Abstract
Background
Parkinson’s disease is a progressive neurodegenerative disease, which significantly impacts patients’ quality of life and is associated with high treatment and direct healthcare costs. In England, levodopa/carbidopa intestinal gel (LCIG) is indicated for the treatment of levodopa-responsive advanced Parkinson’s disease with troublesome motor fluctuations when available combinations of medicinal products are unsatisfactory.
Objective
We aimed to determine the cost effectiveness of LCIG compared to the standard of care for patients with advanced Parkinson’s disease in England, using real-world data.
Methods
A Markov model was adapted from previous published studies, using the perspective of the English National Health System and Personal and Social Services to evaluate the cost effectiveness of LCIG compared to standard of care in patients with advanced Parkinson’s disease over a 20-year time horizon. The model comprised 25 health states, defined by a combination of the Hoehn and Yahr scale, and waking time spent in OFF-time. The base case considered an initial cohort of patients with an Hoehn and Yahr score of ≥ 3, and > 4 h OFF-time. Standard of care comprised standard oral therapies, and a proportion of patients were assumed to be treated with subcutaneous apomorphine infusion or injection in addition to oral therapies. Efficacy inputs were based on LCIG clinical trials where possible. Resource use and utility values were based on results of a large-scale observational study, and costs were derived from the latest published UK data, valued at 2017 prices. The EuroQol five-dimensions-3-level (EQ-5D-3L) instrument was used to measure utilities. Costs and quality-adjusted life-years were discounted at 3.5%. Both deterministic and probabilistic sensitivity analyses were conducted.
Results
Total costs and quality-adjusted life-years gained for LCIG vs standard of care were £586,832 vs £554,022, and 2.82 vs 1.43, respectively. The incremental cost-effectiveness ratio for LCIG compared to standard of care was £23,649/quality-adjusted life-year. Results were sensitive to the healthcare resource utilisation based on real-world data, and long-term efficacy of LCIG.
Conclusions
The base-case incremental cost-effectiveness ratio was estimated to be within the acceptable thresholds for cost effectiveness considered for England.
Similar content being viewed by others
Advanced Parkinson’s disease poses a significant burden on patients and the National Health System owing to decreased quality of life, substantial economic burden and limited treatment options. |
The economic evaluation adresses several points of critique from health technology assessment bodies on previous economic evaluations in advanced Parkinson’s disease, and applies data from a recent, large, real-world dataset. |
Our analysis suggests that levodopa/carbidopa intestinal gel is likely to be a cost-effective option for patients who are unsuitable for, or have not responded to, other treatment options. Levodopa/carbidopa intestinal gel is associated with increased costs and gains in quality-adjusted life years, compared to standard of care (which includes oral treatments and/or treatment with apomorphine), resulting an an incremental cost-effectiveness ratio of £23,649/quality-adjusted life-year. Uncertainties due to limited data availability in advanced Parkinson’s disease have been accounted for in sensitivity analyses. |
1 Introduction
Parkinson’s disease (PD) is a chronic progressive neurodegenerative disease that manifests as bradykinesia, tremor, rigidity and postural instability, thereby affecting patients’ daily life activities [1, 2]. Although primarily considered a movement disorder, PD is associated with non-motor symptoms such as autonomic dysfunction, sleep disorders, cognitive decline and sensory abnormalities such as anosmia, vision problems and pain [3]. Age is a major risk factor for PD, which affects approximately 1% of the population aged over 60 years, with a continual increase in prevalence with advancing age [4, 5]. The global burden of PD has increased over the past decades [6]. According to an analysis using the Clinical Practice Research Datalink, the estimated prevalence of PD in the general population aged 45 years or over in the UK in 2018 was 18,641 [7]. Moreover, PD imposes a significant economic burden on the healthcare system owing to the associated medical costs that increase with disease severity [2, 8,9,10]. A cost analysis of PD in the UK found that mean costs attributable to PD rose steadily in the years following diagnosis, and were substantially higher for patients with indicators of advanced PD (aPD) [11].
