M.D. ’06 Heather Lurie-Perla, M.D. and Elliott N. Perla, M.D. ’74 Peter P. Ly, M.D. ’96 Frederick MacDowell, Jr., M.D. ’53 Edgar S. Macias, M.D. William W. MacLaughlin, M.D. ’81 Camille Mallouh, M.D. Christopher T. Maloney, M.D. ’63 Manor Medical Center Gabrielle S. Marshall-Salomon, M.D. ’83 Hussein M. Matari, M.D. M. Joseph McGreevy, M.D. ’66, F.A.C.C. Robert J. McNamee, M.D. ’75 Joseph McNelis, M.D. ’87, M.P.H. ’15 Mendez Medical Center, Inc. Gerald Minkowitz, M.D. ’87 Abraham Mittelman, M.D. Estate of Laura G. Morgan, M.D. ’49 John P. Mulkern, M.D. ’91 The New York Eye and Ear Infirmary of Mount Sinai Rocco F. Noto, M.D. NPS Pharmaceuticals, Inc. NYMC Department of Clinical Dental Medicine NYMC Department of Clinical Radiation Medicine NYMC Department of Clinical Radiology NYMC Department of Dermatology/ Dr. and Mrs. Bijan Safai NYMC Department of Emergency Medicine NYMC Department of Medicine NYMC Department of Neurology NYMC Department of Neurosurgery NYMC Department of Psychiatry & Behavioral Sciences NYMC School of Medicine Alumni Association Dr. and Mrs. Ralph A. O’Connell Michael T. Oliver, M.D. ’76 D. Ryan Ormond, M.D. George F. Owens, M.D. ’79 Elaine G. Pacicco, M.D. ’85 and Thomas J. Pacicco, M.D. ’85 Dr. and Mrs. Bruce W. Peek ’82 Alan E. Peters, M.D. ’79
Phelps Memorial Hospital Center Physician Affiliate Group of New York Mr. and Mrs. Stephen Piccolo, Jr. Robert L. Pierce, M.D. ’52 Mitchell Pincus, M.D. ’53 Raymond M. Planell, Esq. John T. Repke, M.D. ’78 Richard E. Rohr, M.D. ’80 Adam D. Rubin, M.D. ’00 Sandra L. Sacks, M.D. ’97 and Harry G. Sacks, D.D.S., J.D. Saint Joseph’s Medical Center, Yonkers John A. Savino, M.D. Justin Scheer, M.D. ’50 Dr. Lester J. Schultz Memorial Fund Mr. and Mrs. Douglas W. Schutt Michal Schwartzman, Ph.D. The William and Sylvia Silberstein Foundation The Single Step Foundation, Inc. William F. Spence, M.D. ’53 John R. Stabile, M.D. ’76 David A. Staffenberg, M.D. ’89 Ms. Francine S. Stein Stifel Nicolaus & Company, Inc. Richard A. Stram, M.D. ’78 Mrs. Phyllis Tartell Ioannis Tassiulas, M.D. Estate of Roscoe W. Teahan, M.D. 1917 Mark T. Thompson, M.D. ’71 University Orthopaedics, P.C. Vifor Pharma Ltd. Mr. and Mrs. Stanley T. Wang David Werdegar, M.D. ’56 Westchester Neuroscience Research Foundation, Inc. The Whiting-Turner Contracting Company Kerri L. Wilks, M.D. ’85 Mr. and Mrs. Michael R. Williams Robert M. Yacynych, M.D. ’88 Estate of Percy C. Zanger, M.D. ’49 Anonymous (3)
C H I R O N I A N • New York Medical College
43
HONOR ROLL OF DONORS (CONTINUED) Maroon and Gold Society
Dr. Joshua Urteaga Richard B. Wu, M.D. ’05
This society is comprised of donors of $50 to $100 who are graduates of the last decade.
Generous Friends
Ms. Thamara A. Al-Shehri, M.P.H. ’13 Adriane L. Argenio, M.D. ’13 Dr. Raul Ayala Catherine C. Ayoub, D.P.T. ’12, M.P.H. ’13 Daniel A. Barone, M.D. ’06 Dr. Zakia D. Bowen, G.M.E. ’14 Giuseppe E. Capasso, Jr., M.D. ’06 Dana R. Deravin Carr, Dr.P.H. ’13, M.P.H. ’01 Jonathan C. Cheng, M.D. ’06 Allyson L. Chesebro, M.D. ’10 Eleanor Chu, M.D. ’10 Dr. Bruce M. Cohn, M.P.H. ’09 Elizabeth D. Drugge, Ph.D., M.P.H. ’12 Lauren N. Elliston, M.D. ’08 John Farrelly, D.V.M., M.S. ’10 Ms. Theresa Gelchie, M.P.H. ’06 Michael S. Graham, M.D. ’07 David N. Greenman, D.D.S., M.P.H. ’07 Dr. Daniel Handayan Izuchukwu K. Ibe, M.D. ’14 Sara A. Keck, M.D. ’06 Jonathan L. Kirsch, M.D. ’08 Agnes McNamara Lamon, M.D. ’11 Brian D. Lamon, Ph.D. ’07 Jesse A. Levin, M.D. ’09 Mr. Shun Lv, M.S. ’09 Gudrun E. Mirick, M.D. ’06 Daniel B. Morilla, M.D. ’07 Kelly A. Siano, M.D. ’11 Sara Noroozkhani, M.D. ’06 Genevieve N. Nwigwe, M.D., G.M.E. ’09 Sophia G. O’Donnell, M.D. ’08 and Seth W. O’Donnell, M.D. ’08 Christopher J. Pappas, Ph.D. ’11, M.S. ’06 Ms. Sonia Parveen, M.P.H. ’07 Patricia M. Raciti, M.D. ’11 Elizabeth Knackmuhs Revere, M.D. ’05 Mr. Jesse S. Rosenblatt, M.P.H. ’07 Changwan Ryu, M.D. ’08 Debjeet Sarkar, M.D. ’05 Michael C. Smith, M.D. ’12 Catherine M. Tegtmeier, M.P.H. ’10 Miss Kristin K. Thurlow, M.S. ’13 Angela Tong, M.D. ’12
Charles J. Abate, M.D. ’85 Abracadabra Painting Co., Inc. Linus S. Abrams, M.D. ’88 Acequia Dermatology Acute Medical, P.C. Mark K. Adler, M.D. Dr. Chisara Adonai Advanced Eye Physician, PLLC Advanced Obstetrics & Gynecology, LLC Imran H. Ahmed, M.D., M.P.H. ’87 Mr. and Mrs. Iqbal Ahmed Geraldine L. Ahneman, M.D. ’67 Ladislau Albert, Jr., M.D.
Elmer C. Arteaga, M.D. Asbestos Corporation of America Dr. Kidane H. Assefa Associated Urologists, P. A. Denis C. Astarita, M.D. ’74 Atlantic Westchester Attain Consulting Haroutiun C. Avedissian, M.D. Mark R. Axelrod, M.D. ’79 Dr. Luna D. Bailey-Riley Mr. Vlad Balaeskoul Bank of America Merrill Lynch Patricia A. Barry, M.D. ’83 and John M. Cosgrove, M.D. ’83, F.A.C.S. Hans H. Bauer, Jr., M.D. ’89 Dr. and Mrs. Howard I. Baum Martin M. Bednar, M.D. ’86, Ph.D. ’86, M.S. ’83 Thomas J. Beggins, M.D. ’84
Eric L. Albin, M.D. ’70 Joan Albin, M.D. ’67 Michael S. Alexander, M.D. ’78 Jane L. Algus, M.D. ’90 AllianceBernstein L.P. Gregory L. Almond, M.D., M.P.H. ’00, M.S. ’00 Alperson Party Rentals Richard E. Alpert, M.D. ’59 Alan R. Altman, M.D. ’71 Amertex Textile Services, Inc. David G. Anderson, M.D. ’91 David R. Andrews, M.D. ’78 Alexander Angerman, M.D. ’74 Lee M. Angioletti, Jr., M.D. ’89 Andrew N. Antoszyk, M.D. ’83 James H. Antoszyk, M.D. ’79 The AquaMarine Group, Inc. Sofia Arain, M.D. ’95 Stephan Ariyan, M.D. ’66 Ms. Ingrid C. Armstrong, M.S. ’01
Dennis G. Begos, M.D. ’90 William J. Behrje, M.D. ’65 Michael I. Belenko, M.D. ’79 The Benevity Community Impact Fund Saverio S. Bentivegna, M.D. ’50, F.A.C.S. Alan S. Berkeley, M.D. ’73 Dr. and Mrs. Robert Bernot Richard Besserman, M.D. ’64 Bethel Medical Family Practice, PC Charles C. Bianco, M.D. ’64 James M. Bianco, M.D. ’75 Barry T. Bickley, M.D. ’90 Frederick Z. Bierman, M.D. Col. Roman O. Bilynsky, M.D. ’90 BioMed Realty Trust, Inc. Nicola Bitetto, M.D. ’64 Robert V. Blake, M.D. ’75 Howard A. Blanchette, M.D. Ms. Margarita Blanter Lewis C. Blowers, M.D. ’57
44
SUMMER/ FALL 2015
$250 to $2,499
