Abstract
Cardiac allograft vasculopathy (CAV) is an obliterative and diffuse form of vasculopathy affecting almost 50% of patients after 10 years from heart transplant and represents the most common cause of long-term cardiovascular mortality among heart transplant recipients. The gold standard diagnostic technique is still invasive coronary angiography, which however holds potential for complications, especially contrast-related kidney injury and procedure-related vascular lesions. Non-invasive and contrast-sparing imaging techniques have been advocated and investigated over the past decades, in order to identify those that could replace coronary angiography or at least reach comparable accuracy in CAV detection. In addition, they could help the clinician in defining optimal timing for invasive testing. This review attempts to examine the currently available non-invasive imaging techniques that may be used in the follow-up of heart transplant patients, spanning from echocardiography to nuclear imaging, cardiac magnetic resonance and cardiac computed tomography angiography, weighting their advantages and disadvantages.
Similar content being viewed by others
Introduction
Cardiac allograft vasculopathy (CAV) is an obliterative and diffuse form of vasculopathy that can be considered as a late complication of heart transplant (HTx). It affects almost 50% of patients after 10 years from transplant and represents the most common cause of long-term cardiovascular mortality [1]. CAV is a distinct disease from coronary atherosclerosis, being characterized by endothelial injury [2], vascular cell proliferation, fibrosis and remodeling, and is triggered by both immune and non-immune factors. Pathophysiology of CAV is complex and not fully understood yet, involving recipient immunological response, cytomegalovirus infection, frequent episodes of acute rejection (especially antibody-mediated) and traditional cardiovascular risk factors.
Given the denervation of the cardiac allograft, CAV manifestations are often subtle, especially in early stages of disease. Invasive coronary angiography (ICA) still represents the gold standard for the diagnosis, especially when combined to intravascular ultrasound (IVUS) and optical coherence tomography (OCT) [3]. As an evidence, CAV is currently classified according to the International Society of Heart and Lung Transplantation (ISHLT) criteria, which are based on either angiographic findings and evidence of graft dysfunction, i.e., reduced left ventricular ejection fraction (LVEF) and/or restrictive filling pattern (Table 1). CAV is then graded as absent (CAV0), mild (CAV1), moderate (CAV2) and severe (CAV3), accordingly [4].
ICA is the gold-standard method used to routinely screen HTx patients, even in the absence of left ventricular dysfunction or symptoms. However, despite its demonstrated safety, ICA holds potential for severe complications, including contrast-related kidney injury and procedure-related vascular lesions [5], with also a low sensitivity per se in detecting early CAV and a limited role in its treatment. Moreover, HTx recipients are a fragile and multi-comorbid population that often presents with renal dysfunction, mainly due to pre-HTx cardiorenal syndromes and immunosuppressive regimens [6]. Given this background, non-invasive and contrast-sparing imaging techniques have been reconsidered and investigated over the past decades, in order to identify those that could represent an alternative to ICA or at least reach comparable accuracy in CAV detection. In addition, they should provide useful information for establishing the optimal timing of ICA, further limiting its use to patients with high suspicion of CAV. This review attempts to examine the available non-invasive imaging techniques that may be used in the follow-up of HTx patients, weighting their advantages and disadvantages (Fig. 1).
Central illustration. This figure shows the different parameters that could be assessed with each non-invasive imaging modality. The sensitivity of each parameter tends to decrease from the outer layers to the inner ones. CAC: coronary artery calcium; CAV: cardiac allograft vasculopathy; CCTA: cardiac computed tomography angiography; CMR: cardiac magnetic resonance; DS: dobutamine-stress ECD: echocardiography; GLS: global longitudinal strain: LVEF: left ventricular ejection fraction; MBF: myocardial blood flow; PET: positron emission tomography; SPECT: single-photon emission computed tomography; WMAs: wall motion abnormalities
Echocardiography
Rest echocardiography
Resting echocardiography provides limited diagnostic accuracy for CAV detection, particularly in mild forms [7–11]. The latest standardized protocol for the assessment of HTx patients includes the quantification of both diastolic and systolic function, mainly through mitral inflow Doppler velocities, LVEF and wall motion abnormalities (WMAs) [4].
Left ventricular ejection fraction
LVEF is often at the upper limit of normal due to either graft denervation and increased levels of circulating catecholamines, and is generally preserved even in advanced forms of CAV, making it unsuitable as an early marker of disease. David et al. showed that patients with severe forms of CAV were characterized by lower values of LVEF and a higher prevalence of grade 2 and 3 diastolic dysfunction as compared with less severe forms of disease (52% vs 62%, p < 0.05 and 75% vs 11%, p < 0.05 respectively), although LVEF was found to be preserved in the majority of them [12]. In the first years after HTx, a reduction in LVEF should be addressed more commonly to acute rejection and less commonly to CAV, while its occurrence years later might point towards CAV progression [13], stressing the role of LVEF as one of the strongest predictors of outcome in HTx [14].
Diastolic dysfunction
The course of diastolic function of the transplanted heart usually presents as bimodal: in the very early phase, relevant left ventricular relaxation disturbances can be observed, even in the absence of acute rejection or CAV [7, 15, 16]; then, they attenuate after the first month. Later on, a worsening in diastolic function during follow-up should point at the possibility of acute rejection or development and/or progression of CAV (Fig. 2), deeming an invasive diagnostic approach necessary [17]. Nonetheless, this bimodal pattern was not considered in the current ISHLT classification of CAV, as a restrictive filling pattern is regarded as a grade 3 graft dysfunction, independently of the time of observation [4].
Diastolic dysfunction in presence of cardiac allograft vasculopathy. The left picture shows a normal diastolic function, as indicated by pulsed wave trans-mitral Doppler velocities and deceleration time of E wave, in a heart transplant patient without cardiac allograft vasculopathy. On the other hand, the right picture shows a restrictive diastolic pattern in presence of grade 3 cardiac allograft vasculopathy
Wall motion abnormalities
The onset of new regional WMAs should raise suspicion towards the presence or the progression of CAV [18], thus warranting for further tests. However, these findings are not specific, as WMAs might develop even in the absence of CAV or acute rejection, especially several years after HTx [3].