The treatment of PD focuses on symptomatic management by dopamine replacement, owing to the absence of disease-modifying treatments [12,13,14]. Oral levodopa is the most effective and widely used treatment in early PD, and is combined with a dopa-decarboxylase inhibitor, carbidopa, to prevent the peripheral conversion of levodopa to dopamine [14, 15]. Advanced PD, or complex PD [16], is characterised by a narrowing therapeutic window and delayed gastric emptying, resulting in an unpredictable clinical response that presents with motor complications in a patient and increasing OFF-time (expressed as a proportion of the waking day when a patient experiences a loss of treatment effect) [17]. However, there is a lack of global consensus on the definition of aPD, with a number of indicators proposed, which may result in heterogeneity in care [18, 19]. Previous economic evaluations have used a combination of OFF-time, and the Hoehn and Yahr (HY) scale, which categorises PD according to five clinical stages based on the progression of motor symptoms [20,21,22,23,24,25,26,27].
Current management of aPD involves device-aided treatments such as subcutaneous apomorphine infusion, and deep brain stimulation (DBS) surgery, and levodopa/carbidopa intestinal gel (LCIG) [13, 17, 22]. However, patients who are over 70 years of age, cognitively impaired or have dysphagia are not considered suitable for DBS surgery [28]. Apomorphine is a dopamine agonist, considered as an abridged or rescue therapy, and can be associated with troublesome side effects such that it is not suitable for all patients [29]. Although used in clinical practice in England [13], its availability and usage vary between countries. Patients who are unsuitable or have failed apomorphine infusion or DBS surgery thus have limited treatment options.
Levodopa/carbidopa intestinal gel includes a combination of levodopa and carbidopa for continuous intestinal infusion in patients with aPD who are unresponsive to available combinations of pharmacological treatments [30]. Treatment is administered directly into the duodenum or upper jejunum by a nasogastric or percutaneous endoscopic gastrostomy tube with a portable infusion pump [30]. Levodopa/carbidopa intestinal gel is licensed in Europe for the treatment of levodopa-responsive aPD in individuals experiencing severe motor fluctuations and hyper-/dyskinesia [30], and was recommended for routine commissioning by the National Health Service (NHS) England in 2015 [31]. In England, LCIG is licensed for the treatment of advanced levodopa-responsive PD with severe motor fluctuations and hyper/dyskinesia when available combinations of medicinal products are unsatisfactory [32].
In an RCT comparing LCIG and oral immediate-release levodopa among patients with aPD, LCIG significantly reduced OFF-time compared with oral levodopa, and additionally increased ON-time without dyskinesia during the day [33]. Other recent clinical studies on the safety and efficacy of LCIG in aPD showed a significant reduction in OFF-time and an improvement in motor fluctuations, non-motor symptoms and consequently, an improvement in patients’ quality of life [34,35,36,37,38,39]. Findings from long-term studies show that the benefit of LCIG in reducing OFF-time is maintained over 5 years, at least [34,35,36, 40,41,42]. The economic analysis presented in this study was aligned with a 12-month open-label study of LCIG in patients with aPD and severe motor fluctuations (NCT00335153) [36].
Previous economic evaluations have analysed the cost effectiveness of LCIG with standard of care (SoC) [i.e., oral therapy with or without subcutaneous apomorphine infusion, and standard follow-up visits] in patients with aPD [20,21,22,23, 43]. These evaluations have been reviewed by various health technology assessment bodies and several areas for improvement have been highlighted, namely, the methodology used for calculating key inputs such as discontinuation rates and health-state transitions, and the lack of available data sources. For these reasons, an updated model is warranted.
This study aims to explore the cost effectiveness of LCIG relative to SoC in patients with aPD from NHS England and Personal and Social Services perspective, with an updated modelling approach consistent with the National Institute for Health and Care and Excellence (NICE) Decision Support Unit documents [44], and using a recent real-world dataset to inform cost and utility inputs.
