Abstract
Coronary revascularization for multivessel disease remains a common and costly source of hospitalizations in the United States. Surgical techniques influence outcomes for coronary bypass and also affect the need for percutaneous coronary intervention in the future. As more radial access has been used for coronary angiography, consideration for use of the radial artery as a surgical conduit remains unclear. Saphenous vein grafts are commonly used for coronary bypass, however long-term patency remains suboptimal, and is also associated with a higher risk of adverse events with percutaneous coronary intervention. Thus, understanding the interplay between coronary bypass techniques and percutaneous coronary intervention has become increasingly important.
Similar content being viewed by others
Coronary revascularization procedures via surgical revascularization are common and costly. |
Understanding surgical techniques for coronary artery bypass is important for long-term outcomes after bypass. |
Despite consideration for increased use of arterial grafts, saphenous vein grafts remain the most commonly used conduits in practice. |
The need for percutaneous intervention to bypass grafts is common and consideration for native vessel versus graft intervention is multi-faceted. |
Digital Features
This article is published with digital features, including a summary slide, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.13537010.
Introduction
Cardiovascular disease continues to be the leading cause of death in the United States and worldwide [1]. Coronary revascularization through either percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) remains one of the most frequently performed and costly procedures in the United States, with costs exceeding $6.7 billion annually in Medicare inpatient payments [2]. CABG remains the standard of revascularization for patients with multi-vessel disease, left main disease, and systolic dysfunction. Procedural volumes in the United States alone are around 200,000 CABG cases and 500,000 PCIs are performed annually [3, 4]. Given the frequency of both procedures, as well as the inherent interplay between coronary angiography, bypass surgery, and subsequent graft failure leading to need for PCI, a discussion of relevant factors from both an interventional cardiology as well as surgical perspective is warranted. The following review highlights overlapping topics relevant to both surgical revascularization and PCI including selection of graft conduits, subclavian stenosis, saphenous vein graft (SVG) patency, and use of anastomotic markers. Considerations for appropriate graft selection and factors affecting long-term outcomes are described in Fig. 1.
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Selection of Bypass Conduit
Choosing appropriate bypass conduits is important in consideration of long-term outcomes after surgical revascularization. There has been renewed interest in arterial revascularization including the use of bilateral internal thoracic arteries or radial arteries as conduits; however, these still comprise only a small subset of procedures [4.9% and 6.5% of secondary graft choice following the internal mammary artery (IMA)]. Graft selection is a complex decision that involves consideration of the affected vessels, degree of stenosis, surgeon preference and experience, and patient factors such as age, comorbidities, body habitus, tobacco use, and prior manipulation of potential grafts as access vessels during coronary angiography. Other considerations include size match between graft and target coronary to be bypassed, conduit length, and luminal diameter [5].
Internal Mammary Arteries
The use of the left internal mammary artery (LIMA) to graft the left anterior descending (LAD) territory has become standard practice. Both the right and left IMAs are significantly more resistant to the development of atherosclerosis compared to SVGs for several reasons, including the presence of a non-fenestrated endothelial layer, lower intercellular junction permeability, higher concentration of antithrombotic molecules, and endogenous endothelial nitric oxide production [6]. Multiple large long-term follow-up studies have demonstrated decreased CABG mortality that corresponds to increased LIMA utilization, with highest IMA graft patency seen when used to graft the left coronary system [7–9].
The long-term patency and significant survival benefit of LIMA usage in CABG has prompted substantial interest in the use of additional arterial conduits, or multi-arterial grafting (MAG) in CABG. The most commonly used conduits for a second arterial graft are the radial artery and the right internal mammary artery (RIMA). While the role of a single IMA as the first and most important graft in CABG has been established, there is ongoing controversy regarding the true value of the use of bilateral IMAs (BIMA) due to uncertainty of the incremental additional survival benefit of a second IMA graft and concerns about the increased risk of sternal wound complications and mediastinitis associated with BIMA harvesting [9]. Currently there is ~ 4% BIMA usage in CABG in the United States and ~ 12% in Europe [10]. The use of a skeletonized (vs. pedicled) harvest technique for RIMA harvest has been proposed as a means to decrease deep sternal wound infections, but concerns about the effect on graft patency have limited adoption of this technique as well [10].
Meta-analysis of 29 retrospective studies including 89,399 patients by Buttar et al. in [10] demonstrated a substantial benefit to overall survival with the use of BIMA compared to LIMA alone along with improved cardiac-event-free, infarct-free, and angina-free survival with BIMA use with effect sizes that continued to increase at extended (> 5 year) follow-up [10]. The Arterial Revascularization Trial (ART) was the first major prospective RCT examining the effect of BIMA vs. SIMA use on long-term outcomes [11]. The 10-year follow-up results of ART were reported by Taggart et al. [12]. The primary endpoint of all-cause mortality did not demonstrate a significant difference in survival between patients undergoing BIMA vs. SIMA grafting, which is inconsistent with prior retrospective data on the subject. In subgroup analysis, there was a survival benefit to the use of MAG (BIMA or SIMA + radial graft). It is anticipated that benefit of MAG will be more completely addressed by the prospective multicenter Randomized comparison of clinical Outcome of single vs. Multiple Arterial grafts (ROMA) trial examining mid- and long-term outcomes of the use of single vs. multiple arterial grafting in CABG. Enrollment in this trial began in January 2018 with an intended cohort of 4300 patients [13]. In our institution, MAG has been reserved for patients under the age of 70 years. The most common conduit selection is in situ LIMA pedicle, skeletonized RIMA as an in situ pedicle or free graft and the non-dominant radial artery. The LIMA is placed on the LAD, RIMA to the distal RCA, posterior descending artery or an obtuse marginal branch (with ≥ 70% stenosis) and radial artery as a free sequential bypass graft usually to an obtuse marginal branch, a diagonal or ramus intermedius (with ≥ 70% stenosis). Target vessels with high-grade stenosis and minimal competitive flow are chosen to increase the likely that an arterial bypass conduit will mature.
Radial Artery
SVGs are widely used, despite occlusion rates as high as 25% at 1 year and 75% at 10 years [14]. The radial artery is an attractive vessel for use in coronary bypass surgery as its length allows it to be used for almost any coronary target or even for multiple sequential anastomoses [15]. The diameter of the radial artery is comparable to most coronary arteries, and observational data show similar 10-year patency rates to that of IMA grafts [16]. With an increase in use, there was concern that poor patency rates at follow-up angiography were secondary to spasm and intimal hyperplasia, but refined harvesting techniques and pharmacologic protocols have demonstrated that rates of radial artery patency have improved over time [16, 17]. At 10-year follow-up, radial artery grafts showed patency of 91.6% and perfect patency (no luminal irregularities) of 88% compared with 97.5% and 96.3% for IMA grafts in a recent study by Gianfederico et al. [18]. This is in contrast with SVG patency rates in the same group of 67.1% and 53.4%. However, radial artery conduits are susceptible to spasm when grafted to native vessels with lesser degrees of stenosis. When grafted to coronary arteries with non-occlusive disease, this conduit is more likely to be found occluded or have radial artery graft stenosis in follow-up angiography [18, 19].
Transradial Catheterization and Subsequent Radial Graft Patency
Recently there has been a shift in the overall utilization of radial access due to multiple factors. Radial access for coronary angiography has been associated with decreased bleeding complications as well as a reduction in mortality in patients with acute coronary syndromes [20, 21]. Given shifting preference for radial artery access as primary access site, there is concern that the use of the radial artery for access during coronary procedures may impact use as a bypass conduit. Histological evaluation of the distal section of radial arteries harvested for use following transradial (TRA) catheterization, compared to those without, showed significant increase in intimal hyperplasia, observed in 68% of specimens that had prior TRA catheterization and in 39% of patients not having TRA. In this study, patients underwent follow-up angiography at 1 month following bypass, and patients with prior TRA catheterization had radial artery graft patency of 77% compared with 98% in those that did not have prior TRA catheterization [22].
In addition to intimal hyperplasia, in a series utilizing optical coherence tomography, imaging of the radial artery immediately following transradial catheterization revealed intimal tears in 67% of patients and medial dissections in 35.6%. Although more frequent in the distal end of the vessel, damage was also observed in the proximal vessel. Furthermore, patients with repeat transradial procedures showed higher rates of radial artery damage than with first-time procedures [23]. Transradial catheterization also appeared to have adverse effects on radial artery size [23]. Although there is variation in the observed severity of decreased luminal diameter, overall persistence in diameter reduction appears to be related to changes in the structure of the artery rather than simply vasospasm [24].