Due to the development of new echocardiographic techniques, it is now possible to assess myocardial deformation, especially left ventricular (LV) global longitudinal strain (GLS) through both tissue Doppler imaging (TDI) and speckle tracking echocardiography, the latter being more angle-independent. Compared to visually assessed WMAs, wall motion velocity analysis assessed by TDI has been proven to detect earlier ventricular dysfunction [7, 19–21]. CAV patients seem to have augmented durations and reduced amplitudes of both systolic and diastolic TDI-myocardial velocities [3]. For instance, a value of radial systolic TDI-derived velocity ≤ 10 m/s showed a sensitivity of about 90% for angiographic and/or IVUS detectable CAV, but the sensitivity decreased down to 51% when investigating main epicardial vessels stenoses, even when with a 9 cm/s cut-off [18]. However, also tissue Doppler velocities at rest are more frequently indicative of advanced stages of CAV [22], and a recent study found no differences in myocardial deformation as assessed by strain analysis among normal and abnormal segments [23].
LV-GLS is less dependent on heart rate and loading conditions as compared to LVEF and other diastolic indexes [24, 25]. The endomyocardial fibers are predominantly oriented longitudinally and represent those more susceptible to the ischemic insult, either macrovascular and microvascular. In this regard, several studies have shown a correlation between a reduced absolute value of LV-GLS and the presence of CAV and coronary microvascular dysfunction (Fig. 3) [26–28]. Clemmensen et al. found a statistically significant correlation, and a significant reduction of LV-GLS among patients with no and mild CAV (CAV0 vs CAV1), as well as a preserved LVEF even in presence of moderate-to-severe CAV [26]. Furthermore, another study attested the association of LV circumferential strain reduction to the presence of proximal coronary stenosis (positive and negative predictive value ≥ 90%, considering proximal stenosis as ≥ 50%) [29]. In addition to that, a recent study based on a small cohort of heart transplanted patients, excluding grade 3 CAV, suggested that layer-specific LV-GLS and the gradient between endocardial and epicardial longitudinal strain values could be relevant non-invasive predictors of CAV [30]. At last STE is angle-dependent and may help in the identification of LV dyssynchrony, as it can spot regional differences in LV dysfunction [20, 26, 31–33]. Indeed, patients with CAV3 showed a reduced absolute value of LV-GLS and a higher LV longitudinal strain time to peak, highlighting a more severe degree of LV dyssynchrony [34].
Left ventricular global longitudinal strain and cardiac allograft vasculopathy. This picture shows left ventricular longitudinal strain and three-layer specific longitudinal strain in three different heart transplant patients, with grade 3 cardiac allograft vasculopathy (CAV), with grade 1 CAV and without CAV, from left to right respectively. Left ventricular longitudinal strain assessed in apical 4-chamber view appears significantly reduced in presence of diffuse CAV, whereas it is almost comparable to normal subjects in the absence of this complication
Stress echocardiography
In the general population, exercise should be the preferred stressor when stress echocardiography is performed. Nonetheless, physical exercise might not represent an adequate cardiovascular stressor for the denervated allograft, mostly because of impaired chronotropic response [10, 35–37]. Thus, in this population of patients, stress echocardiography with pharmacological agents seems to be more favorable when this technique is indicated. However, a recent study highlighted that exercise could still represent a more efficient stressor compared to dobutamine in transplanted patients that prefer and can perform exercise stress echocardiography [38].
As concerns pharmacological agents, dobutamine stress echocardiography (DSE) represents the preferred choice [39, 40]. Unfortunately, the target heart rate may not be easily reached in some patients, and the additional use of atropine is of limited value as opposed to general population [41, 42]. In these cases, a pre-test screening with donor-recipient age difference may be considered, as it directly affects the likelihood of reaching the target heart rate [43]. Even though some studies proved good sensitivity and specificity of dipyridamole stress echocardiography in detecting CAV [39, 40], DSE still represent the first choice.
The latest ISHLT guidelines recommend dobutamine or treadmill stress echocardiography in patients who cannot undergo invasive testing (class of recommendation IIaB) [44]. In particular, these exams are routinely used in patients with or at high risk of progression of chronic kidney disease. Still, the role of DSE in the diagnosis of CAV is controversial, especially with regards to recognition of early CAV. In fact, DSE detects angiographically evident CAV [45] with a sensitivity of 70–80% that is even lower when IVUS is performed during ICA (72–79%) [46]. Furthermore, two recent studies reported a low sensitivity especially with regards to mild CAV [48, 47]. Likewise, a recent meta-analysis confirmed an insufficient sensitivity (60.2%) of DSE in the detection of CAV, despite higher specificity (85.7%) [49]. Clerkin et al. also demonstrated that DSE was not able to detect mild nor moderate CAV in the first 5 years after HTx [47].
The accuracy of stress echocardiography might improve if combined with other techniques, such as myocardial deformation analysis and the use of contrast agents. For instance, strain analysis can increase DSE sensitivity from 63 to 88% in the detection of CAV [5051], representing a promising tool in the detection of CAV.
Cardiac computed tomography angiography (CCTA)
Cardiac computed tomography angiography (CCTA), as most of the below-mentioned techniques, has proved useful in the diagnosis of non-allograft coronary artery disease, with the highest benefit in patients with low-to-intermediate risk of disease [52].
Regarding CAV, many concerns with the feasibility of CCTA have been raised. In particular, denervated hearts usually show elevated heart rates at rest [53]. This point, together with the common presence of impairment in renal function from multiple etiologies, may limit its use. Indeed, HTx patients are often under nephrotoxic, immunosuppressive drugs, and contrast agents may precipitate acute kidney injury. Then, if CAV is suspected, ICA becomes mandatory and further iodinated contrast is required. In spite of these issues, new modalities in CCTA (i.e., dual source, multi-segment reconstruction and motion correction algorithms) may increase its diagnostic accuracy, making this technique more appealing and useful in spite of the above-mentioned pitfalls [54].