2 Methodology
2.1 Population
Patient-level data from NCT00335153 were used to define the baseline distribution of patients according to age, sex and disease severity. A brief description of this trial is provided in the Electronic Supplementary Material (ESM). The trial eligibility criteria included severe motor fluctuations defined as ≥ 3 h of daily OFF-time, resulting in patients with 6.75 ± 2.35 (mean ± standard deviation) OFF-time in hours/day at baseline (N = 354) [36]. In compliance with the licensed indication for LCIG, the cost-effectiveness model population included patients with aPD and severe motor fluctuations, defined on the HY scale as HY ≥ 3 and OFF-time defined as > 4 h, or > 25% of a 16-h waking day [30]. The model inputs were based on the subgroup that meets these criteria, and had complete follow-up data (N = 196). The average age of LCIG cohort was 64 years and 59% of the cohort were male [36]. For the SoC arm, a hypothetical cohort was created to mirror the baseline LCIG cohort.
2.2 Comparator
In line with the current policy in England [32], patients who are suitable for LCIG treatment have not responded to or are inappropriate candidates for apomorphine infusion and DBS treatment. These patients are left with three options: reverting back to treatment with oral medications only, retrying apomorphine or initiating LCIG treatment. The model therefore compared LCIG with SoC, which includes oral PD medications with or without subcutaneous apomorphine infusion/injection [20]. Full details of the SoC medications included in the analysis are provided in the ESM.
2.3 Model Structure
A Markov model was developed, using NHS England and Personal and Social Services perspectives (Fig. 1), to determine the average costs, life-years (LYs), and quality-adjusted life years (QALYs) per patient associated with aPD, and thereby calculate the incremental cost-effectiveness ratio (ICER). The model structure was based on a previous model by Lowin et al., exploring the cost effectiveness of LCIG in an Irish setting [22]. The model redistributed the population into 25 combinations of disease-specific health states, comprising stages 1–5 of the HY scale and the amount of OFF-time experienced (assuming a 16-h waking day: OFF 0 = 0%, OFF I = 1–25%, OFF II = 26–50%, OFF III = 51–75%, OFF IV = 76–100%), and a death state. Patients were followed over a time horizon of 20 years, using 6-monthly cycles (including half-cycle correction). A discount rate of 3.5% was applied to costs and effects, in line with the NICE methods guide [45]. Patients receiving LCIG could experience improvement due to their treatment during the initial 12-month period, based on clinical trial data, but thereafter, they could only move to a more severe HY/OFF stage as LCIG is not disease modifying. Patients in the most severe state (HY5/OFFIV) at the end of the trial period were assumed to discontinue LCIG treatment. For all cycles, patients receiving SoC could transit to a more severe HY/OFF stage or remain in the current health state, as they did not experience any improvement over the course of the model horizon. This assumption was based on the license of LCIG as a treatment for patients who derive no clinical benefit from SoC medications [30, 32].
2.4 Clinical Inputs
2.4.1 Health-State Transitions
The initial treatment effect on improving HY stage and OFF time for patients receiving LCIG was estimated based on the advanced patient distribution to health state in trial NCT00335153 at baseline, 24 weeks (6 months), and 54 weeks (used for model input at 12 months) [36]. These estimates are based on patients with advanced disease at baseline (N = 196) with severe motor fluctuations (defined as HY ≥3 and OFF >25%). This is summarised in Table 1.
Following initial treatment, patients in the LCIG cohort move through the Markov model based on the HY transition probabilities (natural disease progression). The model incorporated the long-term benefit of LCIG treatment as reduced OFF-state progression, by estimating the relative risk of OFF progression for the LCIG cohort compared to the SoC cohort. This was calculated as 0.53 based on clinical data by calculating the ratio between the mean decreased OFF-time per day in the LCIG arm and the oral SoC arm at 12 weeks [33]. The assumption that the OFF-time benefit for LCIG is sustained over time is supported by clinical studies, which show sustained efficacy over 5 years, at least [34,35,36, 40,41,42].
