Abstract
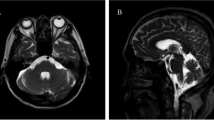
Rapidly progressive cerebellar ataxia is a classical paraneoplastic neurological syndrome associated with different autoantibodies and typical demographic characteristics, extracerebellar signs, tumor association, and prognosis. Anti-Tr/anti-Delta/Notch-like epidermal growth factor-related receptor (DNER) antibody is one of the associated antibodies. Given the rarity of this condition, our current knowledge is based on case reports and small case series. In order to improve our understanding of these conditions, we conducted a systematic review of the literature. Our study followed the PRISMA reporting guidelines. Studies of patients with the presence of anti-Tr/DNER antibodies in serum or cerebrospinal fluid (CSF) were included. We extract data information related to study characteristics, demographics, clinical symptoms, tumor association, neuroimaging, and cerebrospinal fluid analysis. Out of 131 records, we analyzed 17 papers, including a total of 85 patients with anti-Tr/DNER antibody–associated cerebellar ataxia. We confirmed that this disease occurred mostly in middle-aged males. Isolated cerebellar ataxia was the most common presentation. Extracerebellar features were rare (8%). Ninety-one percent of the patients presented an associated tumor, being Hodgkin lymphoma the most common. Abnormal neuroimaging patterns included cerebellar atrophy (19%) and cerebellar hypersignal (6%). Cerebrospinal fluid was inflammatory in 64% of the patients. Oncological response was complete in 88%, but neurological prognosis was poor with only 41% of the patients presenting significant neurological improvement at the last follow up. Anti-Tr/DNER antibodies should be tested in rapid progressive cerebellar ataxia. Oncological response is excellent; however, many patients do not improve from their cerebellar ataxia.



Similar content being viewed by others
References
Graus F, Vogrig A, Muñiz-Castrillo S, Antoine J-CG, Desestret V, Dubey D, et al. Updated diagnostic criteria for paraneoplastic neurologic syndromes. Neurol Neuroimmunol Neuroinflamm. 2021;8(4):e1014. Available from. https://doi.org/10.1212/NXI.0000000000001014.
Hadjivassiliou M, Graus F, Honnorat J, Jarius S, Titulaer M, Manto M, et al. Diagnostic criteria for primary autoimmune cerebellar ataxia-guidelines from an International Task Force on Immune-Mediated Cerebellar Ataxias. Cerebellum. 2020;19(4):605–10.
Jarius S, Wildemann B. “Medusa head ataxia”: the expanding spectrum of Purkinje cell antibodies in autoimmune cerebellar ataxia. Part 3: Anti-Yo/CDR2, anti-Nb/AP3B2, PCA-2, anti-Tr/DNER, other antibodies, diagnostic pitfalls, summary and outlook. J Neuroinflammation. 2015;12:168.
Trotter JL, Hendin BA, Osterland CK. Cerebellar degeneration with Hodgkin disease. An immunological study. Arch Neurol. 1976;33(9):660–1.
de Graaff E, Maat P, Hulsenboom E, van den Berg R, van den Bent M, Demmers J, et al. Identification of delta/notch-like epidermal growth factor-related receptor as the Tr antigen in paraneoplastic cerebellar degeneration. Ann Neurol. 2012;71(6):815–24.
Arya S, Kaji AH, Boermeester MA. PRISMA reporting guidelines for meta-analyses and systematic reviews. JAMA Surg. 2021; Available from. https://doi.org/10.1001/jamasurg.2021.0546.
Christensen PB, Gregersen H, Almasi C. Anti-Tr/DNER antibody paraneoplastic cerebellar degeneration preceding a very late relapse of Hodgkin Lymphoma after 12 years. Cerebellum Ataxias. 2021;8(1):14.
Taniguchi Y, Tanji C, Kawai T, Saito H, Marubayashi S, Yorioka N. A case report of plasmapheresis in paraneoplastic cerebellar ataxia associated with anti-Tr antibody. Ther Apher Dial. 2006;10(1):90–3.
Gungor S, Kilic B, Arslan M, Ozgen U, Dalmau J. Hodgkin’s lymphoma associated with paraneoplastic cerebellar degeneration in children: a case report and review of the literature. Childs Nerv Syst. 2017;33(3):509–12.
Suri V, Khan NI, Jadhao N, Gupta R. Paraneoplastic cerebellar degeneration in Hodgkin’s lymphoma. Ann Indian Acad Neurol. 2012l;15(3):205–7.
Shams’ili S, Grefkens J, de Leeuw B, van den Bent M, Hooijkaas H, van der Holt B, et al. Paraneoplastic cerebellar degeneration associated with antineuronal antibodies: analysis of 50 patients. Brain. 2003;126(Pt 6):1409–18.
Ypma PF, Wijermans PW, Koppen H, Sillevis Smitt PAE. Paraneoplastic cerebellar degeneration preceding the diagnosis of Hodgkin’s lymphoma. Neth J Med. 2006 Jul;64(7):243–7.
Bruylant K, Crols R, Humbel RL, Appel B, De Deyn PP. Probably anti-Tr associated paraneoplastic cerebellar degeneration as initial presentation of a squamous cell carcinoma of the lung. Clin Neurol Neurosurg. 2006;108(4):415–7.
