Abstract
Enchondromas (EC) are frequent incidental findings on magnetic resonance imaging (MRI) performed for the diagnosis of joint pathology, especially observed on MRI examinations of the knee and shoulder. Enchondroma has potential for malignant transformation to chondrosarcoma (CS), and it may be difficult to distinguish EC from low-malignant CS on the basis of imaging or histopathology studies. Therefore, EC is mostly followed up to monitor any growth and/or changes indicating aggressive tumor.
There is no consensual evidence on when and how to follow up patients with EC with regard to potential malignant transformation. Therefore, the Danish Multidisciplinary Cancer Groups initiated and supported the elaboration of Danish guidelines in 2020 based on a literature review. The guidelines are presented here, in addition to a summary of the background literature.
Zusammenfassung
Enchondrome (EC) sind häufig Zufallsbefunde bei einer Magnetresonanztomographie (MRT), die zur Diagnostik einer pathologischen Veränderung eines Gelenks durchgeführt wird, insbesondere werden sie bei MRT-Untersuchungen von Knie und Schulter beobachtet. Bei einem Enchondrom kann es zur malignen Transformation in ein Chondrosarkom (CS) kommen, und es kann schwierig sein, ein EC von einem niedrig malignen CS auf der Basis bildgebender oder histopathologischer Untersuchungen zu unterscheiden. Daher erfolgt bei einem EC meistens eine Nachuntersuchung, um ein Wachstum und/oder auf einen aggressiven Tumor hinweisende Veränderungen zu erfassen. Es gibt keine allgemein akzeptierte Evidenz dazu, wann und wie die Nachuntersuchung von Patienten mit EC in Bezug auf eine potenzielle maligne Transformation erfolgen soll. Daher initiierten und unterstützten die Danish Multidisciplinary Cancer Groups im Jahr 2020 die Entwicklung dänischer Leitlinien auf der Grundlage einer Literaturübersicht. Die Leitlinien werden hier vorgestellt, daneben gibt es eine Zusammenfassung der Hintergrundliteratur.
Similar content being viewed by others
Introduction
Solitary enchondromas (EC) are frequent benign, often asymptomatic, cartilage tumors estimated to constitute 3–17% of all bone tumors [4, 28] and approximately 20% of all cartilage tumors [4]. Enchondroma has potential for malignant transformation to chondrosarcoma (CS), estimated to vary between 0 and 4.2% [3, 22]. It is difficult to obtain a valid risk estimate, as this requires detection of a preceding EC. It has therefore been recommended to look for histological EC changes when diagnosing CS [4], but this can potentially contribute to an overestimation of malignant transformation in EC because a CS may be inhomogeneous. The malignancy usually detected is a low-grade/grade 1 CS, which in the current World Health Organization (WHO) classification of 2013 has been assigned the synonymous term “atypical cartilage tumor” (ACT) because low-grade CS/ACT, despite local aggressiveness, rarely metastasizes [1, 15].
One of the major current problems is the incidental detection of EC on magnetic resonance imaging (MRI) performed when diagnosing joint pathology, especially observed on MRI of the knee and shoulder [19, 21, 33, 35]. The imaging features of detected cartilage tumors have to be assessed for signs indicating CS/ACT or an EC with a potential for transformation into CS/ACT. It is, however, often difficult to differentiate between EC and ATC on the basis of findings from imaging and histology, because cartilage tumors are often inhomogeneous. In addition, there is a well-known interobserver variation even among experienced pathologists and radiologists [32]. Due to the difficulties in distinguishing EC and ACT, incidentally detected cartilage tumors have often been observed over time with regard to malignant transformation. An EC of increasing size in adults and pain have typically been used as signs indicating malignant change, but pain cannot be used for EC found incidentally on MRI for other, possibly pain-causing, pathologies.