Transition probabilities (i.e. natural disease progression) were applied from cycle 3 in the LCIG cohort and from cycle 1 in the SoC cohort. The HY-stage transition probabilities were obtained from a literature review of transition times, which were converted to per cycle probabilities [46]. The transition probabilities for OFF stages were estimated through weighted linear regression of results from published studies [47, 48]. Transitions probabilities for HY stages and OFF stages were assumed to be independent of each other.
2.4.2 Safety Data and Discontinuation
Device-specific adverse events associated with LCIG were included in the model based on clinical studies [34, 36]. Adverse events leading to tube replacement or repositioning were included (12.7% and 14.39% for the first two cycles, 11.9% and 16.4% for the subsequent cycles, for adverse events with and without surgery, respectively). For the initial 12 months, the discontinuation rate was estimated based on trial NCT00335153, resulting in a rate of 6.8% per 6-month cycle [36]. For the subsequent cycles, a long-term discontinuation rate of 3.5% per cycle was applied [34].
2.4.3 Mortality
Mortality was accounted for using all-cause mortality [49]. The model applied a mortality adjustment based on HY stage. Hazard ratios were based on published literature (hazard ratios: HY1–HY3 = 1.18, HY4 = 2.37, HY5 = 3.34) [46]. No additional mortality associated with OFF-time was incorporated.
2.5 Resource Use and Costing
2.5.1 Medication Costs and Associated Administrative Costs
Medication use for SoC and concomitant oral medication for patients receiving LCIG were obtained from the Adelphi Real-World Parkinson’s Disease Specific Programme (Adelphi-DSP) 2019 dataset [50]. Adelphi-DSP was a cross-sectional survey of physicians and patients in a real-world clinical setting. The Adelphi-DSP was conducted in seven countries (France, Germany, Italy, Japan, Spain, the UK and the USA) between 2017 and 2020. The DSP methodology has been previously published and validated [51]. Participating physicians completed a record form for the next 12 months consecutively for consulting patients meeting the eligibility criteria; the physician-reported questionnaire form contained questions on patients’ demographics, clinical assessments, clinical outcomes, medication use and history, healthcare resource utilisation and concomitant conditions. Each patient for whom the physician completed a form was then invited to complete a patient-reported questionnaire, which recorded demographics, current condition, level of satisfaction with their treatment and quality of life. If the patient had a caregiver, they were also invited to complete a form, reporting on demographics and burden of care.
The average daily doses of SoC medications as observed for UK patients (N = 856) in Adelphi-DSP were used to calculate an average cost per patient, sourced from the Monthly Index of Medical Specialties 2020 [50, 52], using the lowest price available for each formulation. Medication costs were further split by regimes containing apomorphine, and those taking oral medications only, estimating a proportion of patients on SoC treated with apomorphine. The model applied the list price of an LCIG cassette from the Monthly Index of Medical Specialties [52]. While all other costs in this analysis reflect the 2017 valuation year, the medication costs are valued at 2019 prices as they were sourced from the Monthly Index of Medical Specialties [52] (in the first quarter of 2020), which is published monthly.
Other costs associated with LCIG treatment included start-up costs, such as nasogastric and percutaneous endoscopic gastrostomy tube insertion, titration and monitoring, as well as the cost of device-specific adverse events and discontinuing treatment, in line with Lowin et al. [21]. Costs of healthcare services were obtained from the latest version (2017–18) of the NHS reference costs at the time of writing [53]. These costs reflect the 2017 valuation year. Resource use and cost inputs are summarised in Table 2. Full details of concomitant medications are provided in the ESM.