Peltola J, Hietaharju A, Rantala I, Lehtinen T, Haapasalo H. A reversible neuronal antibody (anti-Tr) associated paraneoplastic cerebellar degeneration in Hodgkin’s disease. Acta Neurol Scand. 1998;98(5):360–3.
Greene M, Lai Y, Baella N, Dalmau J, Lancaster E. Antibodies to Delta/notch-like epidermal growth factor-related receptor in patients with anti-Tr, paraneoplastic cerebellar degeneration, and Hodgkin lymphoma. JAMA Neurol. 2014;71(8):1003–8.
Bernal F, Shams’ili S, Rojas I, Sanchez-Valle R, Saiz A, Dalmau J, et al. Anti-Tr antibodies as markers of paraneoplastic cerebellar degeneration and Hodgkin’s disease. Neurology. 2003;60(2):230–4.
Graus F, Dalmau J, Valldeoriola F, Ferrer I, Reñe R, Marin C, et al. Immunological characterization of a neuronal antibody (anti-Tr) associated with paraneoplastic cerebellar degeneration and Hodgkin’s disease. J Neuroimmunol. 1997;74(1–2):55–61.
Geromin A, Candoni A, Marcon G, Ferrari S, Sperotto A, De Luca S, et al. Paraneoplastic cerebellar degeneration associated with anti-neuronal anti-Tr antibodies in a patient with Hodgkin’s disease. Leuk Lymphoma. 2006;47(9):1960–3.
Schwenkenbecher P, Chacko L, Pul R, Sühs K-W, Wegner F, Wurster U, et al. Paraneoplastic cerebellar syndromes associated with antibodies against Purkinje cells. Int J Neurosci. 2018;128(8):721–8.
Briani C, Vitaliani R, Grisold W, Honnorat J, Graus F, Antoine JC, et al. Spectrum of paraneoplastic disease associated with lymphoma. Neurology. 2011;76(8):705–10.
Quero K, Joubert B, Picard G, Rogemont V, Touati M, Jaccard A, Magi L, Abraham J, Honnorat J. Paraneoplastic cerebellar degeneration associated with Hodgkin lymphoma: a French retrospective cohort. Poster presented at: 25th Congress of the European Hematology Association. June 11–21, 2020.
Barba C, Alexopoulos H, Dimitriadou M, Akrivou S, Tsiortou P, Plomaritoglou A, Dalakas MC. Anti- Trantibodies in autoimmune cerebellar ataxia: Serial antibody testing and response to immunotherapy (P2.2-039). Neurology. 2019; 92(15 Supplement). https://n.neurology.org/content/92/15_Supplement/P2.2-039.abstract.
Shenoy P, Maggioncalda A, Malik N, Flowers CR. Incidence patterns and outcomes for Hodgkin lymphoma patients in the United States. Adv Hematol. 2011;2011:725219.
Tohgo A, Eiraku M, Miyazaki T, Miura E, Kawaguchi S-Y, Nishi M, et al. Impaired cerebellar functions in mutant mice lacking DNER. Mol Cell Neurosci. 2006;31(2):326–33.
Engert A, Franklin J, Eich HT, Brillant C, Sehlen S, Cartoni C, et al. Two cycles of doxorubicin, bleomycin, vinblastine, and dacarbazine plus extended-field radiotherapy is superior to radiotherapy alone in early favorable Hodgkin’s lymphoma: final results of the GHSG HD7 trial. J Clin Oncol. 2007;25(23):3495–502.
Fermé C, Eghbali H, Meerwaldt JH, Rieux C, Bosq J, Berger F, et al. Chemotherapy plus involved-field radiation in early-stage Hodgkin’s disease. N Engl J Med. 2007;357(19):1916–27.
Gordon LI, Hong F, Fisher RI, Bartlett NL, Connors JM, Gascoyne RD, et al. Randomized phase III trial of ABVD versus Stanford V with or without radiation therapy in locally extensive and advanced-stage Hodgkin lymphoma: an intergroup study coordinated by the Eastern Cooperative Oncology Group (E2496). J Clin Oncol. 2013;31(6):684–91.
Zaborowski MP, Michalak S. Cell-mediated immune responses in paraneoplastic neurological syndromes. Clin Dev Immunol. 2013;2013:630602.
Eiraku M, Hirata Y, Takeshima H, Hirano T, Kengaku M. Delta/Notch-like epidermal growth factor (EGF)-related receptor, a novel EGF-like repeat-containing protein targeted to dendrites of developing and adult central nervous system neurons *. J Biol Chem. 2002;277(28):25400–7.
Rewcastle NB. Subacute cerebellar degeneration with Hodgkin’s disease. Arch Neurol. 1963;9:407–13.
Horwich L, Buxton PH, Ryan GM. Cerebellar degeneration with Hodgkin’s disease. J Neurol Neurosurg Psychiatry. 1966;29(1):45–51.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–6.
Author information
Authors and Affiliations
Contributions
Igor Gusmão Campana: substantial contributions to the conception or design of the work; acquisition of data for the work; and drafting of the work
Guilherme Diogo Silva: substantial contributions to the conception or design of the work; acquisition of data for the work; and major revision for important intellectual content
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(XLSX 19 kb)
Rights and permissions
About this article
Cite this article
Campana, I.G., Silva, G.D. Anti-Tr/DNER Antibody–Associated Cerebellar Ataxia: a Systematic Review. Cerebellum 21, 1085–1091 (2022). https://doi.org/10.1007/s12311-021-01346-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12311-021-01346-4