In Denmark, there has not been consensus on how to handle incidentally detected cartilage tumors, especially with varying follow-up procedures. The Danish Multidisciplinary Cancer Groups (DMCG.dk) have therefore initiated and supported the elaboration of the following evidence-based Danish guidelines in 2020 for the diagnosis and follow-up of solitary EC in adults (>18 years old). Tumors in the spine and head–neck region were not considered in these guidelines.
Danish guidelines
Solitary enchondromas in long bones, pelvis, and thoracic skeleton, including scapula
-
1.
Patients with the following imaging signs should be referred to a sarcoma center for treatment as the signs indicate aggressive cartilage tumor, ACT, or CS changes:
-
endosteal scalloping more than two thirds of the cortical bone on radiographs and/or MRI/CT
-
bone destruction
-
cortical remodeling/thickening
-
bone expansion and soft tissue mass (evidence level B).
-
-
2.
Growth greater than 6 mm over 12 months indicates active tumor necessitating referral to a sarcoma center (C).
-
3.
Enchondromas with cortical contact and possibly cortical impact or surrounding bone marrow edema on MRI should be followed up with MRI regardless of size.
-
First follow-up after 12 months.
-
Subsequent follow-up intervals should depend on the imaging features, where in particular cortical thinning and tumor size larger than 4 cm requires annual follow-up until the changes are deemed stable or are progressing and thereby require referral to a sarcoma center (C).
-
-
4.
Enchondromas larger than 2 cm without cortical contact/impact or surrounding bone marrow edema on MRI should be followed up with MRI after 12 months. If the enchondroma is unchanged, a final follow-up with MRI should be performed after 2 years unless there is growth or other features indicating aggressiveness (C).
-
5.
Enchondromas less than 2 cm on MRI or radiography without cortical contact/impact or surrounding bone marrow edema on MRI do not need imaging follow-up (B).
Solitary enchondromas in hands and feet
-
6.
In the case of increasing size of EC in the hands and feet, radiography is often sufficient for evaluating signs of malignancy in addition to fracture risk.
-
7.
Enchondromas with a size exceeding 5 cm2 on radiography as well as cortical destruction and soft tissue mass are suggestive of malignancy and may indicate supplementary MRI, if it has therapeutic consequences (B). Patients with such changes should be referred to a sarcoma center.
-
8.
There is no need for imaging follow-up of incidentally found EC with benign imaging appearance (B).
Literature review
The evidence for the guidelines is based on a literature review. The literature search was primarily performed in the PubMed database using four MeSH terms: “Chondroma”, “Chondrosarcoma”, “Diagnostic Imaging”, and “Magnetic Resonance Imaging” confined to the period 1 January 1990 to 10 December 2019 and English language (Fig. 1). Initially, a rough selection was made based on titles of the publications obtained followed by 98 abstract readings, resulting in 52 publications selected for full-text reading; 25 of them encompassed data usable for the guidelines. By screening references in the publications obtained and citations of relevant publications using Web of Science, a further four publications were included (Fig. 1).
Flowchart for the literature search. The three search strings used: 1. (“Chondroma”[Mesh]) AND “Chondrosarcoma”[Mesh] AND ((“1990/01/01”[PDat]: “2019/12/10”[PDat]) AND English[lang]) AND (Humans[Mesh] AND English[lang]); 2. (“Chondroma”[Mesh]) AND “Diagnostic Imaging”[Mesh] AND ((“1990/01/01”[PDat]: “2019/12/10”[PDat]) AND Humans[Mesh] AND English[lang]); 3. (“Chondroma”[Mesh] AND “Magnetic Resonance Imaging”[Mesh]) AND ((“1990/01/01”[PDat]: “2019/12/10”[PDat]) AND Humans[Mesh] AND English[lang])
Data regarding imaging signs of EC versus CS/ACT and surveillance of EC, as background for the guidelines, were as stated in the next section.