In 2005, first evidences stated that CCTA may be used as a screening tool in HTx recipients for de novo CAV or as a follow-up strategy [55]. Furthermore, it detects an intimal maximal thickness (IMT) > 0.5 mm as well as IVUS, thus being more sensitive than ICA [56].
The use of multi-slice machines significantly improved the diagnostic accuracy of the technique. In a pilot study on 10 patients using 16-slice CCTA, the detection of inflammatory plaques (defined as > 30% necrosis and presence of calcium) well correlated with IVUS-derived virtual histology [57]. 64-slice was reasonably superior to 16-slice CCTA, in particular with regards to sensitivity and negative predictive value (NPV): it correctly evaluated 95% of ≥ 2 mm segments, with 100% sensitivity and NPV in finding significant, invasively treatable stenoses (> 50%) [5859] (Fig. 4). Conversely, this technique was inaccurate in the evaluation of subtle CAV and yielded more radiation exposure than ICA (19 mSv vs. 5.7 mSv).
Invasive coronary angiography vs coronary computed tomography angiography. Presence of coronary allograft stenosis in proximal-middle left anterior descending artery (LAD, continuous arrows) and proximal circumflex artery (LCx, dashed arrow), as detected by either invasive coronary angiography (ICA) and 64-slice multidetector computed tomography (MDCT). ICA, invasive coronary angiography; LAD, left anterior descending artery; LCx, left circumflex artery; MDCT, multidetector computed tomography. Adapted from Nunoda S et al., 2010 (10.1253/circj.cj-09–0800) [84]
Whether CCTA proved overall applicable to CAV, the quantification of coronary artery calcium (CAC) showed heterogeneous results. First evidences stated that the only absence of CAC was not reliable enough to exclude CAV [60], confirming a previous study that demonstrated that CAC score was not valid to make diagnosis [61]. Instead, a high score may suggest the presence of pre-existing or de novo allograft atherosclerotic lesions. However, recent findings showed a 97% NPV in excluding moderate-to-severe CAV and 88% NPV in excluding significant stenosis at ICA [62]; patients with CAC also had more events than those without it. These data are in support of a 2012 systematic review that found 99% NPV and high sensitivity for CAC in the diagnostic workup of CAV [63].
Several parameters from CCTA—as well as their combination—may be useful in the prediction and the identification of early CAV: volume/length ratio of the plaque, wall burden and the proportion of fibrotic/fibro-fatty/calcified/low-attenuation tissue [63]. The spread of advanced technique, such as the evaluation of fractional flow reserve using computed tomography, although not tested yet in heart transplant patients, may help in defining the functional significance of a coronary stenosis, without recurring to ICA.
Nuclear imaging
Single-photon emission computed tomography
While the role of single-photon emission computed tomography (SPECT) is well established in the diagnosis of non-allograft coronary artery disease, its role in the diagnostic workup of CAV is way less clear. In patients with inadequate acoustic window and contraindication to contrast agents, pharmacological SPECT could represent an alternative imaging technique for CAV detection. Globally, the use of pharmacological stressors is preferred over physical exercise, and gated technique can improve sensitivity [64]. Many tracers have been tested in the context of CAV, with a solid role in prognostic stratification and a more questionable role in diagnosis.
SPECT has a high NPV, especially when combined with a normal wall motion pattern, but low specificity and sensitivity for milder cases of CAV, wherein LVEF is still preserved. This may be explained by the diffuse, balanced distribution of ischemia in CAV, as it is not territory-related [65]. In these cases, a global reduction in color-contrast may be missed, thus leading to false negatives. 99mTc-tetrofosmin-gated adenosine stress SPECT was not found to be sensitive in detecting CAV, even when stricter criteria of ≥ 70% stenosis were applied [66]. Some clues may help in distinguishing between true and false negatives, in particular a lung/heart ratio > 0.37 during stress independently predict CAV even in cases of preserved LVEF, often involving main coronary branches [67]. This evidence implies that SPECT might not be ideal for early CAV detection, but it might be useful to exclude severe disease or to delay ICA, particularly in patients with previously normal epicardial coronary arteries.
As for what concerns the prognostic value of SPECT, data are more encouraging, as many studies showed that a negative stress SPECT is associated with better outcome. For instance, the presence of wall motion abnormalities together with a positive stress SPECT can predict cardiac events [67]. Manrique et al. demonstrated that a > 3 segments defect during stress could predict late revascularization at > 2 months [68]. Patients with a negative stress-SPECT with 99mTc have a high NPV for major events at 12 months [69], and this trend is maintained at a 5-year evaluation [70]. Accordingly, a negative gated SPECT test holds a low risk of major cardiovascular events [68]. Large though reversible defects demonstrated to predict death [66]. In contrast, a heterogeneous uptake of tracer using SPECT showed to predict allograft dysfunction, but it was not associated with future major cardiac events and reduced survival [71].
Positron emission tomography
The study of perfusion using positron emission tomography (PET) shows more accuracy as compared with SPECT in the diagnostic workup of non-allograft coronary artery disease [72]. This seems to apply also to the setting of CAV: the study of myocardial blood flow (MBF) can reveal the diffuse, non-segment specific nature of CAV, with earlier identification of the disease [73]. In fact, MFR assesses both macro- and microvascular function, rather than relying solely on an anatomic characterization of CAV. In the last years, growing evidence has been collected to support the use of cardiac PET in non-invasive surveillance for CAV, with recent guidelines incorporating recommendations for this technique [74].
The first evidence comes from an outdated study by Allen-Auerbach et al., whom demonstrated that endothelial-independent MBF abnormalities were related to morphological indexes of CAV progression with IVUS [75]. 13NH3-PET with quantification of MBF provided improved detection of CAV, and valid stratification of severity, representing a strong predictor of major cardiac events [76] (Fig. 5). In a comparison study among PET, IVUS and ICA, 82Rb-dipiridamole PET test demonstrated that the reduction in MBF and the concurrent increase in coronary resistance were highly suggestive of CAV, with > 96% specificity [77]. Moreover, myocardial flow reserve quantification using 13NH3 was inversely related to the volume of coronary plaques as estimated by IVUS, also when ICA was negative [78]. Despite this evidence, there are not available universally accepted PET flow thresholds for CAV detection, therefore more studies are warranted in order to standardize this promising technique in the early identification of CAV in HTx patients.