Vasomotor function also appears to be adversely affected by transradial catheterizations. Multiple studies indicate that both flow-mediated dilation and nitroglycerin-mediated dilation are significantly impaired immediately following transradial catheterization. The duration of impaired vasomotor function is less clear, with some studies indicating partial recovery at 3–12 months, but additional reports show that full recovery fails to occur [25]. These concerns have led to hesitancy in using radial arteries that have been previously used for cardiac catheterization. Although typically the left radial artery is preferred for harvest for bypass while the right radial artery is used for cardiac catheterization, use of the left radial artery is not uncommon. Thus, further work is needed to determine the true clinical impact of radial artery instrumentation on bypass outcomes. The use of multi-arterial bypass grafts is reserved for younger CABG patients because of the perceived long-term benefits associate with improved patency rates and durability. It has been our practice to avoid the previously instrumented radial artery as a bypass conduit as the long-term patency of these vessels is uncertain.
On-pump vs. Off-pump Coronary Artery Bypass Grafting
The role of cardiopulmonary bypass (CPB) in the performance of CABG has been examined in detail. The distal anastomoses of coronary bypass grafts are most commonly performed with the use of the CPB to create a bloodless, motionless field (“on-pump”, ONCAB) but this can also be performed on a beating heart without CPB using specialized stabilizing devices and other techniques (“off-pump”, OPCAB). It was initially believed that patients who were older and with greater burden of comorbidities would benefit from an off-pump approach by sparing them exposure to the deleterious effects of aortic clamping and other manipulation and the systemic inflammatory response induced by CPB, which can include renal dysfunction, stroke, coagulopathy, and myocardial injury [26]. However, concerns existed about the effects of the off-pump technique on the completeness of revascularization and long-term graft patency [27]. Numerous high-profile RCTs have been conducted to address the role of off-pump CABG.
The Randomized On/Off Bypass (ROOBY) trial was a prospective randomized controlled trial conducted by the Veterans Administration comparing a composite endpoint of death and major complications at 30 days and 1 year in patients undergoing ONCAB (n = 1099) vs. OPCAB (n = 1104) CABG [27]. Study surgeons were required to document prior experience of at least 20 OPCAB procedures. Trainees served as the “primary” surgeon in 64% of the ONCAB cases vs. 55.4% of the OPCAB cases (p < 0.001). There was no difference in the combined endpoint at 30 days between the OPCAB and ONCAB groups, but the rate of the primary endpoint was greater in the off-pump cohort at 1 year (9.9 vs. 7.4%, p = 0.04). These patients also had slightly higher rates of death from cardiac causes at 1 year compared to on-pump patients (2.7 vs. 1.3%, p = 0.03). Significantly fewer grafts were performed in the OPCAB group compared to ONCAB (2.9 ± 0.9 vs. 3.0 ± 1.0, p = 0.002). At 5 years, the trends in higher rates of death (15.2 vs. 11.9%, p = 0.02) and the composite endpoint (31.0 vs. 27.1%, p = 0.046) in the OPCAB cohort continued. OPCAB patients also required repeat CABG at slightly higher rates (1.4 vs. 0.5%, p = 0.02) [28].
Follow-up angiograms performed 1 year after CABG demonstrated lower overall graft patency in the OPCAB group (82.6 vs. 87.8%, p < 0.01) and more patients with at least one occluded graft (36.5 vs. 28.7%, p < 0.01) [27]. LIMA-LAD graft patency was similar between groups though fewer LIMA-LAD grafts in the OPCAB group (89.0 vs. 93.2%, p = 0.01) were considered “excellent” by the FitzGibbon grading system.
The CABG Off or On Pump Revascularization Study (CORONARY) was an international prospective randomized controlled trial comparing a composite endpoint of death, nonfatal stroke, nonfatal myocardial infarction, and new renal failure requiring dialysis at 30 days after surgery in patients undergoing isolated OPCAB (n = 2375) vs. ONCAB (n = 2377) [29]. Participating surgeons were required to have at least 2 years of experience and have completed at least 100 procedures using the technique dictated by randomization; trainees were not allowed to serve as the primary surgeon for any procedure in this trial. There was no significant difference in the rate of the primary outcome between OPCAB vs. ONCAB (9.8 vs. 10.3%) at 30 days after surgery. Patients undergoing OPCAB received fewer grafts than in the ONCAB group (3.0 vs. 3.2, p < 0.001), were more likely to receive an incomplete revascularization (11.8 vs. 10.0%, p = 0.05), and were more likely to require repeat revascularization prior to discharge (0.7 vs. 0.2%, p = 0.01). Similar findings persisted at 1 and 5 years [30, 31].
The German Off-Pump Coronary Artery Bypass Grafting in Elderly Patients (GOPCABE) study was similar in design and analytic endpoints to CORONARY conducted on patients aged 75 years or older [32]. Study surgeons were required to be experienced in the technique dictated by randomization; OPCAB surgeons had performed a mean of 514 procedures and ONCAB surgeons had performed a mean of 1378 prior to the study. Similar to CORONARY, there was no significant difference in the primary composite endpoint between OPCAB and ONCAB at 30 days (7.8 vs. 8.2%) and 1 year (13.1 vs. 14.0%). OPCAB was associated with a lower number of grafts planned (2.9 vs. 3.0) and grafts performed (2.7 vs. 2.8, p < 0.001) and greater rates of incomplete revascularization (34.0 vs. 29.3%, p < 0.001) along with greater rates of early repeat revascularization (1.3 vs. 0.4%, p = 0.04). These findings persisted at 5-year follow-up [33].
When observed in aggregate, these trials demonstrate that OPCAB can be performed with short- and mid-term outcomes similar to that of ONCAB, but with important caveats. Patients undergoing OPCAB are likely to receive fewer bypass grafts and are more likely to receive an incomplete revascularization, which plays an important role in long-term survival. The level of surgeon and team experience with OPCAB also plays a crucial role in OPCAB outcomes. OPCAB outcomes in ROOBY, in which OPCAB surgeon experience requirements were relatively less stringent, were notably less favorable than in CORONARY and GOPCABE, in which OPCAB was performed only by surgeons with extensive experience with the technique.
A 2018 retrospective analysis of data from the National Inpatient Sample of over 2 million patients undergoing ONCAP or OPCAB between 2003 and 2011 by Benedetto et al. found that OPCAB was associated with increased risk-adjusted mortality, length of stay, and overall cost compared to ONCAP when performed by low-volume centers or low-volume surgeons. When performed by high-volume centers and high-volume surgeons, OPCAB was associated with reduced risk-adjusted mortality compared to ONCAB [34].
The effect of OPCAB experience on outcomes is further underscored by a large 2018 meta-analysis of all extant RCTs of OPCAB vs. ONCAB (104 trials including 20,627 patients) by Gaudino et al. found that OPCAB was associated with higher incidence of incomplete revascularization and decreased “midterm” (~ 3 year) survival compared to ONCAB [35].
In an editorial accompanying the publication of the 5-year results of GOPCABE, Puskas et al. argue that the evidence clearly demonstrates the importance of surgeon experience in OPCAB outcomes [36]. Although associated with inferior long-term survival and greater rates of incomplete revascularization in large cohorts, based on the available literature, OPCAB is a suitable option with near and midterm outcomes approximating those of ONCAB when performed by experienced teams at high-volume centers. In this setting, patients at greatest perioperative risk may derive the greatest benefit from OPCAB compared to the general CABG population.
Endoscopic vs. Open Saphenous Vein Harvest
Reversed greater SVG is the conduit most commonly used in CABG for revascularization of non-LAD territories [37]. SVG may be harvested using an open technique (open vein harvest, OVH), in which the desired length of vein is obtained using a single incision or multiple smaller “skip” incisions beginning just above the medial malleolus and extending proximally, or by endoscopic methods. Endoscopic vein harvest (EVH) is performed using dedicated platforms that allow SVG harvest via a single transverse 2–3 cm incision just above or below the medial aspect of the knee using a combination of endoscopic visualization, blunt dissection, and bipolar tissue sealing for control of side branches. Endoscopic dissection is extended proximally and distally based on the length of vein desired, after which additional sub-centimeter counterincisions are made to obtain proximal and distal control of the segments of SVG left in situ prior to removal of the conduit [37].
OVH has been the mainstay of vein harvest since the development of CABG and remains the most common method worldwide, but EVH has become commonplace in the US and other developed countries since its introduction in the mid-1990s [38]. Compared with OVH, EVH is associated with decreased pain and surgical site infection at the vein harvest site and decreased postoperative length of stay [39–41].
Concerns have been raised about the effect of EVH on long-term patency of vein grafts, due in part to endothelial injury resulting from the increased manipulation of the vein and use of bipolar tissue sealing in EVH [42]. A 2009 secondary analysis of patients undergoing CABG as a part of the Project of Ex-Vivo Vein Graft Engineering via Transfection IV (PREVENT IV) trial (n = 1753 EVH, n = 1247 OVH), which included angiographic follow-up at 12–18 months after CABG, by Lopes et al., reported higher rates of vein graft failure (defined by ≥ 75% stenosis) in patients undergoing EVH (46.7 vs. 38%, p < 0.001), along with higher rates of myocardial infarction (MI), repeat revascularization, and death at 3-year follow-up [43]. A 2018 systematic review and meta-analysis by Kodia et al. of 11 studies (including Lopes et al.) describing 18,131 patients undergoing CABG with OVH (60%) or EVH (40%) with a mean follow-up of 2.6 years reported superior graft patency in the OVH cohort (82.3 vs. 75.1%, p = 0.01) [42, 43].