Kenneth I. Blumberg, M.D. ’86 Devon E. Bock, M.D. ’86 Richard P. Bodony, M.D. ’88 Peter N. Bogdan, M.D. ’64 Dr. and Mrs. James C. Bolz Stephen E. Borkow, M.D. ’63 Stephen Borstelmann, M.D. ’96 Mr. and Mrs. John D. Bottomley Sumankumar S. Brahmbhatt, M.D. Arnold J. Brender, M.D. ’81 Christiana Menemenlis Brenin, M.D. ’90 David R. Brenin, M.D. ’90 Joel I. Brenner, M.D. ’70 L. Paul Brief, M.D. ’64 Michael Brody, M.D. ’66 C.W. Brown Inc. Tonya M. Brown-Price, M.D. ’90 David J. Broza, M.D. ’89 Mr. and Mrs. Mark H. Bunker Ms. Estelle Burke Jerome M. Burke, M.D. ’84 Jennifer L. Burns, M.D. ’00 Andrew S. Burstiner, M.D. ’89 Robert J. Bussan, M.D. ’48 David M. Butler, M.D. ’79 Philip A. Butler, M.D. ’80 Joseph J. Calandra, M.D. ’82 Arthur Calick, M.D. ’65 Mr. and Mrs. James L. Callinan Joseph A. Camilleri, Jr., M.D. ’85 Canon Solutions America, Inc. Cantigny Research Foundation, Inc. Howard D. Cantwell, M.D. ’65 Deborah J. Millington Capilupi, M.D. ’89 and Thomas Capilupi, M.D. ’87 Edmund F. Caporaso, M.D. Joseph G. Cardinale, M.D. ’80 Care Security Systems, Inc. Maria M. Torroella Carney, M.D. ’92 Dr. and Mrs. Stephen F. Carolan ’84 John T. Carr, M.D. ’61 Robert A. Carrellas, M.D. ’89 John W. Carrier, M.D. ’51 Lyda E. Rojas Carroll, M.D. ’88 Mairead A. Carroll, Ph.D. Edward W. Carsky, M.D. ’55 Joseph P. Castellano, M.D. ’75 and Heather C. McKee, M.D. John J. Castronuovo, Jr., M.D. ’44 Saint Michael’s Medical Center Catskill Orthopedics, PC
Joseph E. Cerbone, M.D. ’82 Mark J. Cerbone, M.D. ’84 Christopher T. Channon, M.D. ’76 Michael T. Charney, M.D. ’66 Burawit B. Charuworn, M.D. ’99 Mr. Bin Chen William J. Chernack, M.D. ’70 Edward Chew, M.D. ’03 Qwie T. Chew, M.D. ’65 Children’s Health of Ocala PA Karlene M. Chin, M.D. ’81 Chinatown Kitchen of Monticello, Inc. Roger Chirurgi, M.D. Sang-Hee Choi, M.D. ’94 Ms. Annette Choolfaian, R.N. Neil T. Choplin, M.D. ’76 Shafi K. Choudhury, M.D. and Muhammad S. Choudhury, M.D. Howard N. Christ, II, M.D. ’55 Mr. and Mrs. Peter P. Chu Alfonso P. Ciarlo, M.D. ’65 Elizabeth Cirincione, M.D. ’94 Lucy A. Civitello, M.D. ’80 and Howard J. Cohen, M.D. ’81 Clancy Moving Systems Jason R. Clark, M.D. ’97 Costanza Cocilovo, M.D. ’96 Alan R. Cohen, M.D. ’73 Allan B. Cohen, M.D. ’67 Richard F. Cohen, M.D. ’90 Tony Cohen, M.D. ’66 Kenneth Cohn, M.D. ’68 Herbert L. Cole, M.D. ’54 Lewis S. Coleman, M.D. ’74 Wayne A. Colizza, M.D. John K. Conant, Jr., M.D. ’79 Dr. Patrick S. Conklin John J. Connolly, Ed.D. Alan J. Conrad, M.D. ’81, M.M.M., C.P.E, F.A.C.H.E. Dr. Mariel Harris and Dr. Daniel R. Cooperman Alan B. Copperman, M.D. ’89 Ms. Janet A. Corvini Paul F. Cotter, M.D. ’61 Elizabeth M. Craven, M.D. ’61 and Wales Craven, M.D. ’63 Mr. and Mrs. William V. Cuddy, Jr. CulinArt Inc. Curran & Connors, Inc. Custom Staffing of Westchester Rachel Cyrlak, M.D. ’81 JKB Daira, Inc. Danza Group of Paterson, LLC
David L. Feingold, Inc. Elliot Davidoff, M.D. ’71 William J. Dean, M.D. ’64 John DeAngelis, M.D. ’57 Paul S. Degenfelder, M.D. ’99 Joseph Dello Russo, M.D. ’62 Peter Demir, M.D. ’59 Ms. Dee Demling Lawrence S. Deutsch, M.D. ’71, M.S. ’66 John N. DiBella, M.D. Janet B. Dickinson, M.D. Eileen M. Dieck, M.D. ’86 and William B. Dieck, M.D. ’83 Anthony A. Diflumeri, M.D. ’65 Enzo V. DiGiacomo, M.D. ’65 Hope Dillon, M.D. ’75 Connie DiMari, M.D. and Mr. William R. Solli Mr. Jerome D’Imperio Janis DiPietro, M.D. ’79 Franklin L. DiSpaltro, M.D. ’65 Bram A. Dolcourt, M.D. ’04 Thomas E. Donnelly, M.D. ’60 Mrs. Patricia B. Doscher, R.N. ’57 and Crile Doscher, M.D. ’60 Montgomery B. Douglas, M.D. Wilmot S. Draper, M.D. ’60 Malcolm E. Drezner, M.D. ’61 Mr. and Mrs. H. E. Drugge Dryst, Inc. Andrew P. Duffy, M.D. ’87 Martin B. Duke, M.D. ’63 Dr. and Mrs. Mark A. Eberbach William A. Eddy, M.D. ’52 Christopher E. Emond, M.D. ’03 Joseph T. English, M.D. Charles W. Episalla, M.D. ’88, M.S. ’87 Majid Eshghi, M.D. Behruz Eslami, M.S. ’83, Ph.D. ’84 William J. Esposito, M.D. ’54 John S. Ettenson, M.D. ’83 The Eye Clinic, LLC Robert E. Fabricant, M.D. ’60 Dr. and Mrs. John T. Fallon, III Joseph J. Fay, M.D. ’68 John M. Feder, M.D. ’87 Kalmen A. Feinberg, M.D. ’64 Michael J. Feinstein, M.D. ’64 Dr. Alexander Ferenczy, III Mr. and Mrs. Robert C. Ferguson David H. Fields, M.D. ’73 Ilona W. Figura, M.D. ’83 Stanley P. Filewicz, M.D. ’59
Burton M. Fink, M.D. ’71 Ms. Barbara Flasch Floorcraft Marie L. Foegh, M.D. Eric C. Fok, M.D. ’93 Foley Graphic Center, Inc. A. P. Fontanetta, M.D. ’73 Denis J. Frank, M.D. ’71 Bruce I. Friedman, M.D. ’79 Dr. and Mrs. Bruce J. Friedman ’76 Mark J. Friedman, M.D. ’71 Steven I. Friedman, M.D. ’76 Dr. William and Mrs. Esther Frishman Mr. and Mrs. Robert J. Fruggiero Fred D. Fumia, M.D. ’75 Frank M. Galioto, Jr., M.D. ’68 Donna M. Gallagher, M.D. ’89 Peter A. Galvin, M.D. ’80 Garrie Pest Control Michael R. Gatto, M.D. ’76 Francis J. Geary, M.D. ’64 Harris J. Gelberg, M.D. ’73 Steven J. Gerschultz, M.D. ’89 Theodore Giannaris, M.D. Dr. Elsa-Grace Giardina and Dr. Alan L. Saroff Lucille P. Taverna Giardina, M.D. ’71 James M. Gibbons, Jr., M.D. ’58 Elyse W. Glaser, M.D. David J. Glass, M.D. ’85 J. Peter Glass, M.D. ’72 Irving Glassman, M.D. ’51 Cary D. Glastein, M.D. ’79 GNYHA Ventures, Inc. Albert C. Goldberg, M.D. ’63 Laurence D. Goldstein, M.D. ’84 Paul Goldstein, M.D. ’71 Carey S. Goltzman, M.D. Angela E. Gonzalez, M.D. ’94 Arnold P. Good, M.D. ’85 Bradley J. Gordon, M.D. Donald L. Gordon, M.D. ’47 Virginia A. Gortych-Barnes, M.D. ’87 Ira A. Gould, M.D. ’64 Arun Goyal, M.D. ’90 Graphic Management Partners LLC Gina M. Greco-Tartaglia, M.D. ’91 Lawrence J. Green, M.D. ’89 Robert D. Green, M.D. ’61 Stuart A. Green, M.D. ’67 Joel G. Greenspan, M.D. ’74 J. C. Greenwald, M.D. ’45+ Gabriel Gregoratos, M.D. ’54
Richard H. Greif, M.D. ’75 Karen E. Grimmell, M.D. ’61 David J. Gross, M.D. ’84 and Maria Gross Anita Grover, M.D. ’78 Jin Li, M.D., Ph.D. ’01 and Gary Guo, M.D., Ph.D. Dr. Naushaba S. Habib Daniel S. Haddad, M.D. ’83 Dr. Ronald J. and Mrs. Maria+ Hagadus Itzhak C. Haimovic, M.D. ’75 Jerome C. Hall, M.D. ’90 Suelyn D. Hall-Harper, M.D. ’91 and Douglas M. Harper, M.D. ’92 Edward C. Halperin, M.D., M.A. Jennifer J. Halstead-Kenny, M.D. ’03 and John M. Kenny, M.D. ’01 Naomi R. Ham, M.D. ’84 and Elmer C. Agustin, M.D., M.P.H. ’15 Irwin Hametz, M.D. ’73 Paul A. Hanna, M.D. ’94 Eastlyn E. Harding-Marin, M.D. Harquin Creative Group Leonard R. Harrison, M.D. ’64 Robert A. Harwood, M.D. ’62 Walter H. Hasbrouck, M.D. ’55 Jennifer and Marc Bernstein John J. Healy, M.D. ’63 Edward L. Hedaya, M.D. ’81 Kathleen A. Heffernan, M.D. ’81 Edward R. Heilman, M.D. ’74 Paul B. Heller, M.D. ’68 Hempstead Funeral Home Robert M. Herenstein, M.D. ’85 L. S. Herman, M.D. ’74 Robert A. Herzlinger, M.D. ’69 William H. Hewes, M.D. ’41+ CAPT Deborah Ann Hinkley, USN, M.D. ’89 Hinman Straub, P.C. Thomas H. Hintze, Ph.D. ’80, M.S. ’78 Robert D. Hirsch, M.D. ’61 Richard N. Hirsh, M.D. ’69 Barbara M. Hisler, M.D. ’83 Kevin M. Holcomb, M.D. ’92 Rivka S. Horowitz, M.D. ’78, Ph.D. Stephen K. Hoverman, M.D. ’78 Howard Jay Kline, M.D. Mr. and Mrs. Irwin Hu Dr. Gustave Huber Hudson Valley Economic Development Corporation Magdalen E. Hull, M.D. ’79, M.P.H.