Imaging signs of benign vs. atypical and malignant intraosseous cartilage tumor
Intramedullary cartilage tumors are thought to be formed from remnants of hyaline cartilage in the bone marrow, which can grow and displace normal bone marrow. Enchondroma is usually located centrally in tubular bones and is most frequent in short tubular bones, the proximal femur, and the proximal humerus [4]. Enchondroma in long tubular bones is mostly located in the metaphysis and often relatively close to the previous growth plate, but EC may also occur in epiphyses [30].
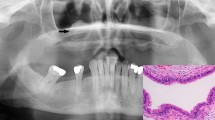
Radiographically, EC usually appear as an intramedullary lobulated lesion with calcifications displaying a stippled, pop-corn-like or ring and arc configuration (Fig. 2). On MRI, EC has a rather characteristic appearance because the matrix of hyaline cartilage exhibits a homogeneously high signal in a lobulated configuration on water-sensitive sequences, such as STIR (short tau inversion recovery) and T2-weigted or proton density (PD) fat-suppressed sequences. The cartilage areas are usually surrounded by septae with low signal intensity, often in a ring and arc configuration, corresponding to matrix calcifications, in addition to small dot-shaped calcifications. On T1-weighted images, the cartilage areas exhibit intermediate signal, sometimes mixed with high signal intensity areas due to marrow fat dispersed between the cartilage areas, especially at the periphery of EC (Fig. 2). Magnetic resonance imaging usually adds diagnostic value to radiography in the assessment of intramedullary cartilage tumors. In a study by DeBuckleer et al. [11], the diagnosis of EC and CS was confirmed by supplemental MRI in five of 16 EC and 14 of 16 low-grade malignant CS tumors.
Enchondroma larger than 2 cm without cortical contact necessitating follow-up after 12 and 36 months. a, b Radiographs showing typical enchondroma changes with stippled and pop-corn-like calcification in the proximal tibia. b, c Magnetic resonance imaging: coronal T1-weighted and sagittal proton fat-saturated sequences show characteristic well-delineated intraosseous cartilage areas surrounded by septae
Microscopically, EC consists of areas of hyaline cartilage surrounded by bone marrow, whereas a malignant cartilage tumor exhibits permeative growth with malignant cartilage tissue replacing bone marrow tissue. The diagnosis of grade 2 and 3 CS can mostly be made on the basis of imaging and verified histologically, and differentiation between EC and grade 2–3 CS is usually made without major problems. However, the differentiation between EC and low-grade CS/ACT is often difficult and remains a diagnostic challenge with imaging as well as histopathologically [32].
The problem of differentiating EC and CS/ACT has increased in recent years due to the frequent use of MRI for the diagnosis of joint pathology, especially knee and shoulder MRI where cartilage tumors or cartilage remnants are frequent incidental findings. The prevalence of incidentally detected cartilage tumors on shoulder MRI has been reported to be 2.1% [21]; for knee MRI performed for the indication of pain, the reported prevalence has ranged from 2.3 to 2.9% [19, 33, 35], whereas the prevalence was only 0.8% in 601 healthy persons [19]. Cartilage tumors detected incidentally at the knee were found most frequently in the distal femur (approximately 2%) followed by the proximal tibia (0.5–0.7%) and the proximal fibula (0.1–0.2%), and they were generally small [33, 35]. In the study by Stomp et al. [33], encompassing 1285 knee MRI examinations, 86% of 49 tumors were smaller than 2 cm and in Walden’s study of 449 knee MRI examinations, 57% of 23 tumors were smaller than 1 cm [35]. The tumors were often located close to the previous growth plate. Stomp et al. observed contact with the growth plate in 29 of the 48 tumors in tubular bone, nine crossed it and only ten were more than 2 cm from the growth plate. In Walden’s study, 72% of the tumors were less than 1.5 cm from the growth plate [35]. In the prevalence study of shoulders (encompassing 477 MRI examinations), seven of ten randomly detected EC were smaller than 1 cm and the three larger ones measured a maximal 1.2 cm; eight of nine EC in the humerus were close to the growth plate and one was less than 1.5 cm from it [21]. The frequent close relationship to the growth plate supports the notion that incidentally observed EC may represent persisting hyaline cartilage from the growth plate displaced into the bone marrow during growth. They are typically less than 2 cm and located within 2 cm of the growth plate area [27]. In the case of pure cartilage remnants without tumorous growth, there may not be visible matrix calcifications on radiographs [27].