Myocardial blood flow quantification positron emission tomography. Inferolateral reduction in myocardial blood flow (MBF), suggestive of significant CAV in left circumflex artery (LCx), and milder degrees of myocardial ischemia during peak hyperemia, suggestive of diffuse CAV. ICA, invasive coronary angiography; LAD, left anterior descending artery; LCx, left circumflex artery; LM, left main artery; LV, left ventricle; LVEF, left ventricular ejection fraction; MBF, myocardial blood flow; OM, obtuse marginal; RV, right ventricle. Adapted from Bravo PE et al., 2018 (10.1093/eurheartj/ehx683) [8776]
PET imaging may also allow vascular wall evaluation, as a case report in 2016 demonstrated that 18fluorodeoxyglucose (FDG)-PET detected vascular inflammation before the onset of alterations on ICA, still using IVUS as gold standard [79]. This is line with pathophysiologic aspects of CAV, as inflammation either due to immunologic and non-immunologic factors is a leading driver of vascular impairment [80].
PET still holds prognostic information, according to several studies. Myocardial flow reserve ≤ 1.75 using 82Rb-dipiridamole PET was found to be related to increased rate of major cardiac events, also in the setting of preserved LVEF and normal perfusion [81]. The quantification of coronary flow reserve using the same tracer was also able to predict long-term outcome [82].
Cardiac magnetic resonance
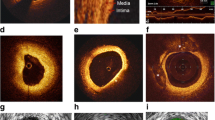
Cardiac magnetic resonance (CMR) represents a useful resource in the assessment of both structural and functional changes, providing also information regarding the composition of myocardial tissue. In fact, in patients with insufficient acoustic window, CMR is an alternative to echocardiography to assess cardiac chamber volumes and function as well as to exclude acute cellular rejection. In fact, its role in HTx patients has been more intensively studied with regards to acute cellular rejection, since first studies in CAV showed low sensitivity [838584] (Fig. 6). First encouraging data derive from the analysis of the peak filling rate, which is an estimate of diastolic function, whose values were lower in advanced CAV rather than in earlier stages. Indeed, early diastolic strain rate impairment was successively associated to microvascular dysfunction [86], while LVEF, stroke volume and cardiac output may be found normal either in early and late stages [87]. These results might hint that diastolic dysfunction in this population might be more sensitive than indexes of systolic function for the precocious detection of CAV.
Invasive coronary angiography vs cardiac magnetic resonance. Evidence of diffuse wall thickening in the distal left anterior descending artery (LAD) and stenosis in the left circumflex artery (LCx), as revealed by invasive coronary angiography (ICA). Cardiac magnetic resonance (CMR) did not detect any of these defects. CMR, cardiac magnetic resonance; ICA, invasive coronary angiography; LAD, left anterior descending artery; LCx, left circumflex artery. Adapted from Nunoda S et al., 2010 (10.1253/circj.cj-09–0800) [84]
Microvascular disease can be assessed by stress perfusion CMR, through the estimate of myocardial perfusion reserve (MPR), even though first results were not encouraging in detecting CAV [84], later ones showed promising findings due to the fact that diffuse CAV can affect the microvasculature independent of lesions in the epicardial vessels. In fact, further and more detailed studies about MPR reported a lower index in those with an IMT ≥ 0.5 mm as found with IVUS, with a moderate inverse relationship [88]. MPR ≤ 1.68 has a 100% sensitivity and 100% NPV in detecting CAV, but still has low specificity (63%). This index, as well as GLS, is altered years after HTx, and should be attributable to CAV rather than to fibrosis or graft rejection [89]. Also, MPR assessed by multiparametric CMR outperformed ICA for the detection of moderate CAV in a study by Miller et al. [90].
Microvascular reactivity has also been studied by oxygenation-sensitive CMR with a protocol of 1-min hyperventilation, followed by 30 s of apnea [91]. Significant differences were found between CAV and non-CAV HTx recipients, but intriguingly this difference was maintained between mild/absent and moderate-to-severe CAV. Unfortunately, its usefulness was questioned in presence of interstitial fibrosis, but fibrosis in turn may indicate a more advanced stage of disease. This analysis might provide key information without using a stressor nor a contrast agent.
As mentioned above, contrast-enhanced CMR with gadolinium is able to identify portions of myocardium characterized by inflammation, scarring and diffuse fibrosis, which could provide valid help in serial assessment of adverse cardiac remodelling as well as strong prognostic value. Late gadolinium enhancement imaging has been widely proven to be a prognosticator in HTx patients [92], even though diffuse myocardial changes might be missed. In this context, recent techniques such as T1- and T2-mapping have been investigated in this population. Latest studies demonstrated that T2-weighted sequences can predict outcome at multivariate analysis, whilst extracellular volume and pre-contrast T1-weighted sequences tend to remain stable [93]. Perhaps, damage onset is an early finding in CAV, but tend to remain stable over time. Extracellular volume was shown to be related to vascular stenosis at ICA and to fibrosis at endomyocardial biopsy analysis; T1-relaxation time, instead, correlates only to the grade of stenosis at ICA, and IMT only to the grade of fibrosis at biopsy. With these premises, further studies should focus on whether extracellular volume is a precocious sign of CAV-induced fibrosis.
Conclusions
The identification of CAV, especially with regard to early disease, represents a puzzling challenge for cardiologists. ICA is still the gold standard in the diagnosis of this long-term, survival-limiting disease, but does not show high sensitivity nor is free from complications. Non-invasive and more sensitive techniques are an appealing field but are still quite nebulous. To date, no technique—ICA included—is able to interpret the diffuse and subtle nature of CAV, so that such new techniques are expected to point out early alterations in vessel walls and significative early metabolic alterations for CAV. Echocardiography is a low cost, widely available technique but with limited sensitivity; the use of speckle tracking techniques may improve its diagnostic power. CCTA showed a good accuracy, but results concerning the detection of subtle CAV are controversial; the combination of multiple parameters as well as the development of sophisticated acquisitions may help in the diagnosis of earlier forms. Nuclear imaging, especially PET, will likely help in the management of HTx patients with suspected CAV, with a shift from anatomic to metabolic assessment. Nonetheless, radiation issues still limit its large-scale feasibility. MPR as assessed by CMR is promising, but anatomical vessel definition is scarce; further studies are deemed to state whether the evaluation of the extracellular volume may be an early sign of CAV. Studies regarding the combination of imaging techniques are strongly required, as their complementary nature may increase the overall sensitivity for CAV, thus limiting the need for invasive, periodic follow-ups.