C H I R O N I A N • New York Medical College
45
HONOR ROLL OF DONORS (CONTINUED) Michael J. Hutzler, M.D. ’97 Mr. John A. Imbiano, A.S.L.A. John D. Imig, Ph.D. Immunom Technologies, Inc. Mario A. Inchiosa, Jr., Ph.D. Institute for Systems Biology IQ Landscape Architects, P.C. Norman J. Isaacs, M.D. ’54 William H. Isacoff, M.D. ’70 Lori A. Iurato-Barazani, M.D. ’86 and Lance A. Barazani, M.D. ’86 J&R Tours, Ltd. Parvin M. Jacobs, M.D. ’55 Mr. and Mrs. Jeffrey Jacobson Ms. Patricia James-Sommer David Janeway, D.O. Amballur D. John, M.D. ’90 Heather D. Johnson, M.D. ’02 and John P. Magnan, M.D. ’02 Erica C. Jones, M.D. ’92 Edward F. Jordan, M.D. ’72 Frank T. Jordan, M.D. ’71 Grace G. Jorgensen, M.D. ’54 Ms. Marie E. Josma Kenneth B. Juechter, M.D. ’68 Fern R. Juster, M.D. Jonathan M. Kagan, M.D. ’69 Samuel D. Kahnowitz, M.D. ’76 Lawrence S. Kaminsky, M.D. ’78 Sari Kaminsky, M.D. and Eric C. Rackow, M.D. Robert J. Kane, M.D. ’65 Mr. Seymour Kaplan Mr. Yutaka Kasai Jawad Kassem, M.D. Kenneth G. Kasses, Ph.D. ’74 Aaron E. Katz, M.D. ’86 Kaufman Borgeest & Ryan LLP Stephen Z. Kaufman, M.D. ’65 Eugene L. Kavanagh, M.D. ’74 John J. Kearney, M.D. ’63 George D. Keckeisen, M.D. ’81 Daniel Kenigsberg, M.D. ’78 The Kensico Cemetery Barry R. Kent, M.D. ’67 John G. Ketterer, Jr., M.D. ’61 Mr. and Mrs. Richard J. Keyes, Jr. Kenneth Khaw, M.D. ’88 Mr. and Mrs. Sung-Hyun Kim Joseph A. King, M.D. ’47 Jack J. Kleid, M.D. ’65 46
SUMMER/ FALL 2015
Alan M. Klein, M.D. ’71 Steven D. Klein, M.D. ’98 Howard J. Kline, M.D. ’58, F.A.C.C. Jeffrey Kluger, M.D. ’71 Gary G. Knackmuhs, M.D. ’76 Peter A. Knight, M.D. ’80 Jennifer Koestler, M.D. Behnam Kohanim, M.D. ’90 Drs. Phillip Kohanski ’87 and Renee Kohanski ’90 Orest J. Kozicky, M.D. ’81 Rosemary Kraemer, Ph.D. ’90 Mitchell S. Kramer, M.D. ’85 Leonard B. Krich, M.D. ’65 Mark A. Krich, M.D. ’97 Paul E. Krochmal, M.D. ’75 Linda S. Krook, M.D. ’78 Keith A. Kurland, M.D. ’79 Michael V. Kurzawa, M.D. ’85 Annette E. Kussmaul, M.D. ’93 Gina S. Kwak-Rabin, M.D. ’90 and Glenn E. Rabin, M.D. ’90 KYA Construction Corp. L.J. Coppola Inc. Catherine C. Labiak-Maher, M.D. ’82 and James O. Maher, III, M.D. ’82 Edmund F. La Gamma, M.D. ’76 Col. and Mrs. Daniel F. Lally Mrs. Frances Lamer Mr. and Mrs. Howard Lander Jodi D. Langer, M.D. Nicholas F. LaRusso, M.D. ’69 Kameran Lashkari, M.D. ’85 Mrs. Lorraine Lasker Nechama Lasser-Ross, Ph.D. and William N. Ross, Ph.D. Ferdinand LaVenuta, M.D. ’63 Nancy P. Lawless, M.D. ’89 Donald P. Lawrence, M.D. ’66 Linda F. Lazar, M.D. and Rande H. Lazar, M.D. James B. Leach, M.D. ’56 Edward Lebovics, M.D. Jack C. Lee, M.D. ’65 Dr. May Lee Robert C. Lee, M.D. ’88 Simon X. Lee, M.D. Louis H. Lefkowitz, M.D. ’64, F.A.C.O.G., F.A.C.S. Christopher S. Leonard, Ph.D. Alan M. Lesselroth, M.D. ’70 Stuart D. Lestch, M.D. ’66
Mrs. Diane L. Levere Aleksandr Levin, M.D. Elliot M. Levine, M.D. ’91 Jerry I. Levine, M.D. ’77 Richard H. Levine, M.D. ’80 Peter D. Levit, M.D. ’76 Mr. and Mrs. Paul H. Lewis Walter M. Lewis, M.D. ’91 Naixi Li, M.D., Ph.D. ’98 and Xin Quan, M.D. Leslie LiDonnici, M.D. ’78 Mr. Michael Liebeskind Robert Y. Lin, M.D., M.S. ’92 Richard W. Lindsay, M.D. ’60 Janet C. Lin-Torre, M.D. ’85 Lion Medical PC Mr. Percival D. Liongson LM Electric, Inc. Joseph K. Lobl, M.D. ’82 Charles Lomanto, M.D. ’63 Eduardo Lopez, M.D. Dr. Gladys H. Lopez Rene I. Lopez, Jr., M.D. Francis C. Losito, M.D. ’64 Peter A. Loud, M.D. ’89 Jacquelyn S. Loughlin, M.D. ’75 Grace M. Lozinski, M.D. ’00 Peter J. Lucas, M.D. ’72 Robert Ludemann, M.D., Ph.D. Maja L. Lundborg-Gray, M.D. ’95 and Daniel S. Gray, M.D. ’91 George W. Lutz, M.D. ’61 Luvly Enterprises John J. Lynch, M.D. ’58 Vincent A. Lynch, M.D. ’67 George D. Lyons, M.D. ’92 Barbara G. Mackintosh, M.D. ’81 Francis P. MacMillan, M.D. ’64 Anthony V. Maddalo, M.D. ’81 Gregory H. Mahairas, M.D. ’59 Jean M. Cacciabaudo, M.D. ’90 and William A. Maiorino, M.D. ’89 Andrea G. Maitlin-Katz, M.D. ’88 Michael J. Majsak, P.T., Ed.D. Frank P. Maldonado, M.D. ’64 Bella Mikhailova Malits, M.D. ’90 Albert J. Mariani, M.D. ’75 Ada M. Marin, M.D. ’83, M.P.H. The Marino Organization, Inc. Craig W. Markert, M.D. ’73 Alan B. Marks, M.D. ’78
Jon O. Marks, M.D. ’76 Clifford L. Marshall, M.D. ’77 Jeffrey S. Mason, M.D. ’75 Raymond J. Mastrovito, M.D. ’74 Stanley J. Mathew, M.D. Jeffrey S. Matican, M.D. ’82 Matthew & Tony General Landscaping, Inc. Paul A. Maxwell, M.D. ’70 James T. Mazzara, M.D. ’63 Richard G. McCarrick, M.D. Sarah M. McGee, M.D. ’83 and William T. McGee, M.D. ’83 Kathryn E. McGoldrick, M.D. and Jonathan Mardirossian, M.D. James F. McGroarty, M.D. ’68 Peter P. McKellar, M.D. ’70 George R. McKendall, M.D. ’84 Mr. and Mrs. Thomas A. Mehuron Martin K. Melman, M.D. ’74 Morton Meltzer, M.D. ’65 Ana T. Menendez-Tuckman, Ph.D. ’96, M.S. ’96 and Ronald Tuckman John H. Mensher, M.D. ’67 Metropolitan Medical & Rehab Burt R. Meyers, M.D. Monica Y. Michell, M.D. ’82 Harold Michlewitz, M.D. ’71 Philip A. Miles, M.D. ’64 Samuel I. Miles, M.D. ’74 Millennium Medical and Rehab P.C. Bruce A. Miller, M.D. ’67 James L. Mills, M.D. ’73 Jeffrey H. Minassian, M.D. ’79 Mintz, Levin, Cohn, Ferris, Glovsky and Popeo, P.C. Michael A. Miranda, M.D. ’92 Stephen T. Moffitt, M.D. ’88 Mogul Contracting, Inc. George R. Monahan, M.D. ’57 James P. Mooney, M.D. ’56 Carver L. Moosman, M.D. ’51 Mrs. Miriam K. Moran Dan K. Morhaim, M.D. ’75 Edward N. Moss, M.D. ’76 Michael M. Moss, M.D. ’64 William C. Mulford, M.D. ’58 Michelle A. Multz, M.D. ’87 James J. Murdocco, M.D. ’65 Kenneth E. Murdock, M.D. ’68 Richard E. Murphy, M.D. ’61 Eric Mustonen, M.D. ’75
Paula M. Muto, M.D. ’89 and Jonathan K. Gordon, M.D. ’89 Adelaide G. Nardone, M.D. ’83 Nature Spine & Joint Care LLC Dr. Ernesto Navarro Jack Needleman, M.D. ’74 Steven I. Neibart, M.D. ’81 Kathleen G. Nelson, M.D. ’71 Mario Nelson, M.D. New York College of Podiatric Medicine Ms. Sum Yee Wang and Mr. Daoshing Ni Mr. Andreas Niens George A. Nikias, M.D. ’89 John J. Novello, M.D. ’76 Ms. Elsa I. Nunez Nkemdilim N. Nwosa, M.D. ’99 NYMC Department of Cell Biology and Anatomy NYMC Department of Ophthalmology NYMC Department of Physical Medicine and Rehabilitation OB GYN Associates Stephen A. Obstbaum, M.D. ’67 Mary Alice O’Dowd, M.D. ’76 Dr. Christopher N. Okonkwo Uchenna A. Okoronkwo II, M.D. OLA Consulting Engineers, PC Omega Environmental Services Nancy L. Oplinger, M.D. ’91 Deirdre A. O’Reilly, M.D. ’95 John P. O’Reilly, M.D. ’61 Otolaryngology Consultants of Memphis Dr. Tamas Otrok Douglas E. Padgett, M.D. ’82 Patrick J. Pagano, Ph.D. ’91 David M. Paige, M.D. ’64 Carrie A. Palmer, M.D. ’04 Carol A. Palmieri, M.D. ’92 Dr. Scott M. Palyo Robert D. Pane, M.D. ’74 Philip A. Passalaqua, M.D. ’64 Richard S. Pataki, M.D. ’62 Mrugesh Patel, M.D. ’91, Ph.D. ’91 Thomas R. Patnaude, M.D. ’74 Mr. David D. Patterson Kevin L. Pehr, M.D. ’81 Robert A. Peinert, M.D. ’70 Thomas E. Pellechi, M.D. ’96 Myles L. Pensak, M.D. ’78 Jason R. Penzer, M.D., J.D. Mark A. Perazella, M.D. ’88 Richard D. Perera, M.D. ’58
