Abstract
To assess the longitudinal incidence of Kawasaki disease (KD) within the well-defined predominantly White population of Olmsted County, MN. This retrospective cohort study used a population-based medical record linkage system and manual chart reviews to identify children with KD in Olmsted County, MN between January 1, 1979-December 31, 2016. Age- and gender-adjusted incidence rates were calculated using the 2010 U.S. White population. 124 children with KD were confirmed during the study period (median age 3.5, 61% male, 85% White, 9% Asian). The overall age- and gender-adjusted incidence rates for all ages and < 5 years old were 9.8 and 21.4 per 100,000 person-years, respectively. There was an overall increase in incidence up to 1994 followed by plateau, except among children between the ages of 1–5 years. There was also an overall increase in incidence among females compared to males. 24% of children had cardiac complications. While the overall incidence of KD in Olmsted County appears to be stable since 1994, the incidence of KD in subgroups of children 1–5 years old and females seems to have increased. Given the rising trends and one-quarter of children developing cardiac complications, further studies identifying factors driving these trends are warranted.
Similar content being viewed by others
Introduction
Kawasaki Disease (KD) is a serious pediatric pro-inflammatory condition recognized as the leading cause of acquired heart disease among children of developed nations, and thus has led to significant efforts to determine its etiology and optimize timely treatment [1, 2]. Epidemiological studies have been reported in over 60 countries about the incidence of KD, with the incidence in Asian countries being 10 times higher than that of Western countries and continuing to rise [2] Epidemiological studies on KD in the United States have been primarily conducted in the West Coast region [3,4,5] with a large proportion of Asian populations. Recently, Coronavirus disease 2019 (COVID-19) causes Multisystem Inflammatory Syndrome (MIS) in previously healthy children which overlaps with clinical features of KD [6]. Given this unexpected emergence of MIS by COVID-19, a long-term longitudinal incidence for KD could be timely as it establish a baseline trend of KD before COVID-19 pandemic and may provide an insight into the epidemiology of KD in relation to previous pandemic (eg, 2009 H1N1 influenza).
Longitudinal age- and gender-adjusted incidence studies of KD in a well-defined population are limited in the U.S., particularly in communities with predominantly White populations such as in the Midwestern region. Although there is a lack of an active nationwide surveillance system for KD in the U.S., nationwide studies have been conducted [4, 5, 7,8,9,10,11,12]. Most previous studies have estimated KD incidence based on inpatient hospitalization rates, usually only among children < 5 years old [11].U.S. studies have shown average annual rates of incidence, ranging from 8 to 25 per 100,000 person-years, predominantly in non-White populations and over short-term periods of time [13]. In addition, coronary artery aneurysms associated with KD have been reported to develop in 2.3% of cases in the U.S. [14] International data generally reports an average of 5% of patients developing persistent coronary changes and 25% with complications such as aneurysms [2] Given the large geographical area, large population, and racial diversity in the U.S., as well as the lack of a national surveillance system for KD, there is a need for epidemiological information in a mixed rural–urban setting with a predominantly Caucasian population [12] We aim to assess the longitudinal, population-based incidence of KD between 1979–2016 using the well-defined predominantly White population of Olmsted County, Minnesota, utilizing both inpatient and outpatient clinical data.
Methods
Study Setting
This study was conducted in Olmsted County, Minnesota, which has similar population characteristics to the U.S. White population, with the exception that a large proportion of the population is employed in the healthcare field [15]. The Olmsted County population has the same age, sex, and ethnic characteristics as Minnesota in general, with a majority of non-Hispanic Whites (82%) and minorities of the population comprised of African American (6%), Asian (6%), Hispanic (5%) and mixed descent (1%) [16]. Olmsted County provides an ideal location to perform population-based studies under the auspices of the Rochester Epidemiology Project (REP) which has archived the medical records of virtually all persons residing in Olmsted County for more than half a century. It maintains an electronic index of both inpatient and outpatient records for medical and surgical events, and has archived all addresses and demographic information since 1966, allowing researchers to retrieve all medical data for disease trends in this population. Over 95% of residents authorize their medical information for research use [17] The Mayo Clinic, and Olmsted Medical Center as a non-Mayo Clinic health care provider along with their affiliated Hospitals which are the major partner of the REP provide primary and specialty care for majority of the community. Therefore, health care is virtually self-contained in our study setting. This makes our study setting an excellent location to perform a population-based longitudinal study such as this [15, 18]. This study protocol was approved by the institutional review boards at both Mayo Clinic and Olmsted County Medical Center.