Following the report by Lopes et al., a large-scale analysis of Society of Thoracic Surgeons (STS) Adult Cardiac Surgery Database, combined with Medicare data, was performed at the request of the US Food and Drug Administration by Williams et al. to evaluate the effect of EVH on death, MI, and repeat revascularization after CABG [41]. This observational study of 235,394 Medicare patients undergoing isolated CABG from 2003–2008 with one IMA and at least one vein graft reported that patients undergoing CABG + EVH had no significant difference in rates of death, MI, or repeat revascularization compared to patients undergoing CABG + OVH at 3 years of follow-up.
The similarity in non-wound outcomes between EVH and OVH have been re-demonstrated in more recent prospective randomized studies [38, 44]. Krishnamoorty et al. performed a single-center randomized controlled [Vein Integrity and Clinical Outcomes (VICO)] trial comparing two different EVH techniques and OVH (n = 100 in each) in patients undergoing CABG with one IMA and at least one vein graft, and reported mildly improved endothelial integrity in OVH conduits vs. both EVH techniques but without any difference in major adverse cardiac events seen at 48 months of follow-up [44]. Zenati et al. performed a randomized controlled [Randomized Endovein Graft Prospective (REGROUP)] trial of patients undergoing isolated CABG with at least one vein graft at 16 VA cardiac surgery centers from 2014–2017 (n = 1150 patients) examining the effect of EVH vs. OVH on a composite outcome of all-cause mortality, nonfatal MI, and repeat revascularization. Consistent with prior studies, there was an increased rate of wound complications in the OVH group but no difference between OVH and EVH with regard to other outcomes [38]. Angiographic follow-up was not reported in either of these studies.
Despite a growing body of evidence demonstrating equivalent long-term cardiac outcomes between EVH and OVH and lower rates of wound complications with EVH, the question of which technique is superior remains controversial. EVH was endorsed as the standard of care for vein harvest for CABG by the International Society for Minimally Invasive Cardiothoracic Surgery in a 2005 consensus statement and affirmed this position in a 2015 update [45]. While the superiority of EVH for mitigation of wound complications appears to be settled, questions about the effect of EVH on long-term vein graft patency remain. The use of a “no-touch” technique in OVH, in which the SVG is harvested as a single pedicle in which the surrounding vaso vasora and perivascular fatty and adventitial tissue are preserved, is associated with excellent long-term patency, likely attributable to the relative decrease in endothelial injury incurred during vein harvest [46–48]. A definitive answer to the question of the ideal vein harvest technique for CABG will likely require a large trial comparing EVH to no-touch OVH performed by experienced personnel. It has been our practice to harvest the SVG almost exclusively by EVH for greater than 10 years. The physician’s assistants in our practice are trained and proctored by industry specialists in EVH. Newer technology for EVH allows the practitioner to harvest the vein with minimal manipulation of the conduit and with focal bipolar cautery, thereby minimizing the thermal spread of injury.
Single vs. Multiple Distal Revascularization with SVGS
SVGs may be deployed using individual vein segments for each desired distal coronary bypass target with a unique proximal aortic anastomosis (single SVG, s-SVG) or with a longer vein segment serving multiple distal coronary targets from a single proximal aortic anastomosis (multiple SVG, m-SVG). In CABG procedures in which vein grafts are required for two or more distal coronary targets, the s-SVG technique results in the use of a corresponding number of distinct vein segments, whereas when the m-SVG technique (also referred to as “jump”, “snake”, or “sequential” grafts) is used, most or all distal targets may be served by a single vein graft [49]. Such grafts are typically deployed in a “right to left” configuration: the most distal end of the graft is anastomosed to the posterior descending artery of the right coronary system in an end-to-side fashion and then brought around the lateral wall of the left ventricle to bypass obtuse marginal and diagonal targets in via side-to-side coronary anastomoses, followed by standard proximal aortic anastomosis. Alternative configurations are common [49]. The use of s-SVG for the left anterior descending territory, however, is not recommended because of the overwhelming evidence supporting the use of the left internal mammary artery for this purpose [50].
At present, there is little high-quality evidence regarding the superiority of m-SVG vs. s-SVG. Proponents of s-SVG suggest that m-SVG makes a large section of myocardium with diseased native inflow dependent on the long-term patency of the proximal portion of a single vein graft. However, m-SVG grafts have been demonstrated to have higher flow rates than s-SVG grafts and that the flow rate in m-SVG grafts increases based on the number of distal anastomoses served by a single vein graft [51]. The use of m-SVG grafts may also make it possible to bypass smaller targets and creates the potential for coronary-to-coronary collateral flow in the event of proximal m-SVG graft occlusion [49].
Multiple studies have reported superior mid- and long-term patency of m-SVG grafts. Kim et al. performed a prospective cohort study of 309 patients undergoing isolated CABG at a single center from 2002–2007 in which intraoperative transit-time flow measurements and CT angiography prior to discharge and at 1 and 3–5 years postop were used to compare patency of s-SVG (n = 244) with m-SVG (n = 84) grafts [52]. m-SVG grafts demonstrated higher flow rates intraoperatively compared with s-SVG grafts, and flow increased linearly with the number of distal targets fed by a m-SVG graft. Greater patency at 3 years (93 vs. 87%, p = 0.048) was demonstrated in the m-SVG group. All-cause mortality and rates of MI and repeat revascularization were not reported.
Similar findings were reported by Park et al. in a prospective cohort study of 2515 patients undergoing isolated CABG (n = 1037 m-SVG and n = 1478 s-SVG) from the same center from 2005–2016 [50]. Five-year failure rates for m-SVG grafts were 10.3% compared with 17.7% for s-SVG group. There was also no significant difference in a composite endpoint of all-cause mortality, nonfatal MI, and repeat revascularization at mean follow-up of 88 months between m-SVG and s-SVG. A subgroup analysis compared the patency of m-SVG grafts bypassing the right coronary artery (RCA) system as a terminal end-to-side anastomosis and left circumflex (LCx) system as an in-transit side-to-side anastomosis with that of s-SVG grafts to each of these territories. Compared to the RCA-LCx m-SVG grafts, single grafts to the LCx territory had equivalent patency rates, whereas single grafts to the RCA system had lower patency rates. This comparison was further subdivided by single grafts to the distal RCA and to the posterior descending artery or posterolateral branch (PDA/PL); grafts to the distal RCA had equivalent patency to the m-SVG RCA-LCx grafts, whereas PDA/PL grafts had comparatively lower patency. A systematic review by Li et al., which included the report by Kim et al., also reported superior mid- and long-term patency of m-SVG grafts and specifically concluded that side-to-side anastomoses used for in-transit bypasses had superior long-term patency compared with end-to-side anastomoses [53].
A notable exception to the finding of superior long-term patency of m-SVG grafts is the report by Mehta et al. of the 1-year angiographic and 5-year clinical outcomes of patients undergoing m-SVG and s-SVG as a part of the PREVENT IV study [54]. As a part of the 12–18-month angiographic follow-up described in the preceding section, rates of SVG failure (defined as ≥ 75% stenosis) were highest in the m-SVG alone group (50.6%) and lowest in the s-SVG alone group (41.6%), and intermediate in patients who received a combination of m-SVG and s-SVG (46.0%). Rates of composite outcome of death, MI, and repeat revascularization at 5 years were modestly higher in patients undergoing m-SVG.
A more recent report by Wallgren et al. compared the effects of a single m-SVG serving the left and right coronary systems to s-SVG of these territories in 6.895 patients (m-SVG n = 2122, s-SVG n = 4773) undergoing CABG from 2009–2015 from the SWEDEHEART population-based registry, with a primary outcome of a composite endpoint of all-cause mortality, MI, re-angiography, and repeat revascularization at 30 days after surgery and a mean of 35 months of follow-up. A significantly higher rate of this endpoint at 30 days was observed in the m-SVG cohort (5.4 vs. 3.9%), along with higher rates of re-angiography (2.7 vs. 1.7%) and mortality (2.2 vs. 1.3%). However, these differences disappeared at mid-term follow-up. The authors attribute the disparate early results to the more technically demanding nature of m-SVG, although data about duration of cardiopulmonary bypass or aortic cross-clamp application are not reported [49].
Overall, there is not a clear consensus regarding the superiority of m-SVG compared to s-SVG for CABG. Current US and European CABG guidelines do not discuss the use of m-SVG vs. s-SVG [55, 56]. At this time, decisions about the use of multiple vs. single grafting should be individualized to patients based on factors including distribution of coronary lesions and availability of vein conduit in combination with surgeon preference and experience. We utilize m-SVG very commonly when there are four or more distal anastomoses to be completed. Some of the compelling considerations in choosing to create a m-SVG is the area of ascending aorta available for proximal anastomosis, the over length of conduit available to complete the CABG operation as well the caliber and quality of the distal target. Those targets with marginal run-off if bypassed with a s-SVG are more likely to fail. The m-SVG in these cases increases the outflow from the conduit, improves the flow rate, and should improve patency.