John R. Person, M.D. ’73 Dr. Muhammad A. Pervaiz Pfizer Foundation Matching Gifts Program Joseph D. Pham, M.D. ’90 Dr. and Mrs. Donald C. Phillibert V. Rachel Phillips, M.D. ’79 Mrs. Teletta A. Piper Joseph O. Piscetta, M.D. ’46 Francis J. Pizzi, M.D. ’69 Anna M. Plichta, M.D. Mitchell C. Pollack, M.D. ’77+ Bernard J. Powers, M.D. ’76 John M. Powers, M.D. ’77 Glenn M. Preminger, M.D. ’77 Louise M. Priolo-Grecco, M.D. ’87 John L. Prue, M.D. ’74 PS&S LLC Vivek J. Puppala, M.D. ’04
Renee Z. Rinaldi, M.D. ’76 Albert W. Ritter, M.D. ’92 RK Psychology Associates, LLC James P. Roach, M.D. ’58 Barry S. Robbins, M.D. ’73 Janine O. Robertson, M.D. ’49 Paul E. Rodriguez, M.D. ’65 Neil M. Rofsky, M.D. ’85 Nancy C. Rose, M.D. ’84 and G. Marc Jackson, M.D. Richard J. Rose, M.D. ’64 Stephanie L. Rosen, M.D. ’93 and Barney H. Rosen, M.D. ’93 Howard D. Rosenberg, M.D. ’76 Ms. Alice J. Brody and Mr. Ronald S. Ross Andrew J. Roth, M.D. ’88 Barbara K. Roth, M.D. ’75 Richard Rovit, M.D.
Quality Living Liaisons, LLC David and Leah Raab Joseph P. Rafferty Jr., M.D. ’87 Laurence M. Raiford, M.D. ’77 Srinivas Rajamahanty, M.D. Audrey L. Randolph, M.D. Dr. Sanjay D. Rao Sudhamani R. Rao, M.D. and Sateesh C. Babu, M.D. RCK Basketball Booster Ms. Larissa F. Reece Dr. Donald R. Reeves, Jr. Sarah L. Reid, Esq. Robert P. Reisman, M.D. ’78 Maureen A. Relland, M.D. ’64 and Robert R. Riggio, M.D. ’58 Mr. Robert M. Rene Robert D. Restuccia, M.D. ’72 Andrew Ricci, Jr., M.D. ’77 Charles R. Rich, M.D. ’74 Alfonso Richards, M.D. ’56, F.A.C.S. Elisabeth J. Wilder Richards, M.D. ’91 Beverly L. Richman, M.D. ’64 Fay H. Rim, M.D. ’02
Maureen and Joe Roxe, The Roxe Foundation Jack M. Rubenstein, M.D. ’76 Audrey and Samuel H. Rubin, M.D. Ronald B. Rudlin, M.D. ’64 Charles J. Ruotolo, M.D. ’95 Jeffrey M. Rusheen, M.D. Stephen D. Ryan, M.D. ’90 Scott R. Saffran, M.D. ’87 Saint Michael’s Medical Center Paul Sakiewicz, M.D. Stanley R. Sakowitz, M.D. ’62 Shirley U. Salvatore, M.D. ’87 and James A. Salvatore, M.D. ’87 Emanuel Salzman, M.D. ’43 San Diego Heart & Medical Clinic, Inc. San Sebastian Enterprise Ltd. Betty Sanchez-Catanese, M.D. ’83 and Anthony J. Catanese, M.D. ’83 Robert S. Sanford, M.D. ’64 Sanofi-Aventis Sidney A. Sass Associates, Inc. Mrs. Anne R. Sawyer Donald E. Sawyer, M.D. ’70
Dr. Robin M. Scarlata Lawrence S. Schechter, M.D. ’66 Theodore J. Schmahai, Ph.D. ’88 Kenneth B. Schnide, M.D. ’82 Steven L. Schoenfeld, M.D. ’83 Henry G. Schriever, M.D. ’60 Melvin L. Schulman, M.D. ’65 David Schwalb, M.D. ’84 Aaron M. Schwartz, M.D. ’50 Ira S. Schwartz, Ph.D. Jerold Schwartz, M.D. ’56 Lee S. Schwartzberg, M.D. ’80 Ms. Veronica Scianna Maria G. Scunziano-Singh, M.D. ’93 Frederick B. Seley, M.D. ’64 Deborah A. Shapiro, M.D. ’89 and Alan R. Plumer, M.D. ’88 Gabrielle L. Shapiro, M.D. ’90 Jerome R. Shapiro, M.D. ’61 Moira Shea, M.D. ’79 and William J. Wittman, M.D. ’79 John P. Sheehy, M.D. ’75 Win Shen, M.D. ’83 Bruce E. Sherling, M.D. ’73 Sanford Sherman, M.D. ’56 Dr. Sandra Shivers and Mr. Jed M. Shivers Tighe P. Shomer, M.D. ’77 Joanna F. Shulman, M.D. ’80 The Sigmund Foundation Mark D. Siletchnik, M.D. ’75 Jeffrey E. Silverstein, M.D. ’91 Simotas Property Management LLC Athos Simotas, M.D. ’58 Simpson Gumpertz & Heger, Inc. Tej-Preet Singh, M.D. ’01 Catherine B. Small, M.D. ’77 and Robert D. Small, M.D. ’77+ David L. Smith, M.D. ’61 Gary M. Snyder, M.D. ’79 John L. Soelling, M.D. ’46 Mrs. Shirley W. Somers Barbara R. Sommer, M.D. ’79 Jonathan E. Sonne, M.D. ’98 Gary Stallings, II, M.D., M.P.H. Ms. Elisabeth Stamm David J. States, M.D. ’53 Mr. William A. Steadman, II, M.A. Paul Stefek, M.D. ’81 Frederick Steinberg, M.D. ’58 John T. Stinson, M.D. ’75 John L. Stoneham III, M.D. ’88 Rev. Ruth H. Strang, M.D. ’49 Suburban Carting Corporation
C H I R O N I A N • New York Medical College
47
HONOR ROLL OF DONORS (CONTINUED) Joyce M. Sudeall-Blackwood, M.D. ’74 Elizabeth L. Supra-Johnson, M.D. ’88 and Joseph A. Johnson, M.D. ’88 Deon K. Sutherland, M.D. ’02 Svigals + Partners, LLP Ross H. Taff, M.D. ’74 Michael G. Tager, M.D. ’58 Patricia Tager, M.D. Dr. Mitchell K. Taguchi Lindsay S. Tan, M.D. ’82 Marvin B. Tankel, M.D. ’80 Robin J. Tapper, M.D. ’84 Joseph J. Tartaglia, M.D. David B. Tashjian, M.D. ’96 Philip G. Taylor, M.D. ’64 Loretta A. Terranova, M.D. ’80 Dr. and Mrs. Sanjay P. Thakur This Close for Cancer Research, Inc. Yvonne S. Thornton, M.D., M.P.H. Dr. Khin M. Thu Raj K. Tiwari, Ph.D. David A. Tompkins, M.D. ’04 Joy T. Torakawa, M.D. Joseph M. Torruella, M.D. ’56 James P. Tracey, M.D. ’89 Tri-County Orthopaedic and Sport Medicine, PA James N. Trone, M.D. ’55+ Charlotte L. Tsai, M.D. ’01 and Danny W. Hsia, M.D. ’01 Dr. Nancy N. Tsai Oya Tugal, M.D. Elisabeth F. Turnauer, M.D. ’52 Arnold I. Turtz, M.D. ’48 Urologic Cancer Research Institute LLC Edward S. Valentine, M.D. ’78 Scott K. Varland, D.D.S. Lisa T. Vasak, M.D. ’92 Pierre A. Vauthy, M.D. ’72 Joseph S. Vetrano, M.D. ’70 Diodato Villamena, M.D. ’71 Lidia F. Vitale, M.D. ’90 Jack H. Vitenson, M.D. ’65 Susan L. Vogel, M.D. ’76 Mr. and Mrs. Henry Vong James A. Walker, M.D. ’61 Ilisa D. Wallach, M.D. ’87 and Meir Salama, M.D. ’87 Marc K. Wallack, M.D. Joseph B. Walsh, M.D. Anna M. Ward, M.D. ’85
48
SUMMER/ FALL 2015
Thelma G. Warshaw, M.D. ’47, F.A.A.D. Watchung Pediatrics Ben C. Watson, Ph.D. Wayne Radiology Associates, LLC Thomas G. Webber, M.D. ’73 Xiaofang Wei, M.D. Ruth H. Weichsel-Hoffman, M.D. ’65 Steven Weinstock, M.D. ’74 Lori Anne Weir, M.D. ’99, M.P.H. ’09 Tedd L. Weisman, M.D. ’84 Wayne M. Weisner, M.D. ’48 Mr. Steven M. Weiss William R. Weissman, M.D. ’65 Jerrold L. Wheaton, M.D. ’47
Xiaomei Zeng, M.D. ’93 Yinggang Zheng, M.D. Barry M. Zisholtz, M.D. ’83 Robert C. Zoller, M.D. ’77 Dr. and Mrs. Michael A. Zullo
Legacy Society The Legacy Society recognizes donors who have made provisions for the College in their wills or through other planned gifts. Michael S. Alexander, M.D. ’78 Doris Bate, M.D. ’50 Augusta H. Belmonte, M.D.