Study Design
The study was designed as a population-based retrospective cohort study, which assessed longitudinal age- and gender-adjusted incidence rates of KD per 100,000 person-years among children residing in Olmsted County, MN between 1979 and 2016.
Study Subjects
We identified all patients 18 years of age or younger with an index date of KD (previously called mucocutaneous lymph node syndrome) between January 1, 1979-December 31, 2016. The inclusion criteria were residents of Olmsted County, MN for at least one year prior to the date of KD diagnosis (index date). Patients who had not provided authorization for the use of their medical records for research purposes or those who were not Olmsted County residents at index date and for at least one year prior to index date were excluded in case they were referral cases seeking tertiary care from outside of the county. Patients were also excluded if they had a physician diagnosis of KD, but their chart exhibited limited documentation of number of days of fever or number of other diagnostic clinical symptoms, preventing the reviewers from verifying true cases of KD as defined by the American Heart Association (AHA) guidelines.
Case Ascertainment of KD
Using the REP database, we initially conducted medical index search for all potential KD cases using the International Classification of Diseases, Ninth Revision (ICD-9) code 446.1, International Classification of Diseases, Tenth Revision (ICD-10) code M30.3, and Hospital Adaptation of the International Classification of Diseases second edition (HICDA) code 4,460,213 for Mucocutaneous Lymph Node Syndrome and 4,460,214 for Kawasaki Disease. Then, we performed comprehensive medical record reviews for potential cases of KD to ascertain each case based on the AHA guidelines of diagnosis [19]. A complete KD diagnosis case was defined as fever of at least 5 days duration (or shorter if treatment was initiated sooner than 5 days of illness) along with at least 4 other diagnostic clinical symptoms (bilateral conjunctival congestion, changes of lips and oral cavity, polymorphous exanthema, changes of peripheral extremities, and cervical lymphadenopathy) or evidence of coronary artery abnormality from echocardiogram results. Incomplete KD diagnosis case was defined as fever of at least 5 days duration with only 2–3 other diagnostic clinical symptoms.
Other Pertinent Variables
We collected the following data from the medical records of each patient: demographics (age, gender, race), BMI closest to index date, and history of any infection in the previous one month from KD index date. For the purpose of this study, while we reported distribution of each race and ethnicity for characterization, race and ethnicity were classified as Non-Hispanic White, Asian, and others (Native Hawaii/Pacific Islander, African American, Hispanic, American Indian/Alaskan Native, and Other). We determined whether echocardiography was performed for each patient identified with KD within 3 months, allowing us to assess whether coronary artery abnormalities, ventricular function abnormalities, or any other cardiac abnormalities such as myocarditis were identified. We also collected data on treatment of KD for each patient (IVIG infusion, aspirin, and steroid medications).
Statistical Analysis
Basic demographic and clinical characteristics of identified KD cases were summarized using median (with 25th – 75th percentiles) for continuous variables and percentages for categorical variables. Rates of complications were compared with Chi-Square and Wilcoxon rank-sum for categorical and continuous data respectively.
Overall age- and gender-adjusted incidence rates were estimated using the number of cases in each age group < 1, 1, 2–4, 5–17 and gender as the numerator, with corresponding age- and gender-specific person-years at risk as denominators. Person-years at risk were estimated using the REP census which enumerates the population of people who live in Olmsted County by utilizing individual timeline methods [20]. The rates from our study were age- and gender-adjusted to the U.S. white population in 2010. Ninety-five percent confidence intervals (CIs) for the incidence rates were calculated under the Poisson distribution. Crude overall and age- and gender-specific rates per calendar year were calculated. Poisson regression was used to assess gender, age, and calendar year trends. Non-linear trends and interactions were investigated. We also reported temporal trend of cardiac complications (%) and treatment patterns (%).
Results
Characteristics of Study Subjects
We initially identified 181 potential KD cases during the study period between January 1, 1979 and December 31, 2016 using ICD and HICDA codes. Fifty-seven patients were excluded: 41 were found to be non-KD cases after manual chart review based on the AHA diagnostic criteria, 15 were not a resident of Olmsted County, MN, and 1 had insufficient medical record to ascertain true KD diagnosis with manual review. Table 1 shows the demographic information of the remaining 124 patients who met inclusion criteria for the study (median age [IQR]: 3.5 [2.3–6.3], 61% male, 85% White, 9% Asian). Winter and spring were found to have higher percentages of KD diagnosis (Table 1).