Subclavian Artery Stenosis
CABG procedures rely most commonly on grafting the left IMA (LIMA) for revascularization of the left anterior descending artery (LAD). While the IMA is known to have the highest patency rate and long-term survival of any bypass graft [57], its efficacy ultimately relies on patent proximal flow. Conditions such as subclavian artery stenosis (SAS) may lead to diminished proximal left subclavian artery perfusion and thus diminished flow to both the LAD via the IMA graft and the vessels of the left upper extremity. In a phenomenon referred to as coronary-subclavian steal syndrome, increased oxygen demand created by left upper extremity movement “steals” blood flow from the IMA graft to the arteries of the left upper extremity. The resultant reduction in flow to the LAD can present clinically as angina.
There is debate regarding the optimal screening method for determining the presence of SAS in patients prior to undergoing CABG. The strongest identifiable risk factor for SAS is a prior history of peripheral arterial disease. Those with a history of peripheral arterial disease have a SAS prevalence of 11.5%, compared with 7.6% in patients with cerebrovascular disease, 6.8% in patients with diabetes mellitus, and 4.3% in smokers and patients with hypertension [58]. The prevalence of SAS in patients without any such prior medical history has been reported at 1.5% [58]. The main methods of screening for SAS prior to undergoing CABG include both invasive and noninvasive techniques. Noninvasive techniques include upper extremity blood pressure differentials, doppler ultrasound, and CT angiography (CTA) or MRI angiography (MRA). Associated with minimal risk, some limitations exist in these methods. Inter-arm systolic blood pressure differences greater than 20 mmHg have been shown to have a modest positive predictive value of 67%, with a negative predictive value of nearly 100% [59]. To confirm the diagnosis of SAS in a patient with abnormal interarm systolic blood pressures, Doppler ultrasound can be performed. While readily available and inexpensive, Doppler ultrasonography can have limited efficacy due to overlying bony structures and may require severe stenoses and “stealing” for test results to be positive [60]. CTA and MRA can both provide suitable resolution of the brachiocephalic vessels and are at present understudied methods of assessing SAS presence and severity.
Subclavian angiography is the gold standard invasive screening modality for detecting SAS. In many cases, it can be performed with low risk at the time of coronary angiography. The most commonly associated adverse events include transient ischemic attacks and left upper extremity embolism, but the overall incidence during angiography is less than 2% [59]. Subclavian angiography not only provides definitive data on the patency of the proximal left subclavian artery, but can also be used to evaluate native disease in the LIMA itself as well as to ensure adequate caliber of the vessel for grafting. Significant findings including vertebral and subclavian artery stenoses were present in 15% of patients evaluated with subclavian angiography prior to undergoing CABG in a study by Feit et al. [61]. Further evidence for routine subclavian angiography prior to CABG comes from the radiology literature. In a rare presentation referred to as the Winslow pathway, infrarenal aortic occlusion leads to collateral circulation such that the IMAs provide the sole arterial supply to the lower extremities. If unrecognized at the time of CABG, lower extremity ischemia will result from redirected IMA flow [62]. The high sensitivity and specificity of brachiocephalic angiography are coupled with its success in the revascularization of stenotic subclavian vessels. In the largest single-operator report to date, Bates et al. evaluated preoperative subclavian stenting in 94 patients. Amongst these, there were no instances of subacute thrombosis or re-occlusion (within 30 days). The mid-term (30 days to 2 years) and long-term (> 2 years) restenosis rates were 5.7 and 10.7%, respectively [63]. Although the rates of restenosis of the subclavian artery are significant, given the very low risk of thrombosis or occlusion, stenting of the vessel in the preoperative setting is felt to be an excellent option [59].
There is no consensus on the optimal screening method for SAS prior to CABG. Some practitioners recommend relying on noninvasive screening methods to stratify which patients should undergo angiography [64, 65]. They recommend angiography only in those with inter-arm blood pressure differential greater than 10 mmHg, or if there is a history of radiation therapy to the chest, vasculitis, or known peripheral artery disease. The counterargument for more universal subclavian angiography is the relatively low complication rate as well as the ability to preoperatively intervene on stenoses. This is supported by a study by Marshall et al. noting that the absence of upper extremity claudication, differences in interarm blood pressure, and a history of cerebrovascular ischemia do not exclude the presence of SAS [66]. Subclavian angiography is the most sensitive and specific method for assessing the brachiocephalic vessels for stenotic lesions proximal to the origin of the IMA graft and may be considered in patients undergoing coronary angiography with anticipated need for CABG. In our clinical practice, subclavian angiography at the time of coronary angiography is not universally performed. Longer procedure times, contrast use, as well as more difficult engagement of the left subclavian artery from a right radial approach considerations for left subclavian angiography.
SVG Patency
Although the LIMA is the most common choice for bypass of the left anterior descending artery (LAD), selection of secondary bypass grafts is of some debate with vein grafts frequently being utilized. There is no standard definition of early SVG failure, but it is generally recognized as the presence of angiographically critical or occlusive disease within 1–2 years after CABG [67]. Unfortunately, approximately 15% of SVGs fail within the first year, usually resulting in PCI [67].
A retrospective analysis by Caños et al. examined their institutional database and found that grafts prone to early failure were relatively small, less likely to show ectasia or luminal irregularity comprising of ≥ 50% of SVG shaft length, located in the ostial or proximal third of the graft, and had an increased frequency of TIMI flow grade 0/1 [68]. Intravascular ultrasound analysis in this study showed that early SVGs that fail had lesions that represent an aggressive and diffuse disease process throughout the graft [68]. Patency of vein grafts diminish from 98% immediately after surgery to < 88% within the first month post-operatively with risk factors for failure including diabetes mellitus, hyperlipidemia, and chronic kidney disease [69–72].
Early vein graft failure (VGF) usually occurs within 1 month post CABG and is most commonly due to acute thrombosis of the graft. This is related to technical factors such as the size of the target vessel resulting in poor distal runoff, size mismatch between the graft and target vessel creating turbulent flow, and disruption of the endothelial layer as a result of mechanical trauma and manual distention [73]. Other factors resulting in graft failure within 1 month include a small diameter of the vein graft, pre-existing vein graft disease, and hypercoagulability [74]. When considering vein graft failure between 1 month and 1 year, intimal hyperplasia is the most common etiology. This is thought to be caused by the vein graft’s adaptation to higher arterial pressures, loss of inhibition from the endothelial layer, and smooth muscle cells proliferating and migrating into the vessel’s intimal layer. After 1 year, atherosclerosis becomes the primary reason for vein graft stenosis and occlusion. Similarly to native coronary vessels, vein graft atheromas can rupture, causing thrombotic occlusion of the graft [75]. Vein graft atheromas are noted to be more diffuse, concentric, less calcific, have poorly developed or even absent fibrous caps, and be more susceptible to thrombosis and rupture [76, 77]. Also, human autopsy studies have shown that coronary vein grafts undergo more rapid atherosclerotic lesion development than native arteries [76].
A retrospective study by Halabi et al. showed that early SVG disease was associated with an increased risk of long-term adverse clinical outcomes. In this study, among the patients who underwent cardiac catheterization 1 to 18 months after CABG, the composite of death, MI, and repeat revascularization was significantly more likely among patients with critical (75–99% stenosis) or occlusive (100% stenosis) SVG disease than in those with noncritical (25–75% stenosis) or no stenosis (< 25%) [67]. Additionally, in multivariate analysis, critical (75–99% stenosis) or occlusive (100% stenosis) SVG disease was the strongest predictor of the composite outcome (hazard ratio 2.36, 95% confidence interval 2.00 to 2.79, p < 0.0001) [67].
A prospective cohort study on long-term patency of SVG and LIMA grafts after CABG published by Goldman et al. showed that 10-year patency for SVGs was 61% compared with 85% for LIMA grafts. Along with location of the distal site, the best predictor of graft patency over the 10-year post-bypass period was the diameter of the recipient vessel by angiographic measurement [78]. The 10-year patency rate was 88% for vessels > 2.0 mm in diameter compared with 55% for vessels < 2.0 mm in diameter [78].
Immediately after harvesting, venous conduits undergo a period of ischemia and reperfusion after engraftment resulting in endothelial cell and smooth muscle cell (SMC) damage [79]. The temporary closure of the lumen and reperfusion in these grafts causes damage to the vessel wall, while engraftment in the arterial circulation increases flow as well as longitudinal and circumferential shear stress. This additional stress results in additional damage to SMCs and the extracellular matrix (ECM) as well as generation of reactive oxygen species [79, 80]. Platelets and fibrin are deposited, and circulating leukocytes attach and infiltrate the vessel wall. Growth factors are subsequently released from platelets, macrophages, and SMCs, leading to increased proliferation and migration of SMCs to the intima [81]. Uncontrolled SMC proliferation, extensive ECM deposition, and the influx of macrophages all contribute to intimal hyperplasia [81].