2.5.2 Costs Associated with Health States
Based on the Adelphi-DSP 2019 dataset, a series of regressions were conducted to inform the costs associated with the health states, by exploring the relationship between HY stage, OFF time and healthcare costs. The unit costs applied in the regressions were sourced from NHS and Personal Social Services Research Unit costs [53, 54]. These unit costs reflected the 2017 valuation year. Health-state-related costs included direct medical costs (i.e. hospitalisations, emergency room visits, consultations) and direct non-medical costs (i.e. professional caregiver, respite care). Respite care costs inputs were based on HY stage only, owing to a paucity of data.
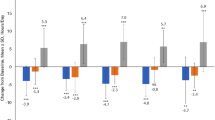
The costs regressions were performed to account for data paucity, particularly in the more severe OFF states (≥ OFF II), in the Adelphi-DSP 2019 UK dataset. The cost regressions were conducted by exploring several generalised linear models. The best-fitting model was chosen primarily based on the Akaike information criterion, and the significance of the coefficients corresponding to HY stage and OFF-time was also considered. Because of a large proportion of zero observations (i.e. no cost observed or reported for the patient during the 12 month study) for most variables considered, except consultations, a two-part regression model using a probit model was applied in combination with the generalised linear model to estimate the probability of incurring costs, as well as the mean positive expenditure. Because of data paucity, not all resulting model parameters were significant. Therefore, exploratory analyses were conducted by applying the regressions to different datasets (the combined Adelphi-DSP 2019 and 2012 UK data, the 2019 EU5 data and the 2019 G7 data) [50, 55]; dataset descriptions are provided in the ESM. However these additional analyses did not impact the significance of the estimated parameters, but resulted in different estimates, and additionally, were less sensitive to changes in OFF states. Therefore the original regressions were used to inform health-state costs. The cost regression outputs, showing the resulting estimated mean cost per patient used in the model are summarised in Fig. 2. The total cost represents the combined costs for all variables. A great proportion of the total cost was associated with professional care (comprising home help, therapists and nursing home staff, with the cost of nursing home staff being the most significant factor). Detailed outputs are provided in the ESM.
2.6 Utility Inputs
2.6.1 Health-State Utilities
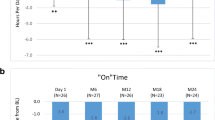
Because of a paucity of data for some health states, the utility estimates applied in the model were estimated from a linear mixed-model regression analysis. The analysis was based on EQ-5D-3L values (mapped to the UK-specific tariff [56]), from a combination of studies, which resulted in an increased sample size, improving the accuracy of the regression. The studies included the Adelphi-DSP study, combining both 2012 and 2019 UK datasets, LCIG clinical studies (NCT00335153, NCT00357994/NCT00660387, NCT00141518 [DAPHNE]) [33, 36, 57] and an LCIG observational study (the GLORIA registry) [35, 58], brief descriptions of the LCIG studies are provided in the ESM. This resulted in a combined dataset of 3862 patients. The outputs of the regression analysis indicated that an increase in HY stage or OFF stage is associated with a utility decrement of 0.110 and 0.071, respectively. Detailed outputs are provided in the ESM.
2.6.2 Caregiver Disutility
The impact of caregiver disutility associated with informal care was included in the model based on regression models, using combined Adelphi-DSP 2012 and 2019 datasets. First, the proportion of the patients in the dataset with an informal caregiver by each HY stage was estimated using a probit model. Second, the associated utility decrement was estimated based on a linear regression model, using patients’ HY stage and EQ-5D data. An increase in HY stage was estimated to result in a utility decrement of 0.023. Detailed outputs are provided in the ESM.