Mrs. Dorothy Mehta James J. Murdocco, M.D. ’65 Mary Alice O’Dowd, M.D. ’76 Guy R. Orangio, M.D. ’79 and Mrs. Patricia Orangio Christopher J. Pappas, Ph.D. ’11, M.S. ’06 Lee J. Phillips, M.D. ’85 John H. Seward, M.D. ’61 Neil S. Silber, M.D. ’75 Theresa A. Smith, M.D. ’56 Rev. Ruth H. Strang, M.D. ’49 Jay H. Stubenhaus, M.D. ’47 Joyce M. Sudeall-Blackwood, M.D. ’74
Tributes and Memorials In memory of Joseph C. Alfenito, M.D. ’47 John F. McCabe, M.D. ’47 In memory of Harry Allen, M.D. ’56 Mrs. Daphine M. Allen In memory of Sgt. John E. Allen Debjeet Sarkar, M.D. ’05 In honor of Dr. Paterno Almendral Dante F. Almendral, M.D. ’90, M.P.H. ’90
Harvey L. White, M.D. ’64 Mr. Roger Williams Myra Wise, Ph.D. and Burton L. Wise, M.D. ’47 Barry R. Witt, M.D. ’84 James J. Y. Wong, M.D. ’76 Douglas A. Woodburn, M.D. ’83 Worcester Internal Medicine, Inc. Gary P. Wormser, M.D. Mrs. Cassandra Wry Tin Tin Wynn, M.D. Dr. Wen Xiong, M.S. ’01 Dr. and Mrs. Vincent J. Yakavonis ’77 Mr. Bor-lin Yao and Ms. Shii-Ben Liaw Mr. and Mrs. Timothy H. Yau Dr. and Mrs. Jae W. Yoon Cecelia A. Young, M.D. ’59 David H. Young, M.D. ’72 Dr. Brikti G. Ytbarek Peter T. Zacharia, M.D. ’88 Reinhard Zachrau, M.D. Gerald W. Zaidman, M.D. Joseph J. Zaladonis, Jr., M.D. Donna A. Zeide, M.D. Carl Zeiss Microscopy, LLC
Douglas M. Berger, M.D. ’85 Robert V. Blake, M.D. ’75 Marshall B. Block, M.D. ’68 Mrs. Dale Block Alan D. Dauer, M.D. ’62 Morris A. Diamant, M.D. ’78 Harriet E. Dickenson, M.D. ’82 Theodore Diktaban, M.D. ’76 Emalie and John Feerick Stanley P. Filewicz, M.D. ’59 Francis J. Geary, M.D. ’64 Arthur Ginsburg, M.D. ’58 Dr. Ronald Hagadus Howard D. Harrison, M.D. ’61 John F. Hoell, M.D. ’60 Dr.+ and Mrs. Henry V. Kogut ’43 Bradley S. and Ruth Friedman Kuhn Judith F. Kupersmith, M.D. ’69 and Joel Kupersmith, M.D. ’64 Mrs. Diane L. Levere S. R. Mackay, M.D. ’57 Camille Mallouh, M.D. Carl M. Marchetti, M.D. ’60 Edmund D. Marinucci, M.D. ’44 Ariz R. Mehta, M.D. ’03
In memory of Ruth and Boots Almond Gregory L. Almond, M.D., M.P.H. ’00, M.S. ’00 In honor of Ali and Mary Ann AlShehri Ms. Thamara A. AlShehri, M.P.H. ’13 In memory of William S. Anapoell, M.D. Mark F. Anapoell, M.D. ’57 In memory of Ronald H. Anderson David G. Anderson, M.D. ’91 In memory of Louis V. Angioletti, M.D. ’38 Louis V. Angioletti, Jr., M.D. ’66 In memory of James P. Angiulo, M.D. ’72 Robert D. Restuccia, M.D. ’72 In memory of Nicholas Antoszyk, M.D. ’48 Andrew N. Antoszyk, M.D. ’83 James H. Antoszyk, M.D. ’79 In memory of Sanford H. Anzel, M.D. ’54 Mrs. Darlene Anzel In memory of Dr. Zalmen A. Arlin This Close for Cancer Research, Inc. In memory of Zinaida Ilyasova Bella Mikhailova Malits, M.D. ’90
In memory of Bernie and Min Barish Robert A. Barish, M.D. ’79 In honor of Patrick and Susan Barone Daniel A. Barone, M.D. ’06 In honor of Harry C. Barrett, D.Min., M.P.H. Geraldine L. Ahneman, M.D. ’67 In memory of Morris L. Bass, M.D. ’43 Mrs. Marilyn Bass In memory of Marilyn Batterman Amy BattermanDitchek, M.D. ’83 In honor of Ira Bedzow, Ph.D. Richard A. Stram, M.D. ’78 In memory of Francis P. and Frances Belloni Dr. and Mrs. Francis L. Belloni In honor of Saverio S. Bentivegna, M.D. ’50, F.A.C.S. Dr. Kelly R. Aguilar William R. Bungarz, M.D. Christian Caicedo, M.D. Joseph G. Cardinale, M.D. ’80 Dr. Patrick S. Conklin Charles E. Dorfman, M.D. Fred B. Ginsberg, M.D. Frank D. Iuliano, M.D. Dr. Rongjie Jiang Linda F. Lazar, M.D. and Rande H. Lazar, M.D. Dr. Gustavo A. Morales Paul Sakiewicz, M.D. Patrick J. Sciortino, M.D. R. Scott Snyder, M.D. Dr. Joshua Urteaga In memory of Lillian Bigman Jeff S. Silber, M.D. ’95 In memory of Darlene Biolo Mark A. Perazella, M.D. ’88 In memory of George Black John M. Zimmerman, M.D. ’78 In memory of Maurice “Sonny” Black John M. Zimmerman, M.D. ’78 In memory of Joseph and Josephine Bober Nancy B. Holyst, M.D. ’88 In memory of Libby E. Bogel, M.D. ’78 Andrew M. Murphy, M.D. ’78 In memory of Joyce Bonder Michael I. Bonder, M.D. ’70 In memory of Robert Bonder Michael I. Bonder, M.D. ’70 In honor of Claire E. Bottomley, M.D. ’14 Mr. and Mrs. John D. Bottomley In memory of Joan Brakeley JKB Daira, Inc. In memory of Joel Brander This Close for Cancer Research, Inc. In memory of Brooke L. Brennan, M.D. ’01 Zachary M. Campbell, M.D. ’01 In celebration of the 81st birthday of Paul H. Brenner, M.D. ’61 Ms. Sybil Bernstein In memory of Eleanor Brooks Sharon and Edward Halperin Elizabeth and Alan Reznik
In memory of William E. Brown II and Mattie M. Brown Tonya M. BrownPrice, M.D. ’90 In memory of John Joseph Broza David J. Broza, M.D. ’89 In honor of David J. Burke, M.D. ’86 and Gordon M. Burke, M.D. ’11 Ms. Estelle Burke In honor of Howard S. Bush, M.D. ’82 Mrs. Patricia B. Doscher, R.N. ’57 and Crile Doscher, M.D. ’60 In memory of Stanley Butler, M.D. ’52 Mrs. Jessie Butler In memory of John L. Capalbo, M.D. ’41 Andrea J. Capalbo, M.D. ’81 In honor of James R. Cassuto Mrs. Irene Cassuto In memory of Jean Castiglione Mr. Anthony J. Castiglione In memory of John A. Chadbourn, M.D. Justin M. Segraves, M.D. ’14 In honor of Delroy Chang Karlene M. Chin, M.D. ’81 In honor of Scarlet and Penelope Chew Qwie T. Chew, M.D. ’65 In memory of Enzo Chirurgi Roger Chirurgi, M.D. In honor of Annette Choolfaian, R.N. David N. Greenman, D.D.S., M.P.H. ’07
In memory of Irvin P. DeStefano, M.D. Rocco F. Noto, M.D. In memory of Matthew DiBiase, M.D. George M. Arcieri, M.D. ’64 In memory of Susan M. DiFabio Dominick F. DiFabio, M.D. ’71 In memory of Joseph DiQuattro The DiQuattro Family In memory of Anthony Peter Ditaranto Anthony V. Ditaranto, M.D. ’72 In honor of Jay D. Draoua, M.D. Jonathan L. Kirsch, M.D. ’08 In honor of Elizabeth Drugge, Ph.D., M.P.H. ’12 and Rhett J. Drugge, M.D. ’88 Mr. and Mrs. H. E. Drugge In memory of Marion Golden Dubin Carey S. Goltzman, M.D. In memory of William and Mary Dugan Paul F. Cotter, M.D. ’61 In memory of Samuel J. Eallonardo III, M.D. ’93 Annette E. Kussmaul, M.D. ’93 In honor of Mark W. Eberbach, SOM ’17 Dr. and Mrs. Mark A. Eberbach In memory of Marco Elmann Elie M. Elmann, M.D. ’87 In honor of Joseph T. English, M.D. Dr. Punyabrata Roy
In honor of Gloria B. Chu, M.D. ’09 Mr. and Mrs. Peter P. Chu
In memory of Herbert M. Eskwitt, M.D. ’47 Joseph A. King, M.D. ’47 Myra Wise, Ph.D. and Burton L. Wise, M.D. ’47
In memory of Samuel Ciner Edward C. Halperin, M.D., M.A.