The joint MRI examinations revealing incidental cartilage tumors usually only consist of water-sensitive as well as T1-weighted sequences. The MRI signals obtained by such standard sequences rarely allow for a definite differentiation between EC and CS/ACT, but there is evidence of imaging signs indicating aggressive cartilage tumor based on numerous comparative studies [6, 8, 12,13,14, 17, 20, 23, 28, 29]. They have been focused mainly on cartilage tumors in long tubular bones, as EC in the hands and feet are mostly visualized sufficiently with radiography.
Long tubular bones
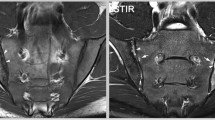
In long tubular bones, the following imaging characteristics are indicative of aggressive cartilage tumor, ACT or CS changes: endosteal scalloping greater than two thirds of the cortical bone on radiographs and/or MRI/computed tomography (CT), bone destruction, cortical remodeling/thickening, bone expansion, and soft tissue mass. Additional characteristics are: bone marrow edema and enhancement around the tumor, and ring and arc enhancement in the tumor process (Fig. 3).
Active cartilage tumor (ACT): radiographs (a, b); MRI coronal T1-weighted and axial STIR images (c, d); coronal and axial post-contrast T1-weighted fat saturation images (e, f). The tumor has a large area of cortical contact accompanied by scalloping in addition to ring and arc enhancement. Tumor curettage was performed and the histological findings were consistent with ACT/grade 1 chondrosarcoma
The evidence for most of these characteristics is based on a study by Murphey et al. conducted in 1998 [28], comprising 187 patients, 92 with EC and 95 with CS. In 90% of the patients, the distinction between EC and CS could be made on the basis of endosteal scalloping over two thirds of the cortex depth or the extent of scalloping corresponding to more than two thirds of the tumor in relation to the cortex, cortical destruction, soft tissue mass (by CT/MRI), and radiographic periosteal reaction as well as markedly increased tracer uptake on bone scintigraphy. In Murphey’s study and in numerous subsequent comparative studies, the most consistently documented evidence of aggressiveness/malignancy was endosteal scalloping corresponding to more than two thirds of the cortical thickness [14, 28]. However, scalloping detected on MRI may not be a sure sign of malignancy. In a small study comprising 11 EC (verified by histology in nine cases and by 4–7-year follow-up in two cases) located eccentrically in long tubular bones, the prevalence of scalloping was 100% with an extent corresponding to 50–100% (mean 75%; [5]). This may partly be due to the location of lesions close to the cortex causing partial volume effect on MRI. In such cases, CT scanning may be helpful for clear visualization of the cortex [27].
Peritumoral bone marrow edema has been described as a sign of aggressive tumor [1, 6, 23], but has not been a constantly observed finding. Similarly, peritumoral enhancement or tumor enhancement has been reported as a sign of aggressiveness [1, 10, 13, 14].
Evidence regarding the size of cartilage tumors to be used for differentiating EC from ACT is weak, although the mean length of EC was less than 5 cm compared with more than 5 cm for CS/ACT in Murphey’s study [28]. In general, the size of CS/ACT tumors is mostly greater than 4–5 cm, but EC may also have this size [1, 9].
Small tubular bones
In small tubular bones of the hands and feet, malignant characteristics are cortical destruction/pronounced scalloping, involvement of the phalangeal ends, and soft tissue mass [16, 18]. The EC in small tubular bones are usually sufficiently assessed by radiography where a tumor size greater than 5 cm2, cortical destruction, and/or a soft tissue mass are signs of possible malignancy [18]. Supplementary MRI may be obtained in the case of therapeutic consequences.