2.7 Handling of Uncertainty
2.7.1 Deterministic Sensitivity Analyses
Scenario analyses and one-way sensitivity analyses were conducted to assess the impact of uncertainties surrounding core model outputs. Key parameters were varied to identify the key drivers of the results (Fig. 3). The analysis was conducted using a net monetary benefit, using a willingness-to-pay (WTP) threshold of £30,000/QALY. Scenario analyses explored in the study included: (1) using alternative modelled cohorts: i.e. HY3/OFFI+ and HY3/OFFIII+; (2) assuming 20% of patients receiving SoC are treated with apomorphine to be consistent with a previous LCIG study [20]; (3) HY5/OFFIV patients allowed to continue LCIG treatment after the trial period; (4) excluding the caregiver disutilities from the analyses; and (5) making alternative assumptions regarding the long-term benefit, after the first 5 years in the model: i.e. assuming no benefit to LCIG cohort and progression rates are equal to the SoC cohort (a relative risk of 1 from year 6 onwards), and, alternatively, assuming the benefit of LCIG gradually wanes (the relative risk increases linearly from year 6 to year 20 from 0.53 to 1). Upper and lower limits for the univariate analyses applied 95% confidence intervals for the analysis where available. For parameters where there was no information regarding the uncertainties surrounding the source data, ranges varying from ±20% of the base-case values were applied. Summary tables for the deterministic sensitivity analyses are provided in the ESM.
2.7.2 Probabilistic Sensitivity Analysis
A probabilistic sensitivity analysis (PSA) was conducted to assess uncertainty related to model parameter values and to test the robustness of the model. Appropriate distributions were used (e.g. gamma for costs, beta for probabilities). Because of the non-linearity in the cost regression, health-state costs were varied uniformly within 20% of the estimated mean. The PSA was run over 10,000 iterations. For each iteration, the sampled values for each parameter generated a single estimate of expected costs, effects and net benefits. The costs and QALYs, generated in the PSA are presented (Fig. 4), as well as the proportion of analyses resulting in LCIG being cost effective at different WTP thresholds (Fig. 5).
2.8 Validation
Both internal and external validation were considered. With respect to internal validation, the current analysis is based on a well-established existing model structure; both the model structure and associated assumptions (described above) have been validated in previous studies [20,21,22,23,24,25,26]. Similarly, the model inputs have generally been validated in previous studies [20,21,22]. Where there are differences in inputs these are attributable either to updated data sources, or alternate methods for generating inputs, in an effort to improve internal validity. Therefore, the utility and resource-use inputs in the current analysis make use of the latest real-world evidence (Adelphi-DSP 2019) [50], and mortality and unit cost inputs are based on the latest respective UK data [49, 52, 53]. Similarly, as discussed above, both the natural history (OFF state) transition probabilities, and treatment effect (relative risk of OFF-state progression) associated with LCIG are based on updated methodologies. External validation was conducted by comparing the results of this analysis with the results of previous studies.
3 Results
3.1 Base-Case Results
In the base-case analysis, as compared to SoC, LCIG was associated with an incremental cost of £32,810, a QALY gain of 1.39 and a LY gain of 0.36 over a 20-year time horizon. The ICER per QALY gain was £23,649 and the ICER per LY gain was £90,349. The base-case results are summarised in Table 3, including a breakdown of the estimated costs. Levodopa/carbidopa intestinal gel was estimated to be associated with higher drug acquisition and administration costs than SoC. For all other costs, patients receiving SoC were estimated to have higher expenditure. There was a substantial cost saving of £157,853 associated with professional care.
3.2 Deterministic Sensitivity Analysis
The results of the one-way sensitivity analyses are presented as a tornado diagram in Fig. 3, showing key model parameters and scenarios and the incremental net monetary benefit using a WTP threshold of £30,000. Key drivers of the model were long-term efficacy of LCIG (after the first year), health-state costs from the cost regressions and the long-term discontinuation rate (after the first year).