Abbreviations
- CAC:
-
Coronary artery calcium
- CAV:
-
oronary allograft vasculopathy
- CCTA:
-
Cardiac computed tomography angiography
- CMR:
-
Cardiac magnetic resonance
- DSE:
-
Dobutamine stress echocardiography
- GLS:
-
Global longitudinal strain
- HTx:
-
Heart transplant
- ICA:
-
Invasive coronary angiography
- ISHLT:
-
Nternational Society of Heart and Lung Transplantation
- IMT:
-
Intimal maximal thickness
- IVUS:
-
Intravascular ultrasounds
- LVEF:
-
Left ventricular ejection fraction
- MBF:
-
Myocardial blood flow
- MPR:
-
Myocardial perfusion reserve
- NPV:
-
Negative predictive value
- PET:
-
Positron emission tomography
- SPECT:
-
Single-photon emission computed tomography
- TDI:
-
Tissue Doppler imaging
References
Lund LH, Edwards LB, Kucheryavaya AY, Benden C, Christie JD, Dipchand AI, Dobbels F, Goldfarb SB, Levvey BJ, Meiser B, Yusen RD, Stehlik J (2014) The Registry of the International Society for Heart and Lung Transplantation: Thirtieth Official Adult Heart Transplant Report--2013; focus theme: age. International Society of Heart and Lung Transplantation. J Heart Lung Transplant 33(10):996–1008
Chih S, Chong AY, Mielniczuk LM, Bhatt DL, Beanlands RS (2016) Allograft Vasculopathy: The Achilles’ Heel of Heart Transplantation. J Am Coll Cardiol 68(1):80–91
Thorn EM, de Filippi CR (2007) Echocardiography in the cardiac transplant recipient. Heart Fail Clin 3(1):51–67
Mehra MR, Crespo-Leiro MG, Dipchand A et al (2010) International Society for Heart and Lung Transplantation working formulation of a standardized nomenclature for cardiac allograft vasculopathy. J Heart Lung Transpl 29:717–27
Tavakol M, Ashraf S, Brener SJ (2012) Risks and complications of coronary angiography: a comprehensive review. Glob J Health Sci 4(1):65–93
González-Vílchez F, Vázquez de Prada JA (2014) Chronic renal insufficiency in heart transplant recipients: risk factors and management options. Drugs 74(13):1481–94
Wu HA, Kolias TJ (2012) Cardiac Transplantation: Pretransplant and Posttransplant Evaluation. In Otto CM ed. The Practice of Clinical Echocardiography, 4th Eds. 585–596
Spes CH, Klaus V, Mudra H et al (1999) Diagnostic and prognostic value of dobutamine stress echocardiography for noninvasive assessment of cardiac allograft vasculopathy: a comparison with coronary angiography and intravascular ultrasound. Circulation 100:505–515
Waggoner AD, Bierig MS (2001) Tissue Doppler imaging a useful echocardiographic method for the cardiac sonographer to assess systolic and diastolic function. J Am Soc Echocardiogr 12:1143–1152
Collings CA, Pinto FJ, Valentine HA (1994) Exercise echocardiography in heart transplant recipients: a comparison with angiography and intracoronary ultrasonography. J Heart Lung Transplant 13(4):604–613
Smart FW, Balantyne CM, Cocanougher B et al (1991) Insensitivity of noninvasive tests to detect coronary artery vasculopathy after after heart transplant. Am J Cardiol 67(4):243–247
Daud A, Xu D, Revelo MP, Shah Z, Drakos SG, Dranow E, Stoddard G, Kfoury AG, Hammond MEH, Nativi-Nicolau J, Alharethi R, Miller DV, Gilbert EM, Wever-Pinzon O, McKellar SH, Afshar K, Khan F, Fang JC, Selzman CH, Stehlik J (2018) Microvascular Loss and Diastolic Dysfunction in Severe Symptomatic Cardiac Allograft Vasculopathy. Circ Heart Fail (8):e004759
Chirakarnjanakorn S, Starling RC, Popović ZB, Griffin BP, Desai MY. Dobutamine stress echocardiography during follow-up surveillance in heart transplant patients: Diagnostic accuracy and predictors of outcomes. J Heart Lung Transpl 34:710–7
Barbir M, Lazem F, Banner N, Mitchell A, Yacoub M (1997) The prognostic significance of non-invasive cardiac tests in heart transplant recipients. Eur Heart J 18:692–696
Kobashigawa JA (2001) Heart Transplantation. In: Norman DJ, Turka LA, eds. Primer on Transplantation, 2nd edition, Mt. Laurel, N J Am Soc Transpl 321–66
Zengin E, Westermann D, Radunski U et al (2015) Cardiac mechanics in heart transplant recipients with and without transplant vasculopathy. Int J Cardiovasc Imaging 31(4):795–803
Lunze FI, Colan SD, Gauvreau K et al (2013) Tissue Doppler imaging for rejection surveillance in pediatric heart transplant recipients. J Heart Lung Transplant 32:1027–1033
Störk S, Behr TM, Birk M, Uberfuhr P, Klauss V, Spes CH, Angermann CE (2006) Assessment of Cardiac Allograft Vasculopathy Late After Heart Transplantation: When Is Coronary Angiography Necessary? J Heart Lung Transplant 25(9):1103–1108
Dandel M, Hummel M, Müller J et al (2001) Reliability of tissue Doppler monitoring after heart transplantation for replacement of invasive routine screenings by optimally timed cardiac biopsies and catheterizations. Circulation 104(12):I184–I191
Pan C, Wang C, Pan W et al (2011) Usefulness of real-time three-dimensional echocardiography to quantify global left ventricular function and mechanical dyssynchrony after heart transplantation. Acta Cardiol 66(3):365–370
Sutherland G, Steward M, Grondstroen K et al (1994) Color Doppler myocardial imaging. A new technique for assessment of myocardial function. J Am Soc Echocardiogr 7:441–58
Dandel M, Hummel M, Meyer R, Müller J, Kapell S, Ewert R, Hetzer R (2002) Left ventricular dysfunction during cardiac allograft rejection: early diagnosis, relationship to the histological severity grade and therapeutic implications. Transpl Proc 34:2169–2173