Incidence of Kawasaki Disease
The overall age- and gender-adjusted incidence rate for all ages and < 5 years were 9.2 (95% CI 7.6 – 10.9) and 21.4 (95% CI 16.7 – 26.0) per 100,000 person-years, respectively (Table 2). There was an overall increased linear trend in incidence up to 1994, since when the incidence has remained stable (Fig. 1).
This appears to be driven by children 2–4 years old, who have appeared to increase incidence throughout the study period, while infants and school-aged children (5–17 years) did not increase in incidence (Fig. 2).
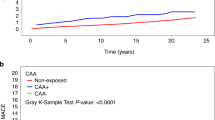
Males (11.7; 95% CI 9.2 – 14.7 per 100,000 person-years) had a higher incidence rate compared to females (7.8; 95% CI 5.8 – 10.4 per 100,000 person-years) (P = 0.03). Further investigation showed a difference in gender-specific incidence trends (interaction P = 0.008) between male and female patients, with an increasing incidence in female patients and a steady fluctuation in male patients (Fig. 3).
Outcomes of Kawasaki Disease
We assessed the cardiac complications exhibited over the study period. Eleven subjects had no information on any complications. Twenty-eight (24%) study subjects had cardiac complications as a result of KD, all including coronary artery abnormality of either aneurysm, ectasia or periluminal thickening, and one patient with a miscellaneous cardiac abnormality. Such complications occurred disproportionately more in males (78.6%, vs. 54.1% of females P = 0.022) and younger patients (P = 0.041). The proportion with cardiac complications was highest among those less than 2 years old (41.7%). The prevalence of cardiac complications appears to have decreased over time although this is difficult to generalize with a small sample size.
Table 1 summarizes the treatment pattern of children with KD. Twenty-nine (24%) of patients did not receive IVIG or aspirin as treatment. 93 cases (75%) were treated with both IVIG and aspirin, and 1 patient was also treated with steroids. The 28 cases who did develop cardiac complications and the 29 who had not received IVIG or aspirin as treatment were found to be different patients. Almost all patients (96.4%) with cardiac complications received treatment with IVIG, and 100% received aspirin. Fifteen of the 29 patients who were not treated with any IVIG or aspirin were cases of incomplete KD without sequelae of coronary abnormalities.
Distribution of Kawasaki Disease Symptoms
The median days of fever were 6 (IQR 5–7). Symptoms in frequency were reported as the following: bilateral conjunctival congestion (n = 103, 83%), polymorphous exanthema (n = 98, 79%), and changes of the lips and oral cavity (n = 98, 79%), cervical lymphadenopathy (n = 91, 73%), and desquamation of palms and soles (n = 86, 69%). Twenty-nine cases where categorized as having incomplete KD (< 4 symptoms and no coronary abnormalities). Forty (32%) of cases had symptoms of upper respiratory illness within one month prior to KD index date.
Discussion
To our knowledge, this is the most long-term incidence study for KD, which has a span of 38 years of KD incidence and its outcomes, almost the entire time that Kawasaki Disease has been recognized as a diagnosis since 1967 [1]. We have assessed a well-defined, predominantly White population within the Midwestern region of the U.S., a region in which incidence of KD has not been studied for almost 30 years, since Windsor et al. in 1991 [21]. The overall incidence of Kawasaki Disease over a 38-year period in the Midwestern community with a predominantly White population appears to be stable since 1994. However, the incidence of KD among children 1–5 years old and females seems to have significantly increased.
Incidence of Kawasaki Disease
Our study results indicate that the overall incidence of KD in Olmsted County, MN appears to be stable since 1994, as shown in Fig. 1. Nationwide studies by Holman et al. have shown that annual incidence rates in the U.S. have remained relatively constant between 1997–2007 except for a peak in 2005, [11, 22] whereas our study demonstrated a peak incidence rate in 1994 followed by a plateau. Also, we did not observe any increased incidence of KD during and after the 2009 H1N1 pandemic suggesting the 2009 H1N1 does not cause MIS observed in COVID-19.
The incidence of KD among children 1–5 years old seems to have increased over time as depicted in Fig. 2. Sun et al. similarly described a recent increase in incidence of KD among patients 1–5 years old in China in 2017 [23]. The annual incidence rates found in this study for all ages and < 5 years were 9.84 and 21.37 per 100,000 person-years, respectively. These are similar to that of short-term U.S. nationwide studies, such as Holman et al. described as 20.8 per 100,000 for children < 5 years old in 2006 [11]. Most studies in the U.S. have assessed KD incidence in minority populations in major urban centers with similar incidence rates around 20 per 100,000, [4, 5, 8, 10, 12, 13, 24, 25] indicating that incidence in predominantly White populations are not necessarily lower than in minorities.