In memory of Muriel K. Ettenson John S. Ettenson, M.D. ’83
In memory of my parents and in celebration of my 40th year reunion Joseph B. Cleary, M.D. ’73
In honor of Cathey E. Falvo, M.D., M.P.H. Eugene Conrad, Ph.D., M.P.H. ’89, M.S.
In memory of Archie Cohn, M.D. ’27 Kenneth Cohn, M.D. ’68 In memory of George and Hannah Cohn Dr. Bruce M. Cohn, M.P.H. ’09 In honor of Wayne A. Colizza, SOM ’16 Wayne A. Colizza, M.D. In memory of Nereida Comas Waldemar A. Comas, Esq. In memory of Anthony and Frances Conca Dominick Conca, M.D. ’70 In memory of Joseph Corey Stephen L. Rubin, M.D. ’70 In memory of Thomas and Katheryn Cotter Paul F. Cotter, M.D. ’61 In memory of Dorothea Davis Robert A. Davis, M.D. ’74 In honor of Donald W. Delahanty, M.D. ’51 Kevin C. Delahanty, M.D. ’84 In memory of Marie and Martin Demling Ms. Dee Demling In memory of Nicholas E. DeRobertis, M.D. Alicia N. DeRobertis, M.D. ’12
In honor of Jeffrey A. Feinstein, M.D. ’91 Mr. and Mrs. Donald Feinstein In honor of The Fifth Pathway Program Thomas S. Walter, M.D. In memory of Jeffrey Floch Martin H. Floch, M.D. ’56 In memory of William Fok Eric C. Fok, M.D. ’93 In memory of Sheniqua C. Fontaine Ms. Cynthia L. FontaineSt. Clair In memory of Steven Forst, M.D. ’77 Mrs. Heidi Forst In memory of Martin J. Frank, M.D. ’70 Dr. and Mrs. Robert E. Crootof ’70 In memory of Steven James Frisch Mr. and Mrs. Thomas E. Frisch In memory of Frances and Aaron Frishman Dr. William and Mrs. Esther Frishman In memory of Robert L. Fruggiero Mr. and Mrs. Robert J. Fruggiero In honor of Victor Garcia’s thesis defense and novel work on 20HETE John D. Imig, Ph.D. In memory of Donald H. Gemson, M.D. ’78 Anita Grover, M.D. ’78 C H I R O N I A N • New York Medical College
49
HONOR ROLL OF DONORS (CONTINUED) In memory of Melvin Gerber, M.D. ’64 Mrs. Marilyn Gerber
In memory of Dr. and Mrs. Abraham R. Heller Paul B. Heller, M.D. ’68
In honor of Lewis and Barbara Kramer Mitchell S. Kramer, M.D. ’85
In memory of Raymond W. Gibbs, M.D. ’51 John W. Carrier, M.D. ’51
In memory of Dr. Edward Henderson David A. Seidman, M.D. ’86
In honor of Diane Krusko Ms. Pamela G. Lawrence
In memory of Shep Goldberg Albert C. Goldberg, M.D. ’63
In honor of Thomas H. Hintze, Ph.D. ’80, M.S. ’78 Maja L. LundborgGray, M.D. ’95 and Daniel S. Gray, M.D. ’91
In honor of Matthew Kurland Keith A. Kurland, M.D. ’79
In honor of Toni Goldberg Albert C. Goldberg, M.D. ’63 In memory of David Goldsmith Jay P. Goldsmith, D.M.D. In memory of Holly Goldstein Edward J. Goldstein, Ph.D., M.D. ’71 In memory of Robert Goldstein, M.D. Kevin L. Pehr, M.D. ’81 In honor of Alexander Golombek Sergio G. Golombek, M.D., M.P.H. ’04 In honor of Jaime Golombek Sergio G. Golombek, M.D., M.P.H. ’04 In memory of Thomas B. Graboys, M.D. ’70 Craig R. Heim, M.D. ’70 In memory of Edmund D. Grammer Mrs. Edmund D. Grammer In honor of Mr. and Mrs. Joseph Greco Gina M. GrecoTartaglia, M.D. ’91 In celebration of the completion of Amanda B. Green, M.D. ’12’s residency Mr. and Mrs. Mitchell A. Mund
In honor of Martin I. Horowitz, Ph.D. Harvey Weisslitz, M.D. ’65 In memory of Denise Ieraci Louise M. PrioloGrecco, M.D. ’87 In memory of Theodore Jacobs, M.D. ’55 Parvin M. Jacobs, M.D. ’55 In memory of Alan M. Jeffrey, Ph.D. Ms. Patricia JamesSommer In honor of Yves M. Jodesty, M.S. ’12 Dr. and Mrs. Yves M. Jodesty In memory of Russell “Rusty” Johnson Jerrold L. Wheaton, M.D. ’47 In honor of Jeff W. Josma, M.D. ’14 Ms. Marie E. Josma In honor of Fern R. Juster, M.D. Kathleen M. Flynn, M.D. ’89 In memory of Hilda and Abraham Kadish Dr. and Mrs. Alan Kadish In memory of Mrs. B. Kaiser Fran E. Kaiser, M.D. ’74
In memory of Michael Green, M.D. ’50 Henry J. Green, M.D. ’75
In memory of Gabor Kaley, Ph.D. Mr. and Mrs. Michael Forman
In memory of Stanley A. Green John L. Prue, M.D. ’74
In honor of Judith and Irwin Kallman Robert Alter, M.D.
In memory of Lester J. Greenberg, M.D. ’33 Stephan M. Greenberg, M.D. ’66
In honor of Dr. Nadim Y. Kassem Jawad Kassem, M.D.
In memory of J. Leonard Greif, M.D. ’39 Richard H. Greif, M.D. ’75
In honor of Jerald W. Katz, M.D. ’84 Mrs. Doris Katz
In memory of Eugene M. Grossman, M.D. V. Rachel Phillips, M.D. ’79
In memory of Ethel and William Katzenstein Martin S. Katzenstein, M.D. ’78
In honor of Susan Grossman, M.D. Dr. ConstanceLynne B. Maroney
In memory of Saul Kay, M.D. ’39 Grace Calef Kay, M.D. ’39
In honor of Rosario M. Gualtieri, M.D. ’39 Nicholas M. Gualtieri, M.D. ’69
In honor of Matthew C. Kessler, M.D. ’14 Frank J. Kessler, M.D.
In honor of Lauren Guenther, SOM ’15 Elyse W. Glaser, M.D.
In memory of Judith Frank Ketterer, M.D. ’61 John G. Ketterer, Jr., M.D. ’61
In honor of Edward C. Halperin, M.D., M.A. Betty SanchezCatanese, M.D. ’83 and Anthony J. Catanese, M.D. ’83 Richard A. Stram, M.D. ’78
In memory of Jenny Irene Keyes Mr. and Mrs. Richard J. Keyes, Jr.