In 1964, Szilagyi and colleagues first suggested that a vein needs to undergo a ≥ 50% increase in dimension to adapt to the increased pressure in the arterial circulation. Although this initial adaptation is necessary for veins to acquire an artery-like structure, this process can also lead to vein graft failure [82]. Arterialization of venous bypass grafts involves processes such as intimal hyperplasia, geometric remodeling, wall stiffening, and inflammation [80].
Perioperative MI with irreversible myocardial cell damage is one of the most serious and life-threatening complications after CABG, and is associated with substantially increased in-hospital morbidity and mortality rates [83]. The most common graft-related etiologies of myocardial cell damage after CABG are graft occlusion due to acute graft thrombosis, subtotal or hemodynamically relevant anastomotic stenosis, graft kinking or overstretching, and postoperative graft spasm [84, 85]. The early identification of patients with perioperative MI due to acute graft failure enables an adequate reintervention strategy for re-revascularization, such as PCI or surgical graft revision to salvage reversibly damaged myocardium. The incidence of early graft failure within 24 h after CABG is about 1–3%, which is strongly associated with a higher mortality within 30 days and a higher incidence of major adverse events [83].
Preoperative measures to avoid graft failure include adequate anatomic characterization of coronary lesions in the cardiac catheterization laboratory [81]. During surgery, intraoperative measures such as avoidance of distention, no-touch technique, and minimizing trauma to the graft handling during harvesting and implantation are effective in preventing early graft failure but do not affect rates of late graft failure [86].
In the United States, the American College of Cardiology (ACC) Foundation/American Heart Association (AHA) Task Force advises that 100–325 mg per day of aspirin should be administered to patients undergoing CABG, preferably preoperatively, or within 6 h postoperatively and then continued indefinitely to help reduce the occurrence of vein graft closure (class I recommendation, level of evidence A). Clopidogrel is an accepted alternative in case of aspirin intolerance after CABG surgery as recommended by the ACC Foundation/AHA Task Force (class IIa recommendation, level of evidence C) [55]. The ACC/AHA guidelines recommend statin therapy for patient undergoing CABG with an LDL cholesterol goal of < 100 mg/dl and ≥ 30% lowering of LDL cholesterol level (class I recommendation, level of evidence C) [55]. Statin therapy is reported to be protective against death after CABG surgery noted from a retrospective analysis of an observational study of over 16,000 patients [87]. The beneficial effect of statin therapy is thought to be based on its inhibitory effects on smooth muscle cell proliferation and its anti-inflammatory effects, which result in decreased intimal hyperplasia formation [81]. We utilize dual antiplatelet therapy with aspirin 81 mg (lifelong) and Plavix® 75 mg (30 days) as well statin therapy for life. This regimen is started on post-operative day 1. Unfortunately, 50 years after the introduction of CABG, the rate of vein graft failure continues to remain high, which may be due to the greater severity of coronary disease in patients who are referred for bypass surgery in the era of percutaneous interventions [73].
SVG–Medical Management and PCI
The 2014 ESC/EACTS guidelines on myocardial revascularization and treatment strategies for vein graft failure recommend medical therapy, thrombectomy, redo bypass graft surgery, or balloon angioplasty with or without stent placement [88]. Per these guidelines, the most appropriate treatment modality for each individual depends on severity of symptoms, presence and extent of ischemia, and the relative benefits and risks involved, including the patient’s general condition and presence of patent arterial grafts.
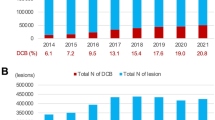
Balloon angioplasty alone has been shown to be effective in the treatment of vein graft failure, although high rates of restenosis and major adverse events have been reported [89, 90]. However, the results of balloon angioplasty in saphenous-vein bypass grafts are less favorable than those in native vessels, with rates of restenosis exceeding 50% [91]. The SAVED trial was the first study to compare balloon angioplasty with bare-metal stents on clinical outcomes. It showed that bare-metal stents reduced the need for revascularization of the target lesion and reduced major cardiac events compared with balloon angioplasty [91]. Further studies have not shown benefit comparing the use of balloon angioplasty alone vs. balloon angioplasty with either a bare-metal stent or drug-eluting stent in the treatment of vein graft failure. In additional attempts to address the ideal management of SVG lesions, the DIVA study conducted in the VA health system compared bare-metal stent (BMS) to drug-eluting stent (DES) placement. This trial enrolled 599 patients randomly assigned to receive either DES or BMS placement for de novo SVG lesions. At 12 months, the rate of target vessel failure was similar across the two groups (17% for DES vs. 19% for BMS) and no significant differences were found regarding serious adverse events or stent thrombosis [92]. No specific recommendations have been made by either the European Society of Cardiology Guidelines or the ACC/AHA Guidelines for revascularization after CABG [55, 88]. In clinical practice, balloon angioplasty with DES placement is the most frequently used technique for vein graft failures, however this may be called into question given results of the DIVA trial as discussed above [92, 93].
A study by Brilakis et al. showed that patients undergoing bypass graft interventions (in either arterial grafts or SVGs) had higher in-hospital mortality compared with patients who underwent native coronary artery interventions. Their team used data from the National Cardiovascular Data Registry CathPCI Registry to evaluate contemporary patterns of PCI in prior CABG patients to identify factors associated with PCI in native coronary arteries vs. bypass grafts as well as to examine in hospital clinical outcomes [94]. They showed that most PCIs performed in prior CABG patients are done in native coronary artery lesions, although SVG PCI becomes more prevalent with longer time intervals from CABG. Compared with native coronary PCI, bypass graft PCI was noted to be independently associated with higher in-hospital mortality [94]. A similar study in a national cohort of over 11,000 veterans with prior CABG undergoing PCI to bypass grafts revealed higher incidence of short- and long-term major adverse events, including more than double the rate of in-hospital mortality compared to native coronary artery PCI. During a median follow-up period of 3.11 years, bypass graft PCI was associated with significantly higher mortality (adjusted HR 1.30; 95% confidence interval: 1.18–1.42), MI (adjusted HR 1.61; 95% confidence interval: 1.43–1.82), and repeat revascularization (adjusted HR 1.60; 95% confidence interval: 1.50–1.71) [95].
An additional treatment consideration is the choice of vein graft intervention versus an attempt at revascularization through native vessel complete total occlusion (CTO) PCI. Following CABG, atherosclerosis or thrombosis of native vessels is increased with an estimated 43% of bypassed native coronary arteries progressing to CTOs as early as 1 year following CABG [96]. Several challenges exist when considering CTO intervention in post-CABG patients compared to non-CABG. In a large, single-center CTO program, CTO lesions in post-CABG patients were more complex (longer, more angulated, more calcified) and more often had blunt proximal cap. Despite these characteristics, success rates for these operators were similar between post-CABG and native CTO interventions at 90% and 93%, respectively. Additionally, CTO intervention on post-CABG patients was not associated with higher short-term risk, but these patents did experience increased risk of MACE at 1 year compared with non-CABG CTO [97]. With ongoing advancements in the field of CTO interventions, options for revascularization strategy have increased. Below is a figure displaying our general approach to management of vein graft lesions incorporating CTO intervention, Fig. 2.
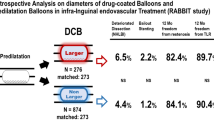
Another complex pathology to manage is the stenotic lesion at the distal bypass anastomoses. Robust clinical trials are lacking regarding optimal treatment strategies. Given that there is often size mismatch between the graft and the native vessel, optimal stent deployment is challenging, and therefore some proceduralists opt for angioplasty with drug-coated balloons.
Use of Proximal Anastomotic Markers (PAMS) in CABG
Coronary angiography in patients who have undergone previous CABG poses unique challenges due to potential uncertainty in the number and exact location of proximal anastomoses of aortocoronary grafts, which can lead to patients receiving increased does of fluoroscopic radiation and intravenous contrast to obtain a satisfactory exam [98]. Proximal anastomotic markers (PAMs), composed of a variety of materials, including standard surgical clips, metal or radiopaque silicone rings, segments of stainless-steel wire, segments of the radiopaque monofilament thread used in surgical sponges, or other materials, can be affixed adjacent to or circumferentially around proximal anastomoses of aortocoronary bypass grafts to facilitate their fluoroscopic identification [99, 100].
The presence of PAMs reduces fluoroscopy time and contrast dose at post-CABG coronary angiography [101, 102]. Despite these benefits, a 1998 survey of the STS membership by Eisenhauer et al. revealed that only 60% of surgeons routinely inserted PAMs at CABG [103]. The most commonly-cited reasons for their omission were a lack of perceived benefit and an unknown effect on graft patency. Concerns about foreign-body reaction affecting graft patency and/or difficulty of redo sternotomy were also raised. Contemporary to this survey was another report by Eisenhauer et al. describing a retrospective review of angiograms performed after CABG in 335 patients with a total of 311 circumferentially “marked” and 405 “unmarked” grafts reporting significantly higher patency rates of marked grafts at ≤ 1 year (90.0 vs. 46.9%) and > 1 to ≤ 5 years (80.0 vs. 59.7%) post-CABG, suggesting that the placement of circumferential PAMs did not significantly affect graft patency in this retrospective, single-center cohort [103].