Interestingly, our study shows a stable incidence in males but an increasing incidence in females (Fig. 3), which is a novel finding that has not been reported in any prior studies. Burgner et al. reported on the epidemiology of KD exhibiting a male to female ratio of about 1.6:1 [26] which is consistent with our overall finding, and Sun et al. described a stable overall male to female ratio of about 1.75:1, with the highest between 6 and 11 months of life (2.06:1). [23] Okubo et al. described an overall male to female ratio of 1.35–1.42:1 in the US with no increase in female to male ratio up to 2012. [14] The increasing incidence in females is a novel finding of our study that warrants further investigation for the cause of this trend, and awareness of this finding among clinicians. The reason for this increase in incidence among females rather than males is not clear, and theinvestigations with larger sample sizes to help guide the discussion of this finding will be needed.
Cardiac Complications
Kawasaki Disease is the leading cause of acquired heart disease in children of developed nations. Most studies demonstrate that one quarter of patients develop coronary artery abnormalities, [2] which is consistent to our study findings. Of the patients in our study who developed cardiac complications recognized during the episode of KD and in the short term follow up, 78.6% were males (vs. 61.3% male in the cohort), and 17.2% were of Asian descent (vs. 8.9% Asian in cohort) (although this was not statistically significant). Regarding age ranges, younger patients were at highest risk, with 62.1% of complications developing in patients who were between the ages of 1–5 years old (vs. 57.3% aged 1–5 in cohort), and 34.5% being less than 2 years old (vs. 20% aged < 2 in cohort).
Okubo et al. studied the development of coronary artery aneurysms in KD patients in the West Coast from 2003–2012, and demonstrated a rate as low as 2–3%, [14] compared to the general 20–25% rates in the literature. [2] Okubo et al.’s findings were based on ICD-9 codes for coronary artery aneurysms rather than including general coronary artery abnormalities such as ectasia and periluminal thickening as our study found. However, our study revealed that there were no coronary artery aneurysms in our patients from 2009–2016, conveying a decrease in development of aneurysms in recent years.
We found 24% of patients had received no treatment, and 24% also had developed cardiac complications. On further review, we found that these were different patient groups. Treatment with IVIG was administered in 96.6% of patients who developed cardiac complications, and aspirin to 100% of patients who developed cardiac complications. Patients who did not receive any treatment were often followed up on an outpatient basis rather than hospitalized. Interestingly, Kibata et al. reported a potential for genetic IVIG resistance that might explain why some patients did not respond to treatment and develop coronary abnormalities. [27] They also described an increase of IVIG-resistant patients from 7 to 23% within the last decade in Japan, consistent with our finding of 24% of patients developing coronary artery abnormalities despite IVIG treatment. Regarding the trend of cardiac complications with seasons, this was the same as the findings with incidence of KD, as winter and spring exhibited the highest rates of cardiac complications (P = 0.66 for seasonality; P = 0.03 for monthly variation). In general the literature has not found statistically significant associations between seasonality and KD.
Strengths
The main strength of our study is a population-based design which minimized selection bias, because most previous studies for KD incidence used hospitalization associated with KD to estimate incidence, rather than population-based all-incident cases of KD as in our study. Because previous studies used ICD-9 codes associated with hospitalization to identify KD cases, [4, 5, 11, 14, 22, 24] patients who were treated as outpatients might be omitted in estimating the incidence of KD by previous studies, leading to an underestimation. We used reliable ascertainment of KD with comprehensive medical record review and predetermined criteria based on AHA guidelines of KD diagnosis. Most retrospective studies did not confirm cases via manual chart review which might cause misclassification. For example, our study excluded 57 cases (31.5%) out of 181 potential cases that were misclassified as KD. Finally, our study has important epidemiological advantages in estimating an accurate incidence of disease: (1) our study setting is virtually self-contained (only two health care sites provide medical care to all Olmsted County, MN residents); (2) patients’ medical records of the two sites are linked through the REP; and 3) almost all (> 95%) of Olmsted County residents authorize using medical records for research.