In honor of Dr. Mark Hasten Ms. Barbara Flasch Lawrence J. Green, M.D. ’89 In memory of Hyman A. Hauptman, M.D. ’30 Bruce Hauptman, M.D. ’63 In honor of Kellie L. Hawkins, M.D. ’11, M.P.H. ’11 Mr. and Mrs. Robert S. Faircloth In memory of Mary Ellen Hawkins McAteer, M.D. ’75 Rebecca A. McAteer, M.D. ’08 50
SUMMER/ FALL 2015
In memory of Charles S. Kleinman, M.D. ’72 Edward F. Jordan, M.D. ’72 In memory of Solomon and Sophie Kluger Jeffrey Kluger, M.D. ’71 In memory of Robert Klurfeld Bronxville Teachers Association In honor of Manpreet K. Kochhar, M.S. ’10 Mr. Dev S. Kochhar and Dr. Param K. Kochhar In memory of Harry Kosovsky, M.D. 43 Steven I. Neibart, M.D. ’81
In honor of Mr. and Mrs. Ernest Kussmaul Annette E. Kussmaul, M.D. ’93 In honor of Priscilla LaBarbera Robert V. Blake, M.D. ’75 In memory of Bertram and Inge Landon Mr. Jerome D’Imperio In memory of Martin L. Lapkin, M.D. ’71 Alan R. Altman, M.D. ’71 In memory of Kathryn and Frank LaRusso Nicholas F. LaRusso, M.D. ’69 In honor of Nicholas F. LaRusso, M.D. ’69 Ms. Barbara Flasch In honor of the 50th wedding anniversary of Sigmund and Lorraine Lasker Susan J. Lasker, M.D. ’80 Richard H. Levine, M.D. ’80 In memory of George, Emily and Georgia Laubach George E. Laubach, M.D. ’63 In memory of Arthur Leber, M.D. Mark J. Leber, M.D. ’76 In memory of Bertha and Martin Lebovics Edward Lebovics, M.D. In honor of Eugene H. Lee, M.D. ’15 Mr. and Mrs. Hyan J. Lee In memory of Armand F. Leone, Sr., M.D. ’47 and Rita F. Leone, M.D. ’51 Activities Unlimited Ms. Gladys L. Astorga Mr. Vlad Balaeskoul Dr. and Mrs. Vincent A. Ciavarra Ms. Emilie De Mattia Drs. Frank and Carolyn DeMaria, Jr. Ms. Dina Giallombardo Ms. Priscilla Lee Goldman Mr. and Mrs. Seth M. Heyman High Mountain Orthopedics Mr. Alan R. Michaels The Sapienza Family Wayne Radiology Associates, LLC Mr. Steven M. Weiss In memory of Susan M. Liebeskind, M.D. ’90 Mr. Michael Liebeskind In celebration of the birthdays of Dr. Jay and Janet Liebowitz Donna A. Zeide, M.D. In honor of Joan, Melanie and Larry Liman Ilona W. Figura, M.D. ’83 In honor of Dr. Ling Ling Thomas R. Patnaude, M.D. ’74 In memory of Paul J. Lombardi, M.D. Donna J. LombardiGoldfus, M.D. ’93
In memory of Rene I. Lopez, Sr., M.D. Rene I. Lopez, Jr., M.D. In honor of Priscilla Ly Peter P. Ly, M.D. ’96 In memory of Isabel Gormley Lynch, R.N. ’55 John J. Lynch, M.D. ’58 In honor of Steven Mark Richard A. Stram, M.D. ’78 In memory of Augusta and Max Maron Norman L. Maron, M.D. ’70 In honor of Norman L. Maron, M.D. ’70 Michael R. Berman, M.D. ’70 In memory of Geraldine Marshall Harold Michlewitz, M.D. ’71 In memory of Margaret Mason Edward C. Halperin, M.D., M.A. In memory of Mary and Edward McCarrick Richard G. McCarrick, M.D. In memory of Barbara Ann McDaniel Sheriff M. Cole McDaniel In memory of John C. McGiff, M.D. Karen L. DavisBruno, Ph.D. ’91 Mr. and Mrs. Thomas P. Hart, Sr. Patrick J. Pagano, Ph.D. ’91 In memory of Katerina McNelis Joseph McNelis, M.D. ’87, M.P.H. ’15 In memory of Roberta A. McQuillan Mr. and Mrs. Patrick Carr Mr. and Mrs. Preston Gilroy Ms. Ethel J. Kelly Mr. and Mrs. Wayne E. Moshier Ms. Carmella A. Phillips Mrs. Mary Retaleato Mr. and Mrs. Gianfranco Stampone In memory of Rita Medoff Ms. Rita Medoff In honor of Monica R. Mehta, M.D. and Ruyintan Mehta Ariz R. Mehta, M.D. ’03 In honor of Carmen and Diego Mendez Mendez Medical Center, Inc. In memory of Marion F. Metalios Mr. James Z. Metalios In honor of Metropolitan Hospital Center Dr. Nelson A. Hernandez In memory of James T. Miglietta, M.D. ’81 Kenneth D. Kushner, M.D. ’81 In honor of D. Douglas Miller, M.D., C.M, M.B.A. Richard A. Stram, M.D. ’78
In celebration of the completion of Ross A. Mund, M.D. ’12’s residency Mr. and Mrs. Mitchell A. Mund In memory of Angela Murdocco James J. Murdocco, M.D. ’65 In celebration of Matthew Menzel Musselman’s graduation from University of California, Santa Cruz Miriam A. Menzel, M.D. ’85 In memory of Sheila and Emil Neibart Steven I. Neibart, M.D. ’81 In memory of Rosalind Neustein Charles Neustein, M.D. ’47 In memory of Ann and Morris Newman Leonard J. Newman, M.D. ’70 and Randi Newman In honor of Leonard J. Newman, M.D. ’70 Michael R. Berman, M.D. ’70 In memory of Robert W. Niehaus, M.D. ’50 Mrs. Mildred M. Niehaus In honor of Sara Noroozkhani, M.D. ’06 Mr. and Mrs. Ardeshir Noroozkhani In memory of Lawrence A. Norton, M.D. ’56 Mrs. Mary Norton In memory of Jose Nunez Ms. Elsa I. Nunez In honor of NYMC Emergency Medicine Residency Program Isaac Alexis, M.D. Dr. Gladys H. Lopez In honor of NYMC Emergency Medicine Residency Program Classes of 2014 and 2015 Dr. Selamawit YemaneMerriwether In honor of the NYMC Department of Obstetrics and Gynecology D. Jay Gloeb, D.O., G.M.E. ’86 In honor of the NYMC Department of Pediatrics Elmer C. Arteaga, M.D. In honor of Drs. Choudhury, Eshghi, Matthews, Phillips, Kono and Fullerton Srinivas Rajamahanty, M.D. In honor of NYMC Veterans of Military Service Thaddeus A. Figlock, M.D. ’60 In honor of Tobechi E. Okoronkwo, M.D. ’14 Uchenna A. Okoronkwo II, M.D. In memory of Thomas F. Oliver Michael T. Oliver, M.D. ’76 In honor of Lindsay C. Overton, M.D. ’08 Mr. and Mrs. Steven C. Overton
In memory of Robert D. Miningham Roy Christopher Monsour, M.D.
In honor of Naomi O. Oyemwense, SOM ’17 Ms. Robertha St. Clair
In memory of Catherine Demsky Minkel, R.N. ’47 Thaddeus A. Figlock, M.D. ’60
In honor of Thomas A. Pacicco, M.D. ’14 Arnold P. Good, M.D. ’85
In honor of our grandsons Lucas, Shane, Bennett and Isaac Dr. and Mrs. Frederick Z. Bierman
In memory of Bernard Pashcow Kay L. Cowan, M.D. ’87
In honor of Mothers who support their childrens’ dreams Dr. Raul Ayala
In memory of David Pasion, Sr. Sandra L. Sacks, M.D. ’97 and Harry G. Sacks, D.D.S., J.D.