More recent studies have provided further insight into the effect of PAMs on graft patency. Olenchock et al. reported a post hoc analysis of the PREVENT IV cohort comparing graft patency and clinical outcomes in patients with PAMs and those without [104]. PAMs were present in 51.2% of evaluable patients (n = 910) and in 52.3% of SVGs (n = 2228). The rates of SVG stenosis ≥ 70%, ostial stenosis, and long-term mortality and/or MI did not differ significantly between patients receiving PAMs and those not. However, there was a significant increase in the rate of periop CABG MI (defined as creatine kinase MB ≥ 10 times the upper limit of normal with new > 30-ms Q waves in two contiguous leads within 24 h of surgery not attributable to preoperative MI) in patients receiving PAM (10.1 vs. 5.5%, p = 0.021). The authors did not have a clear explanation for this unanticipated finding but suggested that it may have been related to local flow disturbance leading to platelet aggregation and distal embolization or to inflammation caused by foreign-body reaction.
Pingpoh et al. reported a retrospective observational study of 1378 patients (n = 331 with PAMs, n = 1047 without) with history of CABG who underwent first post-CABG cardiac angiography a single center from 2005–2016 to evaluate the effect of PAM on post-CABG angiography. The presence of PAMs was associated with significant comparative reductions in duration of angiography, fluoroscopy time, and contrast dose. There was also no relationship between the presence of PAMs and vein graft patency at a mean of 112 (with PAM) to 115 (without PAM) months of follow-up [98].
There do not appear to be any strict contraindications to the use of PAMs. However, a number of subjective considerations may make their use undesirable. If subsequent redo sternotomy is anticipated, the placement of one or more PAMs may create a severe local inflammatory reaction at the site of future cross clamp application or aortotomy for aortic valve replacement. If the tissue quality at a proximal anastomosis is marginal, further local tissue manipulation required for PAMs placement creates the risk for additional bleeding or anastomotic injury. The survey of STS membership by Eisenhauer described several PAM-related complications reported by > 1% of respondents, including “kink, stenosis, or fibrosis at graft ostia,” “makes redo [sternotomy] difficult,” and “aortic erosion.” A number of single catastrophic events were also reported, including “temporary pacing wire pulled through marker and tore aorta when pulled postoperatively,” “sponge/ instrument caught on marker causing bleeding,” and “sternal saw caught on marker and tore aorta” [103]. Avoidance of these and related issues may prompt surgeons not to place PAMs.
Overall, PAMs appear to be beneficial in post-CABG angiography but their exact effect on perioperative MI and long-term graft patency is unclear. The studies reporting that PAM has no negative effect on these outcomes are based on single-center retrospective data, whereas the finding of increased rates of perioperative MI comes from a prospective randomized multi-center cohort with protocoled angiographic follow-up. Based on available evidence, the placement of PAMs at CABG should be considered, but decisions regarding implementation should be individualized based on patient factors and the joint preferences of surgeons and referring cardiologists.
Conclusions
Atherosclerotic coronary artery disease, the resultant ischemic cardiomyopathy, and related sequela comprise the leading cause of death worldwide and is not projected to diminish in the foreseeable future. Therefore, medical professionals involved in percutaneous and surgical coronary revascularization will continue to discuss, study, and reassess the efficacy and overall impact on survival and quality of life of many of the topics highlighted in this publication. The documented improved long-term patency rates of the internal mammary arteries and the radial artery have prompted vigorous discussion amongst cardiac surgeons globally and practice patterns that have increasingly favored all arterial revascularization especially in younger patients. Despite this movement, the saphenous vein as a coronary bypass graft remains the most common conduit in use today. Whether it is harvested via open or by endovascular technique, the inferior long-term patency rates as compared to arterial conduits necessitates reintervention by redo bypass surgery or percutaneous intervention on the graft itself or the native coronary circulation. Strategies to mitigate the well-documented fate of the saphenous vein graft and improve the overall patency of arterial bypass conduits will continue to evolve. Ultimately, the long-term clinical outcomes after coronary artery bypass surgery are a result of the complex interplay involving conduit selection, handling and salvage, bypass technique, surgeon and center experience, patient factors and compliance, as well postoperative medical therapy.
References
Cardiovascular Diseases. WHO Fact Sheet. 2017 www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds). Accessed 27 July 2020.
Epstein AJ, Polsky D, Yang F, Yang L, Groeneveld PW. Coronary revascularization trends in the United States, 2001–2008. JAMA. 2011;305:1769–76.
Stuntz M, Palak A. Recent trends in percutaneous coronary intervention volume in the United States [abstract]. Value Health. 2016;19:A641.
Weiss AJ, Elixhauser A. Trends in operating room procedures in U.S. hospitals, 2001–2011: Statistical Brief #171. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD), 2006.
Martinez-Gonzalez B, Reyes-Hernandez CG, Quiroga-Garza A, et al. Conduits used in coronary artery bypass grafting: a review of morphological studies. Ann Thorac Cardiovasc Surg. 2017;23:55–65.
Otsuka F, Yahagi K, Sakakura K, Virmani R. Why is the mammary artery so special and what protects it from atherosclerosis? Ann Cardiothorac Surg. 2013;2:519–26.
Hlatky MA, Boothroyd DB, Reitz BA, Shilane DA, Baker LC, Go AS. Adoption and effectiveness of internal mammary artery grafting in coronary artery bypass surgery among Medicare beneficiaries. J Am Coll Cardiol. 2014;63:33–9.
ElBardissi AW, Aranki SF, Sheng S, O’Brien SM, Greenberg CC, Gammie JS. Trends in isolated coronary artery bypass grafting: an analysis of the Society of Thoracic Surgeons adult cardiac surgery database. J Thorac Cardiovasc Surg. 2012;143:273–81.
Gaudino M, Taggart D, Suma H, Puskas JD, Crea F, Massetti M. The choice of conduits in coronary artery bypass surgery. J Am Coll Cardiol. 2015;66:1729–37.
Buttar SN, Yan TD, Taggart DP, Tian DH. Long-term and short-term outcomes of using bilateral internal mammary artery grafting versus left internal mammary artery grafting: a meta-analysis. Heart. 2017;103:1419–26.
Taggart DP, Lees B, Gray A, et al. Protocol for the Arterial Revascularisation Trial (ART). A randomised trial to compare survival following bilateral versus single internal mammary grafting in coronary revascularisation [ISRCTN46552265]. Trials. 2006. https://doi.org/10.1186/1745-6215-7-7.
Taggart DP, Benedetto U, Gerry S, et al. Bilateral versus single internal-thoracic-artery grafts at 10 years. N Engl J Med. 2019;380:437–46.
Gaudino MFL, Taggart DP, Fremes SE. The ROMA trial: why it is needed. Curr Opin Cardiol. 2018;33:622–6.
Bjork VO, Ekestrom S, Henze A, Ivert T, Landou C. Early and late patency of aortocoronary vein grafts. Scand J Thorac Cardiovasc Surg. 1981;15:11–21.
Virk HUH, Lakhter V, Ahmed M, Brian OM, Chatterjee S. Radial artery versus saphenous vein grafts in coronary artery bypass surgery: a literature review. Curr Cardiol Rep. 2019;21:36.
Tranbaugh RF, Dimitrova KR, Friedmann P, et al. Coronary artery bypass grafting using the radial artery: clinical outcomes, patency, and need for reintervention. Circulation. 2012;126:S170–5.
Khot UN, Friedman DT, Pettersson G, Smedira NG, Li J, Ellis SG. Radial artery bypass grafts have an increased occurrence of angiographically severe stenosis and occlusion compared with left internal mammary arteries and saphenous vein grafts. Circulation. 2004;109:2086–91.
Possati G, Gaudino M, Prati F, et al. Long-term results of the radial artery used for myocardial revascularization. Circulation. 2003;108:1350–4.
Gaudino M, Tondi P, Benedetto U, et al. Radial artery as a coronary artery bypass conduit: 20-year results. J Am Coll Cardiol. 2016;68:603–10.
Ando G, Capodanno D. Radial access reduces mortality in patients with acute coronary syndromes: results from an updated trial sequential analysis of randomized trials. JACC Cardiovasc Interv. 2016;9:660–70.
Jolly SS, Amlani S, Hamon M, Yusuf S, Mehta SR. Radial versus femoral access for coronary angiography or intervention and the impact on major bleeding and ischemic events: a systematic review and meta-analysis of randomized trials. Am Heart J. 2009;157:132–40.