Enchondromas in the fibula, a non-weight-bearing long tubular bone, have EC characteristics rather similar to those of EC in small tubular bones [25]. Five radiographic signs indicating malignancy have been described: size >4 cm, cortical destruction, cortical thickening, periosteal reaction, and soft tissue mass [25]. The same characteristics are applicable with MRI, taking into account that benign fibular EC often presents with pronounced endosteal scalloping [9].
The use of more advanced MR techniques such as diffusion-weighted imaging (DWI), MR-perfusion techniques, and MRI-based texture analyses has been investigated regarding the differentiation between EC and CS/ACT [12, 13, 26]; however, currently the data are limited to a few studies and advanced techniques cannot be recommended for routine clinical use. Future studies have to investigate their role.
Bone scintigraphy may have limited diagnostic value in differentiating EC and ACT. Scintigraphic uptake occurs in both conditions, but a statistically significant difference has been reported by relating the tumor uptake to the physiological uptake in the anterior superior crista iliaca [17]. Positron emission tomography (PET)-CT with quantification by SUVmax (maximum standardized uptake value) seems to be able to differentiate between benign and malignant cartilage tumors. Thus, only one of 17 patients with an SUVmax <2.0 had CS, while 18 of 19 patients with CS had an SUVmax >2 [24]. It is, however, still unclear whether PET-CT can differentiate between EC and ACT and there is no basis for recommending PET-CT in standard evaluation of cartilage tumors [34].
Follow-up of enchondromas
There is no consensual evidence regarding when and how to follow up EC with regard to malignant transformation [1]. Enchondromas found incidentally on MRI are often followed up with MRI according to variable recommendations with intervals of 1–3 years depending on the EC size and imaging features [1]. However, tumors smaller than 1–2 cm localized near the previous growth plate can be considered cartilage residues without the need for follow-up unless there are atypical imaging features ([21, 33, 35]; Fig. 4). In the study by Stromp et al. [33] atypical/aggressive tumors were relatively frequent findings among incidentally detected tumors greater than 2 cm; three out of eight tumors were ACT, indicating a need for follow-up of tumors that are larger than 2 cm with regard to increasing size or other features indicating malignancy. During follow-up, an increase in size of more than 6 mm within 12 months can be interpreted as a sign of active tumor [31] in addition to the occurrence or progression of cortical scalloping.
There is no valid evidence for the length of surveillance of EC regarding potential malignancy. In a recent follow-up study the detection of EC growth and malignant transformation were rare findings usually seen at 2 years of follow-up, suggesting a need for follow-up of at least 3 years [2]. A potential regression of EC has been reported [7]; 11 out of 21 EC/ACT in long tubular bones were observed to regress during a follow-up period of at least 12 months with decreasing tumor size [7]. However, it was a small retrospective study with histological EC confirmation in only two patients. In a recent study involving 347 patients with EC, no regression was reported [9] and the potential for regression is thus uncertain.
For EC frequently detected on knee and shoulder MRI, a validated MR follow-up algorithm has been developed in Birmingham [9]. This algorithm was mainly designed for the purpose of guidance for referral to tumor specialists. Regardless of tumor size, this should be done for all tumors with generalized endosteal scalloping, which was defined as an extent of more than 10% of the tubular bone circumference. All other tumors were categorized with regard to size and scalloping. Tumors with less than 10% endosteal scalloping and larger than 4 cm in size were recommended to be followed up after 1 and 3 years, whereas tumors smaller than 4 cm were recommended to be followed up after 3 years. For tumors without endosteal scalloping (no cortical contact) and a size greater than 4 cm, a 3-year follow-up was recommended. In these three follow-up settings, the detection of changes in a malignant direction should result in referral to a tumor specialist whereas the follow-up program should be ended if the tumor has remained unchanged. Follow-up is not recommended for tumors that are smaller than 4 cm without endosteal scalloping. It is an interesting algorithm that should be tested further. Unfortunately, the depth of scalloping was not taken into account, as was done in almost all other studies conducted since Murphey detected this to be one of the best signs indicating malignancy [28].