Hummel M, Dandel M, Knollmann F, Muller J, Knosalla C, Ewert R et al (2001) Long-term surveillance of heart-transplanted patients: noninvasive monitoring of acute rejection episodes and transplant vasculopathy. Transplant Proc 33:3539–3542
Dandel M, Hetzer R (2009) Echocardiographic strain and strain rate imaging – Clinical applications Int J Cardiol 132:11–24
Logstrup BB, Andersen HR, Thuesen L et al (2013) Left ventricular global systolic longitudinal deformation and prognosis 1 year after femoral and apical transcatheter aortic valve implantation. J Am Soc Echocardiogr 26:246–254
Clemmensen TS, Løgstrup BB, Eiskjær H, Poulsen SH (2015) Evaluation of longitudinal myocardial deformation by 2-dimensional speckle-tracking echocardiography in heart transplant recipients: relation to coronary allograft vasculopathy. J Heart Lung Transplant 34:195–203
Clemmensen TS, Eiskjær H, Løgstrup BB, Tolbod LP, Harms HJ, Bouchelouche K, Hoff C, Frøkiær J, Poulsen SH (2016) Noninvasive detection of cardiac allograft vasculopathy by stress exercise echocardiographic assessment of myocardial deformation. J Am Soc Echocardiogr 29:480–490
Clemmensen TS, Løgstrup BB, Eiskjaer H, Poulsen SH (2016) Coronary flow reserve predicts longitudinal myocardial deformation capacity in heart-transplanted patients. Echocardiography 33:562–571
Dandel M, Hetzer R (2017) Post-transplant surveillance for acute rejection and allograft vasculopathy by echocardiography: Usefulness of myocardial velocity and deformation imaging. J Heart Lung Transplant 36(2):117–131
Sciaccaluga C, Mandoli GE, Sisti N, Natali MB, Ibrahim A, Menci D, D'Errico A, Donati G, Benfari G, Valente S, Bernazzali S, Maccherini M, Mondillo S, Cameli M, Focardi M (2021) Detection of cardiac allograft vasculopathy by multi-layer left ventricular longitudinal strain in heart transplant recipients. Int J Cardiovasc Imaging
Dandel M, Lehmkuhl H, Knosalla C, Grauhan O, Weng Y, Pasic M, Hetzer R (2008) Echocardiographic 2D-strain imaging for early detection of patients with focal coronary stenoses after heart transplantation. J Heart Lung Transpl 27(2 Suppl1):S95–96
Budhe S, Richmond ME, Gilbert J, Lai WW (2015) Longitudinal strain by speckle-tracking echocardiography in pediatric heart transplant recipients. Congenit Heart Dis 10:362–370
Dandel M, Wellnhofer E, Lehmkuhl H et al Early detection of left ventricular wall motion alterations in heart allografts with coronary artery disease: diagnostic value of tissue Doppler and two-dimensional (2D) strain echocardiography
Ghali MCZ, Stewart R, Ghali GZ, Blitzer W (2020) Two dimensional speckle tracking echocardiography detects cardiac allograft stage III vasculopathy in recipients of heart transplants with preserved systolic function. Acta Cardiol 31:1–11
Salles AF, Oliveira JA (2000) Adaptation to exercise following cardiac transplantation. Arq Bras Cardiol 75(1):70–90
Squires RW, Leung TC, Cyr NS et al (2002) Partial normalization of the heart rate response to exercise after cardiac transplantation: frequency and relationship to exercise capacity. Mayo Clin Proc 77(12):1295–1300
Quigg R, Salyer J, Mohanty PK, Simpson P (1998) Impaired exercise capacity late after cardiac transplantation: influence of chronotropic incompetence, hypertension, and calcium channel blockers. Am Heart J 136(3):465–473
Gebska MA, Williford NN, Schadler AJ, Laxson C, Alvarez P, Briasoulis A, Cadaret LM, Yumul-Non IKT, Kerber RE, Weiss RM (2020) Pharmacological vs Exercise Stress Echocardiography for Detection of Cardiac Allograft Vasculopathy. Mayo Clin Proc Innov Qual Outcomes 4(1):65–75
Ciliberto GR, Parodi O, Cataldo G et al (2003) Prognostic value of contractile response during high-dose dipyridamole echocardiography test in heart transplant recipients. J Heart Lung Transplant 22(5):526–532
Ciliberto GR, Massa D, Mangiavacchi M et al (1993) High-dose dipyridamole echocardiography test in coronary artery disease after heart transplantation. Eur Heart J 14(1):48–52
Flox A, Sanchez V, Delgado JF, Fernandez S, Tello R, Jimenez J, Garcia J, Gomez MA, Lombera F, Saenz de la Calzada C (2002) Is atropine infusion necessary to achieve the target heart rate in heart transplant patients during dobutamine stress echocardiography? Transpl Proc 34 3241–3242
Kociolek LK, Bierig SM, Herrmann SC, Labovitz AJ (2006) Efficacy of atropine as a chronotropic agent in heart transplant patients undergoing dobutamine stress echocardiography. Echocardiography 23383–387
Gibson PH, Riesgo F, Choy JB, Kim DH, Becher H (2015) Dobutamine stress echocardiography after cardiac transplantation: implications of donor-recipient age difference. Echo Res Pract 2(2):65–71
Costanzo MR, Dipchand A, Starling R, Anderson A et al (2010) The International Society of Heart and Lung Transplantation Guidelines for the care of heart transplant recipients. J Heart Lung Transplant 29(8):914–956
Badano LP, Miglioranza MH, Edvardsen T et al (2015) European Association of Cardiovascular Imaging/Cardiovascular Imaging Department of the Brazilian Society of Cardiology recommendations for the use of cardiac imaging to assess and follow patients after heart transplantation. Eur Heart J Cardiovasc Imaging 16:919–948
Clerkin KJ, Ali ZA, Mancini DM (2017) New developments for the detection and treatment of cardiac vasculopathy. Curr Opin Cardiol 32:316–325