Kamiya H, Ushijima T, Kanamori T, et al. Use of the radial artery graft after transradial catheterization: is it suitable as a bypass conduit? Ann Thorac Surg. 2003;76:1505–9.
Yonetsu T, Kakuta T, Lee T, et al. Assessment of acute injuries and chronic intimal thickening of the radial artery after transradial coronary intervention by optical coherence tomography. Eur Heart J. 2010;31:1608–15.
Mounsey CA, Mawhinney JA, Werner RS, Taggart DP. Does previous transradial catheterization preclude use of the radial artery as a conduit in coronary artery bypass surgery? Circulation. 2016;134:681–8.
Burstein JM, Gidrewicz D, Hutchison SJ, Holmes K, Jolly S, Cantor WJ. Impact of radial artery cannulation for coronary angiography and angioplasty on radial artery function. Am J Cardiol. 2007;99:457–9.
Puskas JD, Williams WH, Duke PG, et al. Off-pump coronary artery bypass grafting provides complete revascularization with reduced myocardial injury, transfusion requirements, and length of stay: a prospective randomized comparison of two hundred unselected patients undergoing off-pump versus conventional coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2003;125:797–808.
Shroyer AL, Grover FL, Hattler B, et al. On-pump versus off-pump coronary-artery bypass surgery. N Engl J Med. 2009;361:1827–37.
Shroyer AL, Hattler B, Grover FL. Five-year outcomes after on-pump and off-pump coronary-artery bypass. N Engl J Med. 2017;377:1898–9.
Lamy A, Devereaux PJ, Prabhakaran D, et al. Off-pump or on-pump coronary-artery bypass grafting at 30 days. N Engl J Med. 2012;366:1489–97.
Lamy A, Devereaux PJ, Prabhakaran D, et al. Effects of off-pump and on-pump coronary-artery bypass grafting at 1 year. N Engl J Med. 2013;368:1179–88.
Lamy A, Devereaux PJ, Prabhakaran D, et al. Five-year outcomes after off-pump or on-pump coronary-artery bypass grafting. N Engl J Med. 2016;375:2359–68.
Diegeler A, Reents W, Zacher M. Off-pump or on-pump coronary-artery bypass grafting. N Engl J Med. 2013;369:196–7.
Diegeler A, Börgermann J, Kappert U, et al. Five-year outcome after off-pump or on-pump coronary artery bypass grafting in elderly patients. Circulation. 2019;139:1865–71.
Benedetto U, Lau C, Caputo M, et al. Comparison of outcomes for off-pump versus on-pump coronary artery bypass grafting in low-volume and high-volume centers and by low-volume and high-volume surgeons. Am J Cardiol. 2018;121:552–7.
Gaudino M, Benedetto U, Bakaeen F, et al. Off- versus on-pump coronary surgery and the effect of follow-up length and surgeons’ experience: a meta-analysis. J Am Heart Assoc. 2018;7:e010034.
Puskas JD, Gaudino M, Taggart DP. Experience is crucial in off-pump coronary artery bypass grafting. Circulation. 2019;139:1872–5.
Caliskan E, de Souza DR, Boning A, et al. Saphenous vein grafts in contemporary coronary artery bypass graft surgery. Nat Rev Cardiol. 2020;17:155–69.
Zenati MA, Bhatt DL, Bakaeen FG, et al. Randomized trial of endoscopic or open vein-graft harvesting for coronary-artery bypass. N Engl J Med. 2019;380:132–41.
Deppe AC, Liakopoulos OJ, Choi YH, et al. Endoscopic vein harvesting for coronary artery bypass grafting: a systematic review with meta-analysis of 27,789 patients. J Surg Res. 2013;180:114–24.
Gulack BC, Kirkwood KA, Shi W, et al. Secondary surgical-site infection after coronary artery bypass grafting: a multi-institutional prospective cohort study. J Thorac Cardiovasc Surg. 2018;155(1555–1562):e1.
Williams JB, Peterson ED, Brennan JM, et al. Association between endoscopic vs. open vein-graft harvesting and mortality, wound complications, and cardiovascular events in patients undergoing CABG surgery. JAMA. 2012;308:475–84.
Kodia K, Patel S, Weber MP, et al. Graft patency after open versus endoscopic saphenous vein harvest in coronary artery bypass grafting surgery: a systematic review and meta-analysis. Ann Cardiothorac Surg. 2018;7:586–97.
Lopes RD, Hafley GE, Allen KB, et al. Endoscopic versus open vein-graft harvesting in coronary-artery bypass surgery. N Engl J Med. 2009;361:235–44.
Krishnamoorthy B, Critchley WR, Thompson AJ, et al. Study comparing vein integrity and clinical outcomes in open vein harvesting and 2 types of endoscopic vein harvesting for coronary artery bypass grafting: The VICO randomized clinical trial (Vein Integrity and Clinical Outcomes). Circulation. 2017;136:1688–702.
Ferdinand FD, MacDonald JK, Balkhy HH, et al. Endoscopic conduit harvest in coronary artery bypass grafting surgery: an ISMICS Systematic Review and Consensus Conference Statements. Innovations (Phila). 2017;12:301–19.
Johansson BL, Souza DS, Bodin L, et al. Slower progression of atherosclerosis in vein grafts harvested with “no touch” technique compared with conventional harvesting technique in coronary artery bypass grafting: An angiographic and intravascular ultrasound study. Eur J Cardiothorac Surg. 2010;38:414–9.
Samano N, Geijer H, Liden M, Fremes S, Bodin L, Souza D. The no-touch saphenous vein for coronary artery bypass grafting maintains a patency, after 16 years, comparable to the left internal thoracic artery: a randomized trial. J Thorac Cardiovasc Surg. 2015;150:880–8.
Sepehripour AH, Jarral OA, Shipolini AR, McCormack DJ. Does a “no-touch” technique result in better vein patency? Interact Cardiovasc Thorac Surg. 2011;13:626–30.
Wallgren S, Nielsen S, Pan E, et al. A single sequential snake saphenous vein graft versus separate left and right vein grafts in coronary artery bypass surgery: a population-based cohort study from the SWEDEHEART registry. Eur J Cardiothorac Surg. 2019;56:518–25.
Park SJ, Kim HJ, Kim JB, et al. Sequential versus individual saphenous vein grafting during coronary arterial bypass surgery. Ann Thorac Surg. 2020;109:1165–73.
Nordgaard H, Vitale N, Haaverstad R. Transit-time blood flow measurements in sequential saphenous coronary artery bypass grafts. Ann Thorac Surg. 2009;87:1409–15.
Kim HJ, Lee TY, Kim JB, et al. The impact of sequential versus single anastomoses on flow characteristics and mid-term patency of saphenous vein grafts in coronary bypass grafting. J Thorac Cardiovasc Surg. 2011;141:750–4.
Li J, Liu Y, Zheng J, et al. The patency of sequential and individual vein coronary bypass grafts: a systematic review. Ann Thorac Surg. 2011;92:1292–8.
Mehta RH, Ferguson TB, Lopes RD, et al. Saphenous vein grafts with multiple versus single distal targets in patients undergoing coronary artery bypass surgery: one-year graft failure and five-year outcomes from the Project of Ex-Vivo Vein Graft Engineering via Transfection (PREVENT) IV trial. Circulation. 2011;124:280–8.
Hillis LD, Smith PK, Anderson JL, et al. 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011;124:e652-735.
Sousa-Uva M, Neumann FJ, Ahlsson A, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur J Cardiothorac Surg. 2019;55:4–90.
Cameron A, Kemp HG Jr, Green GE. Bypass surgery with the internal mammary artery graft: 15-year follow-up. Circulation. 1986;74:30–6.
English JA, Carell ES, Guidera SA, Tripp HF. Angiographic prevalence and clinical predictors of left subclavian stenosis in patients undergoing diagnostic cardiac catheterization. Catheter Cardiovasc Interv. 2001;54:8–11.
Rogers JH, Calhoun RF 2nd. Diagnosis and management of subclavian artery stenosis prior to coronary artery bypass grafting in the current era. J Card Surg. 2007;22:20–5.
Haj Bakri M, Nasser M, Al SL. Endovascular treatment of coronary subclavian steal syndrome complicated with STEMI and VF: A case report and review of the literature. Clin Case Rep. 2018;6:2482–9.
Feit A, Reddy CV, Cowley C, Ibrahim B, Zisbrod Z. Internal mammary artery angiography should be a routine component of diagnostic coronary angiography. Cathet Cardiovasc Diagn. 1992;25:85–90.
Prager RJ, Akin JR, Akin GC, Binder RJ. Winslow’s pathway: a rare collateral channel in infrarenal aortic occlusion. AJR Am J Roentgenol. 1977;128:485–7.
Bates MC, Broce M, Lavigne PS, Stone P. Subclavian artery stenting: factors influencing long-term outcome. Catheter Cardiovasc Interv. 2004;61:5–11.
Ochoa VM, Yeghiazarians Y. Subclavian artery stenosis: a review for the vascular medicine practitioner. Vasc Med. 2011;16:29–34.