In honor of Marilyn Pearl, M.D. Suzanne F. Roland, M.D. ’89 In memory of Dr. R. Pece George M. Arcieri, M.D. ’64 In honor of Elliott N. Perla, M.D. Dr. Tamas Otrok In memory of Eileen H. Pike, Ph.D. Carl P. Stamm, M.D. ’80, M.S. ’76 In memory of Frank J. Piper, M.D. ’58 Mrs. Teletta A. Piper In memory of Elizabeth Polaschik Mr. and Mrs. Michael R. Williams In honor of Stephanie L. Pollack, M.D. ’14 Mitchell C. Pollack, M.D. ’77 In memory of Louis G. Raff, M.D. ’24 Ira L. Raff, M.D. ’64 In honor of Lena T. Raiser Dennis T. Roarke, M.D. ’13 In memory of Sylvia, Charles and Leah Reback Harvey A. Reback, M.D. ’61 In memory of Herbert B. Reisman, M.D. Robert P. Reisman, M.D. ’78 In memory of Anne Reynolds Robert M. Yacynych, M.D. ’88 In memory of Ralph E. Ricciardi, Sr., M.D. ’37 and Mrs. Sarah Riccardi Ralph E. Ricciardi, Jr., M.D. ’71 In memory of Steven P. Rofsky Neil M. Rofsky, M.D. ’85 In memory of Frank Richard Romano, M.D. ’39 Patricia M. Raciti, M.D. ’11 In memory of Jerome and Roslyn Root Lee P. Root, M.D. ’89 In honor of Martin E. Rose, M.D. ’56 Nancy C. Rose, M.D. ’84 and G. Marc Jackson, M.D. In honor of Rachel Roth Ronald R. Roth, M.D. ’73 In honor of Dr. Samuel H. Rubin Adam D. Rubin, M.D. ’00 In memory of Vernon Rusheen Jeffrey M. Rusheen, M.D. In memory of Arlene Rymer William Rymer, M.D. ’72 In memory of Dr. Saul and Mrs. Evelyn Sacks Sandra L. Sacks, M.D. ’97 and Harry G. Sacks, D.D.S., J.D. In honor of Bijan Safai, M.D., D.Sc. Edgar S. Macias, M.D. In honor of Gabriela E. Sanchez, M.D. ’14 Mr. David E. Sanchez In honor of Betty SanchezCatanese, M.D. ’83 Edward C. Halperin, M.D., M.A. In honor of Henry I. Saphier, M.D. ’61 and Marieanna Saphier, R.N. ’60 Robert D. Green, M.D. ’61 In memory of Gerald and Jeanne Saxe Mr. and Mrs. George T. Weiffenbach In memory of Philip and Felice Scarlata Dr. Robin M. Scarlata C H I R O N I A N • New York Medical College
51
HONOR ROLL OF DONORS (CONTINUED) In memory of Martin J. Schwab Jennifer Koestler, M.D. Heather LuriePerla, M.D. and Elliott N. Perla, M.D. ’74 Mr. David D. Patterson Lori Anne Weir, M.D. ’99, M.P.H. ’09 Ms. Katharine Yamulla
In memory of William H. Somers, M.D. ’50 Mrs. Shirley W. Somers
In memory of Hyman Tobin Seymour Tobin, M.D. ’52
In honor of St. Vincent’s Hospital Dr. Scott M. Palyo
In honor of Seymour Tobin, M.D. ’52 Keith S. Tobin, M.D. ’85
In memory of Pincus A. Stahl, M.D. ’21 Martin B. Stahl, M.D. ’53
In honor of Marco J. Tomassi, M.D. ’03 Patricia McCarthy Tomassi
In honor of Ari Schwibner and Logan Ackerman Edward H. Katz, M.D. ’86
In memory of Frederick M. Stamp Mr. and Mrs. Robert J. Fruggiero
In honor of Michelle P. Tomassi, M.D. Patricia McCarthy Tomassi
In memory of Joseph J. Stavola, M.D. ’87 and Ms. Jeanne Serocke Shirley U. Salvatore, M.D. ’87 and James A. Salvatore, M.D. ’87
In memory of Harry L. Trambert, M.D. ’42 Jonathan J. Trambert, M.D. ’77
In celebration of the 85th Birthday of Morris Seidman David A. Seidman, M.D. ’86 In memory of Guy A. Settipane, M.D. ’57 Russell A. Settipane, M.D. ’84 In honor of Ravi and Manju Shah Dr. Nipa S. Gandhi In memory of Dr. H. N. Sharma Dr. and Mrs. Sanjay P. Thakur In memory of Joan and James Shaw Jacquelyn S. Loughlin, M.D. ’75 In celebration of Bret Silber’s Bar Mitzvah Jeff S. Silber, M.D. ’95 In memory of Ruth Simons David B. Simons, M.D. ’77 In honor of Dr. Sukeshi Singh Dr. and Mrs. Sanjay P. Thakur In memory of Robert A. Solow, M.D. ’48 Brian K. Solow, M.D. ’82 In honor of the SOM Class of 1956 David Werdegar, M.D. ’56 In honor of the SOM Class of 1959 Eugene A. Doherty, M.D. ’59 In honor of the SOM Class of 1960 Thaddeus A. Figlock, M.D. ’60 In honor of the SOM Class of 1962 Robert S. Goldstein, M.D. ’62 In honor of the SOM Class of 1965 Howard D. Cantwell, M.D. ’65 In honor of the SOM Class of 1966 Joseph T. Faraldo, M.D. ’66 In honor of the SOM Class of 1968 Kenneth E. Murdock, M.D. ’68 In honor of the SOM Class of 1969 Jonathan M. Kagan, M.D. ’69 In honor of the SOM Class of 1979 Gary M. Snyder, M.D. ’79
In memory of Mr. John Stein Mr. and Mrs. John Agni Dr. Sandra Shivers and Mr. Jed M. Shivers In memory of William Steinhilber Ernest J. Steinhilber III, M.D. ’57 In honor of Marc A. Stiefel, M.D. ’01 Mr. and Mrs. Roger H. Stiefel In memory of Gladis Stone Richard K. Stone, M.D. ’68 In memory of Stanley Stone Richard K. Stone, M.D. ’68 In honor of Alyssa Stram Richard A. Stram, M.D. ’78 In memory of Kitty Stram Richard A. Stram, M.D. ’78 In honor of Michelle Stram Richard A. Stram, M.D. ’78 In honor of Chari D. Stump, SOM ’17 Mr. and Mrs. David W. Stump In memory of Benjamin Sum Judith Fiedler Topilow, M.D. ’67 and Arthur A. Topilow, M.D. ’67 In honor of Joan V. Sutherland, R.N. Deon K. Sutherland, M.D. ’02 In memory of Alfred Tanz, M.D. ’48 Mrs. Patricia B. Doscher, R.N. ’57 and Crile Doscher, M.D. ’60 In honor of Adam S. Tanzer, M.D. ’96 Dr. and Mrs. Jason Tanzer
In memory of Belkis and Dogan Tugal Oya Tugal, M.D. In memory of Florence C. Voskovitch Col. James W. Voskovitch, M.D. ’59 In honor of Carolyn M. Wassong, M.D. ’08, M.P.H.’ 08 Mr. and Mrs. Louis J. Wassong In honor of Chana Weinstock Dr. and Mrs. Alan D. Weinstock In memory of Sidney and Lilyan Weissberg Steven M. Weissberg, M.D. ’66 In memory of Howard J. Westney, M.D. ’54 Grace G. Jorgensen, M.D. ’54 In honor of Ray T. Whitt, M.D. Morris C. Finkelstein, M.D. ’85, Ph.D. In celebration of Dr. Burton Wise’s 90th birthday Myra Wise, Ph.D. and Burton L. Wise, M.D. ’47 In memory of Ivy Wohl John M. Feder, M.D. ’87 In memory of Orlin V. Wry, M.D. ’58 Mrs. Cassandra Wry In memory of Despina Xouris George V. Tsimoyianis, M.D. ’82 In honor of in honor of JuHan (Eric) Yao Mr. Borlin Yao and Ms. ShiiBen Liaw In honor of Gabriela YaoCohen Alan R. Cohen, M.D. ’73 In memory of Joseph Zelazny Daniel Zelazny, M.D.
In memory of Rajeshwar Thakur Dr. and Mrs. Sanjay P. Thakur In celebration of my birthday Dr. Khin M. Thu
+ Indicates those who are deceased.
In honor of the SOM Class of 1984 Tedd L. Weisman, M.D. ’84 In honor of SOM Class of 1995 Grace W. Ho, M.D. ’95 and Ken T. Yang, M.D. ’95 In honor of the SOM Class of 2000 Earl A. Bueno, M.D. ’00 In honor of the SOM Class of 2017 Mr. and Mrs. Peter M. Dale
52
SUMMER/ FALL 2015
We have made every effort possible to provide a full and accurate list of donors to NYMC during the two-year period from July 1, 2013 through June 30, 2015. If we have omitted or improperly listed your name, please accept our apologies. If you detect an error, please contact our Office of Development and Alumni Relations at (914) 5944550 or email us at development@nymc.edu, so we may correct our records.
COMMENCEMENT 2015
Ph.D. candidates in the Graduate School of Basic Medical Sciences.
Master of Science candidates in the Graduate School of Basic Medical Sciences.
At the 156th Commencement exercises on May 21 in Carnegie Hall, NYMC leadership joined Commencement speaker, Jan K. Richardson P.T., Ph.D., OCS, FAPTA, professor emeritus, Duke University School of Medicine; past president, American Physical Therapy Association; past president, Association of Rheumatology Professionals of the American College of Rheumatology; and past president, Physical Therapy Fund. Front from left: Dr. Mark Hasten, chairman of the Board of Trustees; Dr. Richardson; and Robert W. Amler, M.D., M.B.A., dean of the School of Health Sciences and Practice and vice president of government affairs. Back from left: Edward C. Halperin, M.D., M.A., chancellor and chief executive officer; Alan Kadish, M.D., president; D. Douglas Miller, M.D., C.M., M.B.A., dean of the School of Medicine; and Francis L. Belloni, Ph.D., dean of the Graduate School of Basic Medical Sciences.
Henry I. Saphier, M.D. ’61, front row, second from right, joined proud alumni and faculty At podium: Student Commencement speaker Ph.D. candidate Victor G. Garcia. parents, a grandparent and a sibling of graduates gathered before the ceremony.
Sisters Rachelle Lodescar, M.D. ’13, and Joann Lodescar.
Doctor of Physical Therapy candidates in the School of Health Sciences and Practice.
Mace bearer Joan Y. June, M.S.Ed., assistant dean of student affairs, and flag bearers Timmy O’Connell, M.S., and Joshua Sterling.
Five School of Medicine graduates were inducted into the Armed Forces.
School of Medicine Class of 2015. C H I R O N I A N • New York Medical College
53
New York Medical College Office of Public Relations 40 Sunshine Cottage Road Valhalla, NY 10595
Artwork by Lana Malekan, School of Medicine Class of 2018
Non-profit U.S. Postage PAID Permit No. 19 Burlington, VT