RC. Clerkin KJ, Farr MA, Restaino SW, Ali ZA (2016) Mancini DM. Dobutamine stress echocardiography is inadequate to detect early cardiac allograft vasculopathy. J Heart Lung Transpl 35(8):1040–1
Akosah KO, Mohanty PK, Funai JT et al (1994) Noninvasive detection of transplant coronary artery disease by dobutamine stress echocardiography. J Heart Lung Transplant 13:1024–1038
Elkaryoni A, Abu-Sheasha G, Altibi AM, Hassan A, Ellakany K, Nanda NC (2019) Diagnostic accuracy of dobutamine stress echocardiography in the detection of cardiac allograft vasculopathy in heart transplant recipients: A systematic review and meta-analysis study. Echocardiography 36(3):528–536
Hussein S, Dandel M, Hetzer R (2014) Exercise echocardiography with speckle-tracking derived strain and strain-rate analysis allows detection of heart transplant recipients with focal coronary stenoses. Circulation 130 (Suppl 2): A 18742
Eroglu E, D’Hooge J, Sutherland GR et al (2008) Quantitative dobutamine stress echocardiography for early detection of cardiac allograft vasculopathy in heart transplant recipients. Heart 94: 2 e3
Knuuti J, Wijns W, Saraste A et al (2020) 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J 41:407–477
Gilbert EM, Eiswirth CC, Mealey PC, Larrabee P, Herrick CM, Bristow MR (1989) Beta-adrenergic supersensitivity of the transplanted human heart is presynaptic in origin. Circulation 79:344–349
Shah NR, Blankstein R, Villines T, Imran H, Morrison AR, Cheezum MK (2018) Coronary CTA for Surveillance of Cardiac Allograft Vasculopathy. Curr Cardiovasc Imaging Rep 11:26
Romeo G, Houyel L, Angel CY, Brenot P, Riou JY, Paul JF (2005) Coronary stenosis detection by 16-slice computed tomography in heart transplant patients: comparison with conventional angiography and impact on clinical management. J Am Coll Cardiol 45:1826–1831
Schepis T, Achenbach S, Weyand M et al (2009) Comparison of dual source computed tomography versus intravascular ultrasound for evaluation of coronary arteries at least one year after cardiac transplantation. Am J Cardiol 104:1351–1356
Ballesteros Pradas SM, Romero Rodríguez N, Lage Gallé E et al (2010) Cardiac allograft vasculopathy: coronary computed tomography and virtual histology assessment. Transplant Proc 42:3175–3177
Wever-Pinzon O, Romero J, Kelesidis I et al (2014) Coronary computed tomography angiography for the detection of cardiac allograft vasculopathy: a meta-analysis of prospective trials. J Am Coll Cardiol 63:1992–2004
Günther A, Aaberge L, Abildgaard A et al (2018) Coronary computed tomography in heart transplant patients: detection of significant stenosis and cardiac allograft vasculopathy, image quality, and radiation dose. Acta Radiol 59:1066–1073
Mittal TK, Panicker MG, Mitchell AG, Banner NR (2013) Cardiac allograft vasculopathy after heart transplantation: electrocardiographically gated cardiac CT angiography for assessment. Radiology 268:374–381
von Ziegler F, Kaczmarek I, Knez A et al (2011) Coronary calcifications detected by computed tomography are not markers of cardiac allograft vasculopathy. Transplantation 92:493–498
Günther A, Andersen R, Gude E et al (2018) The predictive value of coronary artery calcium detected by computed tomography in a prospective study on cardiac allograft vasculopathy in heart transplant patients. Transpl Int 31:82–91
Khan R, Jang IK (2012) Evaluation of coronary allograft vasculopathy using multi-detector row computed tomography: a systematic review. Eur J Cardiothorac Surg 41:415–422
Rodney RA, Johnson LL, Blood DK, Barr ML (1994) Myocardial perfusion scintigraphy in heart transplant recipients with and without allograft atherosclerosis: a comparison of thallium-201 and technetium 99m sestamibi. J Heart Lung Transplant 13:173–180
Elhendy A, van Domburg RT, Vantrimpont P, Poldermans D, Bax JJ, van Gelder T, Baan CC, Schinkel A, Roelandt JR, Balk AH (2002) Prediction of mortality in heart transplant recipients by stress technetium-99m tetrofosmin myocardial perfusion imaging. Am J Cardiol 89:964–968
Wu YW, Yen RF, Lee CM et al (2005) Diagnostic and prognostic value of dobutamine thallium-201 single-photon emission computed tomography after heart transplantation. J Heart Lung Transplant 24:544–550
Ciliberto GR, Ruffini L, Mangiavacchi M et al (2001) Resting echocardiography and quantitative dipyridamole technetium-99m sestamibi tomography in the identification of cardiac allograft vasculopathy and the prediction of long-term prognosis after heart transplantation. Eur Heart J 22:964–971
Manrique A, Bernard M, Hitzel A et al (2010) Diagnostic and prognostic value of myocardial perfusion gated SPECT in orthotopic heart transplant recipients. J Nucl Cardiol 17:197–206
Hacker M, Tausig A, Romüller B et al (2005) Dobutamine myocardial scintigraphy for the prediction of cardiac events after heart transplantation. Nucl Med Commun 26:607–612
Veenis JF, Boiten HJ, van den Berge JC et al (2019) Prediction of long-term (> 10 year) cardiovascular outcomes in heart transplant recipients: Value of stress technetium-99m tetrofosmin myocardial perfusion imaging. J Nucl Cardiol 26:845–852
Wenning C, Vrachimis A, Dell Aquila A, Penning A, Stypmann J, Schäfers M (2015) Inhomogeneous myocardial stress perfusion in SPECT studies predicts future allograft dysfunction in heart transplant recipients. EJNMMI Res 5:51