Olsen CO, Dunton RF, Maggs PR, Lahey SJ. Review of coronary-subclavian steal following internal mammary artery-coronary artery bypass surgery. Ann Thorac Surg. 1988;46:675–8.
Marshall WG Jr, Miller EC, Kouchoukos NT. The coronary-subclavian steal syndrome: report of a case and recommendations for prevention and management. Ann Thorac Surg. 1988;46:93–6.
Halabi AR, Alexander JH, Shaw LK, et al. Relation of early saphenous vein graft failure to outcomes following coronary artery bypass surgery. Am J Cardiol. 2005;96:1254–9.
Canos DA, Mintz GS, Berzingi CO, et al. Clinical, angiographic, and intravascular ultrasound characteristics of early saphenous vein graft failure. J Am Coll Cardiol. 2004;44:53–6.
Yanagawa B, Algarni KD, Singh SK, et al. Clinical, biochemical, and genetic predictors of coronary artery bypass graft failure. J Thorac Cardiovasc Surg. 2014;148(515–520):e2.
Kulik A, Ruel M. Statins and coronary artery bypass graft surgery: preoperative and postoperative efficacy and safety. Expert Opin Drug Saf. 2009;8:559–71.
Christenson JT. Preoperative lipid control with simvastatin reduces the risk for graft failure already 1 year after myocardial revascularization. Cardiovasc Surg. 2001;9:33–43.
Efird JT, O’Neal WT, Gouge CA, et al. Implications of hemodialysis in patients undergoing coronary artery bypass grafting. Int J Cardiovasc Res. 2013;2:1000154.
Parang P, Arora R. Coronary vein graft disease: pathogenesis and prevention. Can J Cardiol. 2009;25:e57-62.
Harskamp RE, Lopes RD, Baisden CE, de Winter RJ, Alexander JH. Saphenous vein graft failure after coronary artery bypass surgery: pathophysiology, management, and future directions. Ann Surg. 2013;257:824–33.
Cox JL, Chiasson DA, Gotlieb AI. Stranger in a strange land: The pathogenesis of saphenous vein graft stenosis with emphasis on structural and functional differences between veins and arteries. Prog Cardiovasc Dis. 1991;34:45–68.
Motwani JG, Topol EJ. Aortocoronary saphenous vein graft disease: pathogenesis, predisposition, and prevention. Circulation. 1998;97:916–31.
Yahagi K, Kolodgie FD, Otsuka F, et al. Pathophysiology of native coronary, vein graft, and in-stent atherosclerosis. Nat Rev Cardiol. 2016;13:79–98.
Goldman S, Zadina K, Moritz T, et al. Long-term patency of saphenous vein and left internal mammary artery grafts after coronary artery bypass surgery: results from a Department of Veterans Affairs Cooperative Study. J Am Coll Cardiol. 2004;44:2149–56.
Lardenoye JH, de Vries MR, Lowik CW, et al. Accelerated atherosclerosis and calcification in vein grafts: a study in APOE*3 Leiden transgenic mice. Circ Res. 2002;91:577–84.
Owens CD, Wake N, Jacot JG, et al. Early biomechanical changes in lower extremity vein grafts–distinct temporal phases of remodeling and wall stiffness. J Vasc Surg. 2006;44:740–6.
de Vries MR, Simons KH, Jukema JW, Braun J, Quax PH. Vein graft failure: from pathophysiology to clinical outcomes. Nat Rev Cardiol. 2016;13:451–70.
Szilagyi DE, Smith RF, Elliott JP. Venous autografts in femoropopliteal arterioplasty. Observations in the treatment of occlusive disease. Arch Surg. 1964;89:113–25.
Thielmann M, Massoudy P, Jaeger BR, et al. Emergency re-revascularization with percutaneous coronary intervention, reoperation, or conservative treatment in patients with acute perioperative graft failure following coronary artery bypass surgery. Eur J Cardiothorac Surg. 2006;30:117–25.
Jain U. Myocardial infarction during coronary artery bypass surgery. J Cardiothorac Vasc Anesth. 1992;6:612–23.
Rasmussen C, Thiis JJ, Clemmensen P, et al. Significance and management of early graft failure after coronary artery bypass grafting: feasibility and results of acute angiography and re-re-vascularization. Eur J Cardiothorac Surg. 1997;12:847–52.
Chiu JJ, Chien S. Effects of disturbed flow on vascular endothelium: pathophysiological basis and clinical perspectives. Physiol Rev. 2011;91:327–87.
Venkatesan S, Okoli GN, Mozid AM, et al. Effects of five preoperative cardiovascular drugs on mortality after coronary artery bypass surgery: a retrospective analysis of an observational study of 16, 192 patients. Eur J Anaesthesiol. 2016;33:49–57.
Kolh P, Windecker S, Alfonso F, et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: the Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur J Cardiothorac Surg. 2014;46:517–92.
Eisenberg JA, Calligaro KD, Kolakowski S, et al. Is balloon angioplasty of peri-anastomotic stenoses of failing peripheral arterial bypasses worthwhile? Vasc Endovascular Surg. 2009;43:346–51.
Hindnavis V, Cho SH, Goldberg S. Saphenous vein graft intervention: a review. J Invasive Cardiol. 2012;24:64–71.
Savage MP, Douglas JS, Fischman DL, et al. Stent placement compared with balloon angioplasty for obstructed coronary bypass grafts. Saphenous Vein De Novo Trial Investigators. N Engl J Med. 1997;337:740–7.
Brilakis ES, Edson R, Bhatt DL, et al. Drug-eluting stents versus bare-metal stents in saphenous vein grafts: a double-blind, randomised trial. Lancet. 2018;391:1997–2007.
Brennan JM, Sketch MH Jr, Dai D, et al. Safety and clinical effectiveness of drug-eluting stents for saphenous vein graft intervention in older individuals: results from the Medicare-linked National Cardiovascular Data Registry((R)) CathPCI Registry((R)) (2005–2009). Catheter Cardiovasc Interv. 2016;87:43–9.
Brilakis ES, Rao SV, Banerjee S, et al. Percutaneous coronary intervention in native arteries versus bypass grafts in prior coronary artery bypass grafting patients: a report from the National Cardiovascular Data Registry. JACC Cardiovasc Interv. 2011;4:844–50.
Brilakis ES, O’Donnell CI, Penny W, et al. Percutaneous coronary intervention in native coronary arteries versus bypass grafts in patients with prior coronary artery bypass graft surgery: insights from the Veterans Affairs Clinical Assessment, Reporting, and Tracking program. JACC Cardiovasc Interv. 2016;9:884–93.
Pereg D, Fefer P, Samuel M, et al. Native coronary artery patency after coronary artery bypass surgery. JACC Cardiovasc Interv. 2014;7:761–7.
Dautov R, Manh CN, Altisent O, Gibrat C, Rinfret S. Recanalization of chronic total occlusions in patients with previous coronary bypass surgery and consideration of retrograde access via saphenous vein grafts. Circ Cardiovasc Interv. 2016;9:e003515.
Pingpoh C, Siepe M, Burger K, et al. Impact of proximal radiopaque coronary bypass graft markers on post-bypass surgery coronary angiography. J Thorac Cardiovasc Surg. 2018;155:1565–72.
Cikirikcioglu M, Duran E. New discussion on an old subject: proximal anastomosis markers in coronary bypass surgery. Ann Thorac Surg. 2008;86:1401–2.
Nunes CF, Bolooki H. Aorta-coronary graft anastomosis marker: more than 30 years of experience. J Thorac Cardiovasc Surg. 2005;130:583–4.
Eisenhauer MD, Collier E 3rd, Eisenhauer TL, Cambier PA. Beneficial impact of aorto-coronary graft markers on post-operative angiography. Cathet Cardiovasc Diagn. 1997;40:249–53.
Peterson LR, McKenzie CR, Ludbrook PA, et al. Value of saphenous vein graft markers during subsequent diagnostic cardiac catheterization. Ann Thorac Surg. 1999;68:2263–6.
Eisenhauer MD, Wicks AB, Olson JP, Heric B. Prevalence of aortocoronary graft marker use and the factors affecting this decision. J Card Surg. 1998;13:194–9.
Olenchock SA Jr, Karmpaliotis D, Gibson WJ, et al. Impact of saphenous vein graft radiographic markers on clinical events and angiographic parameters. Ann Thorac Surg. 2008;85:520–4.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Brian McNichols, John Spratt, Jerin George, Scott Rizzi, Eddie Ward Manning III, and Ki Park have nothing to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Data Availability
Data sharing is not applicable to this article, as no datasets were generated or analyzed during the current study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
McNichols, B., Spratt, J.R., George, J. et al. Coronary Artery Bypass: Review of Surgical Techniques and Impact on Long-Term Revascularization Outcomes. Cardiol Ther 10, 89–109 (2021). https://doi.org/10.1007/s40119-021-00211-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40119-021-00211-z