Due to the diagnostic superiority of MRI compared with radiography [11], the former is often used for surveillance of cartilage tumors, but it is a relatively expensive procedure. To reduce the cost, the use of radiography has been recommended in the United States for surveillance of EC with benign radiographic appearance, limiting MRI to patients with suspicious clinical or imaging findings, resulting in reduced costs [2, 36].
Practical conclusion
-
There is consensus that endosteal scalloping of more than two thirds of the cortical thickness indicates possible malignant transformation of enchondromas (EC), and that suspicious EC should be followed up with regard to their potential development to chondrosarcoma.
-
There is no consensus to date on the frequency and duration of follow-up.
-
Enchondromas that are smaller than 2 cm will remain benign if they are without cortical contact.
-
Some of the signs suggestive of aggressive tumors and the recommendations for their management—e.g., tumor larger than 5 cm in the tubular bones, growth of more than 6 mm over 12 months, and follow-up regimen after 12 months—are not fully accepted or scientifically proved yet, since they rely only on one or a few studies with varying study concepts.
References
Afonso PD, Isaac A, Villagran JM (2019) Chondroid tumors as incidental findings and differential diagnosis between enchondromas and low-grade chondrosarcomas. Semin Musculoskelet Radiol 23:3–18
Akoh CC et al (2019) Radiographic enchondroma surveillance: assessing clinical outcomes and costs effectiveness. Iowa Orthop J 39:185–193
Altay M et al (2007) Secondary chondrosarcoma in cartilage bone tumors: report of 32 patients. J Orthop Sci 12:415–423
Brien EW, Mirra JM, Kerr R (1997) Benign and malignant cartilage tumors of bone and joint: their anatomic and theoretical basis with an emphasis on radiology, pathology and clinical biology. I. The intramedullary cartilage tumors. Skeletal Radiol 26:325–353
Bui KL et al (2009) Cortical scalloping and cortical penetration by small eccentric chondroid lesions in the long tubular bones: not a sign of malignancy? Skeletal Radiol 38:791–796
Choi BB et al (2013) MR differentiation of low-grade chondrosarcoma from enchondroma. Clin Imaging 37:542–547
Chung BM et al (2018) Magnetic resonance imaging follow-up of chondroid tumors: regression vs. progression. Skeletal Radiol 47:755–761
Crim J et al (2015) Can imaging criteria distinguish enchondroma from grade 1 chondrosarcoma? Eur J Radiol 84:2222–2230
Davies AM et al (2019) A retrospective validation of an imaging protocol for the management of solitary central cartilage tumours of the proximal humerus and around the knee. Clin Radiol 74:962–971
De Beuckeleer LH et al (1995) Magnetic resonance imaging of cartilaginous tumors: a retrospective study of 79 patients. Eur J Radiol 21:34–40
De Beuckeleer LH, De Schepper AM, Ramon F (1996) Magnetic resonance imaging of cartilaginous tumors: is it useful or necessary? Skeletal Radiol 25:137–141
De Coninck T et al (2013) Dynamic contrast-enhanced MR imaging for differentiation between enchondroma and chondrosarcoma. Eur Radiol 23:3140–3152
Douis H et al (2015) Is there a role for diffusion-weighted MRI (DWI) in the diagnosis of central cartilage tumors? Skeletal Radiol 44:963–969
Douis H et al (2018) What are the differentiating clinical and MRI-features of enchondromas from low-grade chondrosarcomas? Eur Radiol 28:398–409
Doyle LA (2014) Sarcoma classification: an update based on the 2013 World Health Organization Classification of Tumors of Soft Tissue and Bone. Cancer 120:1763–1774
Fayad LM et al (2015) Chondrosarcomas of the hands and feet: a case series and systematic review of the literature. Eur J Radiol 84:2004–2012