Limitations
There are inherent limitations for our study as a retrospective study. This is a single-center study with a small sample size despite its population-based design. It is possible that during the early decades of this study time period, cases were missed, particularly because in the early days when the concept of this disease was introduced, it was recognized as a disease that occurs mainly in Asians, and KD was not considered as a high priority in differential diagnosis. While our results provide an important insight into the incidence of KD in the community with a predominantly White population given the lack of this epidemiological data, our findings might not be generalizable or extrapolated to other study settings, particularly with more diverse ethnic compositions. However, it has been known that age, sex, and ethnic characteristics of residents from Olmsted County, MN (where this study was conducted) are similar to those of the state of Minnesota and the Upper Midwest, and thus, we expect that these study results will be generalizable to those regions with similar characteristics.1 Also, not all patients had multiple longitudinal echocardiographs as recommended and thus, our study might have missed some long-term outcomes of KD.
Conclusion
The overall incidence of Kawasaki Disease over a 38-year period in the Midwest community with a predominantly White population appears to be stable since 1994. However, the incidence of KD among children 1–5 years old and females seems to have significantly increased. Further studies identifying potential factors driving these upward trends of KD in high-risk subgroups identified in our study are warranted.
Data Availability
The datasets generated and/or analyzed during the current study are not publicly available as they include protected health information. Access to data could be discussed per the institutional policy after IRBs at Mayo Clinic and Olmsted Medical Center approve it.
Abbreviations
- KD:
-
Kawasaki Disease
- REP:
-
Rochester Epidemiology Project
- IVIG:
-
Intravenous immunoglobulin
- AHA:
-
American Heart Association
References
Kawasaki T (1967) Acute febrile mucocutaneous syndrome with lymphoid involvement with specific desquamation of the fingers and toes in children. Arerugi 16(3):178–222
Cohen E, Sundel R (2016) Kawasaki disease at 50 years. JAMA Pediatrics 170(11):1093–1099
Davis RL, Waller PL, Mueller BA, Dykewicz CA, Schonberger LB. Kawasaki syndrome in Washington State. Race-specific incidence rates and residential proximity to water. Archives of Pediatrics & Adolescent Medicine. 1995;149(1):66–9.
Callinan LS, Holman RC, Vugia DJ, Schonberger LB, Belay ED (2014) Kawasaki disease hospitalization rate among children younger than 5 years in California, 2003–2010. Pediatric Infectious Disease Journal 33(7):781–783
Chang RK (2002) Epidemiologic characteristics of children hospitalized for Kawasaki disease in California. Pediatric Infectious Disease Journal 21(12):1150–1155
Cheung EW, Zachariah P, Gorelik M, Boneparth A, Kernie SG, Orange JS, et al. Multisystem Inflammatory Syndrome Related to COVID-19 in Previously Healthy Children and Adolescents in New York City. 2020.
Bronstein DE, Dille AN, Austin JP, Williams CM, Palinkas LA, Burns JC (2000) Relationship of climate, ethnicity and socioeconomic status to Kawasaki disease in San Diego County, 1994 through 1998. Pediatric Infectious Disease Journal 19(11):1087–1091
Belay ED, Holman RC, Clarke MJ, Destefano F, Shahriari A, Davis RL et al (2000) The incidence of Kawasaki syndrome in West Coast health maintenance organizations. Pediatric Infectious Disease Journal 19(9):828–832
Belay ED, Holman RC, Maddox RA, Foster DA, Schonberger LB (2003) Kawasaki syndrome hospitalizations and associated costs in the United States. Public Health Rep 118(5):464–469
Coustasse A, Larry JJ 3rd, Migala W, Arvidson C, Singh KP (2009) Kawasaki Syndrome in Texas. Hosp Top 87(3):3–10
Holman RC, Belay ED, Christensen KY, Folkema AM, Steiner CA, Schonberger LB (2010) Hospitalizations for Kawasaki syndrome among children in the United States, 1997–2007. Pediatric Infectious Disease Journal 29(6):483–488
Abuhammour WM, Hasan RA, Eljamal A, Asmar B (2005) Kawasaki disease hospitalizations in a predominantly African-American population. Clin Pediatr 44(8):721–725
Ichida F, Fatica NS, O’Loughlin JE, Klein AA, Snyder MS, Levin AR et al (1989) Epidemiologic aspects of Kawasaki disease in a Manhattan hospital. Pediatrics 84(2):235–241
Okubo Y, Nochioka K, Sakakibara H, Testa M, Sundel RP (2017) National survey of pediatric hospitalizations due to Kawasaki disease and coronary artery aneurysms in the USA. Clin Rheumatol 36(2):413–419
Melton LJ 3rd (1996) History of the Rochester Epidemiology Project. Mayo Clin Proc 71(3):266–274