Mc Ardle BA, Dowsley TF, deKemp RA, Wells GA, Beanlands RS (2012) Does rubidium-82 PET have superior accuracy to SPECT perfusion imaging for the diagnosis of obstructive coronary disease?: A systematic review and meta-analysis. J Am Coll Cardiol 60:1828–1837
Agostini D, Roule V, Nganoa C et al (2018) First validation of myocardial flow reserve assessed by dynamic 99mTc-sestamibi CZT-SPECT camera: head to head comparison with 15O-water PET and fractional flow reserve in patients with suspected coronary artery disease. The WATERDAY study. Eur J Nucl Med Mol Imaging 45:1079–1090
Chih S, McDonald M, Dipchand A et al (2020) Canadian Cardiovascular Society/Canadian Cardiac Transplant Network position statement on heart transplantation: Patient eligibility, selection, and post-transplantation care. Can J Cardiol 36:335–356
Allen-Auerbach M, Schöder H, Johnson J et al (1999) Relationship between coronary function by positron emission tomography and temporal changes in morphology by intravascular ultrasound (IVUS) in transplant recipients. J Heart Lung Transplant 18:211–219
Bravo PE, Bergmark BA, Vita T et al (2018) Diagnostic and prognostic value of myocardial blood flow quantification as non-invasive indicator of cardiac allograft vasculopathy. Eur Heart J 39:316–323
Pampaloni MH, Shrestha UM, Sciammarella M, Seo Y, Gullberg GT, Botvinick EH (2017) Noninvasive PET quantitative myocardial blood flow with regadenoson for assessing cardiac allograft vasculopathy in orthotopic heart transplantation patients. J Nucl Cardiol 24:1134–1144
Wu YW, Chen YH, Wang SS et al (2010) PET assessment of myocardial perfusion reserve inversely correlates with intravascular ultrasound findings in angiographically normal cardiac transplant recipients. J Nucl Med 51:906–912
Sasaki M, Tahara N, Abe T, Ueno T, Fukumoto Y (2016) FDG-PET reveals coronary artery inflammation proceeding to cardiac allograft vasculopathy progression. Eur Heart J 37:2413
Olymbios M, Kwiecinski J, Berman DS, Kobashigawa JA (2018) Imaging in Heart Transplant Patients. JACC Cardiovasc Imaging 11:1514–1530
Mc Ardle BA, Davies RA, Chen L et al (2014) Prognostic value of rubidium-82 positron emission tomography in patients after heart transplant. Circ Cardiovasc Imaging 7:930–937
Feher A, Srivastava A, Quail MA et al (2020) Serial Assessment of Coronary Flow Reserve by Rubidium-82 Positron Emission Tomography Predicts Mortality in Heart Transplant Recipients. JACC Cardiovasc Imaging 13:109–120
Fearon WF, Hirohata A, Nakamura M et al (2006) Discordant changes in epicardial and microvascular coronary physiology after cardiac transplantation: Physiologic Investigation for Transplant Arteriopathy II (PITA II) study. J Heart Lung Transplant 25:765–771
Nunoda S, Machida H, Sekikawa A et al (2010) Evaluation of cardiac allograft vasculopathy by multidetector computed tomography and whole-heart magnetic resonance coronary angiography. Circ J 74:946–953
Colvin-Adams M, Petros S, Raveendran G, Missov E, Medina E, Wilson R (2011) Qualitative Perfusion Cardiac Magnetic Resonance Imaging Lacks Sensitivity in Detecting Cardiac Allograft Vasculopathy. Cardiol Res 2:282–287
Erbel C, Mukhammadaminova N, Gleissner CA et al (2016) Myocardial Perfusion Reserve and Strain-Encoded CMR for Evaluation of Cardiac Allograft Microvasculopathy. JACC Cardiovasc Imaging 9:255–266
Machida H, Nunoda S, Okajima K et al (2012) Magnetic resonance assessment of left ventricular diastolic dysfunction for detecting cardiac allograft vasculopathy in recipients of heart transplants. Int J Cardiovasc Imaging 28:555–562
Chih S, Ross HJ, Alba AC, Fan CS, Manlhiot C, Crean AM (2016) Perfusion Cardiac Magnetic Resonance Imaging as a Rule-Out Test for Cardiac Allograft Vasculopathy. Am J Transplant 16:3007–3015
Narang A, Blair JE, Patel MB et al (2018) Myocardial perfusion reserve and global longitudinal strain as potential markers of coronary allograft vasculopathy in late-stage orthotopic heart transplantation. Int J Cardiovasc Imaging 34:1607–1617
Miller CA, Sarma J, Naish JH et al (2014) Multiparametric cardiovascular magnetic resonance assessment of cardiac allograft vasculopathy. J Am Coll Cardiol 63:799–808
Iannino N, Fischer K, Friedrich M, Hafyane T, Mongeon FP, White M (2020) Myocardial Vascular Function Assessed by Dynamic Oxygenation-sensitive Cardiac Magnetic Resonance Imaging Long-term Following Cardiac Transplantation. Transplantation. Epub ahead of print
Chaikriangkrai K, Abbasi MA, Sarnari R et al (2019) Natural history of myocardial late gadolinium enhancement predicts adverse clinical events in heart transplant recipients. J Am Coll Cardiol Img 12:2092–2094
Chaikriangkrai K, Abbasi MA, Sarnari R et al (2020) Prognostic Value of Myocardial Extracellular Volume Fraction and T2-mapping in Heart Transplant Patients. JACC Cardiovasc Imaging 13:1521–1530
Funding
Open access funding provided by Università degli Studi di Siena within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sciaccaluga, C., Ghionzoli, N., Mandoli, G. et al. The role of non-invasive imaging modalities in cardiac allograft vasculopathy: an updated focus on current evidences. Heart Fail Rev 27, 1235–1246 (2022). https://doi.org/10.1007/s10741-021-10155-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-021-10155-0