Ferrer-Santacreu EM et al (2016) Enchondroma versus chondrosarcoma in long bones of appendicular skeleton: clinical and radiological criteria—A follow-up. J Oncol 2016:8262079
Gajewski DA et al (2006) Differentiating clinical and radiographic features of enchondroma and secondary chondrosarcoma in the foot. Foot Ankle Int 27:240–244
Grainger R et al (2008) What is the clinical and ethical importance of incidental abnormalities found by knee MRI? Arthritis Res Ther 10:R18
Herget GW et al (2014) Insights into enchondroma, enchondromatosis and the risk of secondary chondrosarcoma. Review of the literature with an emphasis on the clinical behaviour, radiology, malignant transformation and the follow up. Neoplasma 61:365–378
Hong ED et al (2011) Prevalence of shoulder enchondromas on routine MR imaging. Clin Imaging 35:378–384
Horvai A, Unni KK (2006) Premalignant conditions of bone. J Orthop Sci 11:412–423
Janzen L et al (1997) Intramedullary chondroid tumors of bone: correlation of abnormal peritumoral marrow and soft-tissue MRI signal with tumor type. Skeletal Radiol 26:100–106
Jesus-Garcia R et al (2016) Is PET-CT an accurate method for the differential diagnosis between chondroma and chondrosarcoma? SpringerPlus. https://doi.org/10.1186/s40064-016-1782-8
Kendell SD et al (2004) Radiographic differentiation of enchondroma from low-grade chondrosarcoma in the fibula. Skeletal Radiol 33:458–466
Lisson CS et al (2018) Diagnostic value of MRI-based 3D texture analysis for tissue characterisation and discrimination of low-grade chondrosarcoma from enchondroma: a pilot study. Eur Radiol 28:468–477
Mulligan ME (2019) How to diagnose enchondroma, bone infarct, and chondrosarcoma. Curr Probl Diagn Radiol 48:262–273
Murphey MD et al (1998) Enchondroma versus chondrosarcoma in the appendicular skeleton: differentiating features. Radiographics 18:1213–1237 (quiz 1244–5)
Parlier-Cuau C et al (2011) When should we biopsy a solitary central cartilaginous tumor of long bones? Literature review and management proposal. Eur J Radiol 77:6–12
Potter BK et al (2005) Solitary epiphyseal enchondromas. J Bone Joint Surg Am 87:1551–1560
Sampath Kumar V et al (2016) Surveillance of intramedullary cartilage tumours in long bones. Bone Joint J 98-B:1542–1547
Skeletal Lesions Interobserver Correlation among Expert Diagnosticians (SLICED) Study Group (2007) Reliability of histopathologic and radiologic grading of cartilaginous neoplasms in long bones. J Bone Joint Surg Am 89:2113–2123
Stomp W et al (2015) Prevalence of cartilaginous tumours as an incidental finding on MRI of the knee. Eur Radiol 25:3480–3487
Subhawong TK et al (2017) F‑18 FDG PET differentiation of benign from malignant chondroid neoplasms: a systematic review of the literature. Skeletal Radiol 46:1233–1239
Walden MJ, Murphey MD, Vidal JA (2008) Incidental enchondromas of the knee. AJR Am J Roentgenol 190:1611–1615
Wilson RJ et al (2015) Overutilization and cost of advanced imaging for long-bone cartilaginous lesions. Ann Surg Oncol 22:3466–3473
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A.G. Jurik, B.H. Hansen and K. Weber declare that they have no competing interests.
For this article no studies with human participants or animals were performed by any of the authors. All studies performed were in accordance with the ethical standards indicated in each case.
The supplement containing this article is not sponsored by industry.
Rights and permissions
About this article
Cite this article
Jurik, A.G., Hansen, B.H. & Weber, K. Solitary enchondromas—diagnosis and surveillance. Radiologe 60 (Suppl 1), 26–32 (2020). https://doi.org/10.1007/s00117-020-00681-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00117-020-00681-7