St Sauver JL, Grossardt BR, Leibson CL, Yawn BP, Melton LJ 3rd, Rocca WA (2012) Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clin Proc 87(2):151–160
St Sauver JL, Grossardt BR, Yawn BP, Melton LJ 3rd, Pankratz JJ, Brue SM et al (2012) Data resource profile: the Rochester Epidemiology Project (REP) medical records-linkage system. Int J Epidemiol 41(6):1614–1624
Rocca WA, Yawn BP, St Sauver JL, Grossardt BR, Melton LJ 3rd (2012) History of the Rochester Epidemiology Project: half a century of medical records linkage in a US population. Mayo Clin Proc 87(12):1202–1213
McCrindle BW, Rowley AH, Newburger JW, Burns JC, Bolger AF, Gewitz M et al (2017) Diagnosis, Treatment, and Long-Term Management of Kawasaki Disease: A Scientific Statement for Health Professionals From the American Heart Association. Circulation 135(17):e927–e999
St Sauver JL, Grossardt BR, Yawn BP, Melton LJ 3rd, Rocca WA (2011) Use of a medical records linkage system to enumerate a dynamic population over time: the Rochester epidemiology project. Am J Epidemiol 173(9):1059–1068
Windsor AM, Schell WL, Davis JP (1991) Kawasaki syndrome in Wisconsin. Wis Med J 90(5):227–231
Holman RC, Belay ED, Curns AT, Schonberger LB, Steiner C (2003) Kawasaki syndrome hospitalizations among children in the United States, 1988–1997. Pediatrics 111(2):448
Sun L, Tang Y, Wang Y, Qian G, Yan W, Wang B et al (2018) Changes in Profiles of Kawasaki Disease Noted over Time in Suzhou. China Cardiology 141(1):25–31
Holman RC, Shahriari A, Effler PV, Belay ED, Schonberger LB (2000) Kawasaki syndrome hospitalizations among children in Hawaii and Connecticut. Arch Pediatr Adolesc Med 154(8):804–808
Ghelani SJ, Sable C, Wiedermann BL, Spurney CF (2012) Increased incidence of incomplete Kawasaki disease at a pediatric hospital after publication of the 2004 American Heart Association guidelines. Pediatr Cardiol 33(7):1097–1103
Burgner D, Harnden A (2005) Kawasaki disease: what is the epidemiology telling us about the etiology? Int J Infect Dis 9(4):185–194
Kibata T, Suzuki Y, Hasegawa S, Matsushige T, Kusuda T, Hoshide M et al (2016) Coronary artery lesions and the increasing incidence of Kawasaki disease resistant to initial immunoglobulin. Int J Cardiol 214:209–215
Acknowledgements
We thank Kelly Okeson for her administrative support and the Precision Population Science Lab staff. The study was supported by National Institute of Health (NIH)-funded R01 grant (R01 HL126667).
Funding
The study was supported by National Institute of Health (NIH)-funded R01 grant (R01 HL126667).
Author information
Authors and Affiliations
Contributions
ENT and BSC made substantial contributions to the conception or design of the work, the acquisition, interpretation of data, drafted the manuscript, approved the version to be published, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. CW and YJJ made substantial contributions to the conception or design of the work, the acquisition, interpretation of data, revised the manuscript critically for important intellectual content, approved the version to be published, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. HYS made substantial contributions to the interpretation of data, revised the manuscript critically for important intellectual content, approved the version to be published, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. TGB and JNJ made substantial contributions to the conception or design of the work, interpretation of data, revised the manuscript critically for important intellectual content, approved the version to be published, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. ER and KSK made substantial contributions to the conception or design of the work, analysis and interpretation of data, revised the manuscript critically for important intellectual content, approved the version to be published, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
This study was supported by the NIH R01 HL126667. The authors have no financial relationships relevant to this article to disclose. The authors have no conflicts of interest relevant to this article to disclose.
Ethical Approval
This study protocol was approved by the institutional review boards at both Mayo Clinic and Olmsted County Medical Center.
Informed Consent
We included only those who granted research authorization for this study.
Consent for Publication
We included only those who granted research authorization for this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Taslakian, E.N., Wi, CI., Seol, H.Y. et al. Long-term Incidence of Kawasaki Disease in a North American Community: A Population-Based Study. Pediatr Cardiol 42, 1033–1040 (2021). https://doi.org/10.1007/s00246-021-02577-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-021-02577-2