Notably, LCIG was associated with an ICER of £29,637/QALY in a scenario analysis using a wider population (HY3+/OFFI), thus remaining cost effective at a WTP threshold of £30,000/QALY. Assuming a higher proportion of the SoC cohort were treated with apomorphine in addition to oral treatments impacted the results substantially in favour of LCIG, resulting in an ICER of £3970/QALY. The results remained relatively stable in response to assumptions regarding the long-term efficacy of LCIG (after 5 years). Assuming the effectiveness of LCIG and SoC are equal after 5 years results in an ICER of £31,801/QALY, and assuming a gradual waning in the effectiveness of LCIG after 5 years eventually (leading to parity with SoC by the end of the time horizon) results in an ICER of £25,390/QALY.
3.3 Probabilistic Sensitivity Analysis
Cost-effectiveness pairs generated in the PSA are shown in Fig. 4, and a cost-effectiveness acceptability plot is shown in Fig. 5. Most cost-effectiveness pairs lie in the north-east quadrant, where LCIG is associated with higher costs and greater QALY gain. Results also fall within the south-east quadrant, where LCIG is cost saving. This variability is largely due to varying the health-state costs, which are a key driver of the model. At a WTP threshold of £20,000, LCIG had a 40% probability of being cost effective, and at a WTP threshold of £30,000, LCIG had a 55% probability of being cost effective.
3.4 Validation
A comparison of the results of this analysis with previous analyses [20,21,22] showed consistency in terms of an increase both in costs and QALYs for LCIG compared with SoC, although there was an expected difference in the magnitude of the results. This is further discussed in Sect. 4.
4 Discussion
This study builds on methodologies employed by previously published models using a well-established model structure in aPD [20,21,22,23,24,25,26]. In the base case, it was estimated that LCIG was associated with higher QALYs and higher direct costs compared with SoC, resulting in an ICER of £23,649/QALY, which falls within the £20,000–30,000 cost-effectiveness threshold range specified by NICE [45]. Levodopa/carbidopa intestinal gel was overall associated with higher treatment costs, which accounted for the proportion of patients requiring a second cassette. However, a recent study showed that the average daily dose may be reduced with opicapone treatment [30]. The benefit of LCIG is driven by the slower OFF-time disease progression, and the initial treatment effect during the first year as estimated from clinical data, as patients spend more time in less severe health states. This results in higher utilities, and lower health-state-related costs (including hospitalisations, emergency room visits, consultations, respite care and professional care) over the time horizon. Treatment with LCIG resulted in great savings in professional care (in line with previous findings [59,60,61]), but other variables were less impactful.
The PSAs showed the result was generally robust. However, driven by the sensitivity of the ICER to changes in health-state costs, there were notable variations around the incremental overall costs that ranged from positive to negative (Fig. 4). The cost-effectiveness acceptability plot, therefore, showed that at a WTP threshold of £20,000, LCIG had a 40% probability of being cost effective, and at a WTP threshold of £30,000, LCIG had a 55% probability of being cost effective (Fig. 5). These findings are expected given that health-state costs are the primary contributor to the overall costs, accounting for 98% of the total cost for SoC, and 61% of the total cost of LCIG, notably professional care cost accounts for 89% of total costs for SoC, and 57% of the total costs for LCIG. Therefore, small variations in these costs result in considerable changes to the model results (Fig. 3). While a 40–55% probability of being cost effective (at the £20,000–£30,000 WTP threshold) is not high, reimbursement decision are not made purely based on cost effectiveness. Other factors, for example, disease burden, unmet needs and other socioeconomic factors (e.g. caregiver burden) are all considered during the decision-making process.
There is a lack of consensus on the definition of aPD, with a number of indicators suggested, based on uncontrolled motor and non-motor symptoms, and functional impairments [18, 62,63,64,65,66]. Studies have proposed ≥ 2 h OFF-time (i.e. 12.5% of waking time) as a key indicator that is measured in clinical practice [18, 19, 64,65,66]. Previous economic evaluations have used OFF-time > 8 h (50% of waking time) [20,21,22], and found LCIG to be cost effective compared with SoC. This analysis explored a wider population compared with those of the previously published studies, considering patients with OFF-time > 4 h (25% of waking time). This model cohort is a closer estimation of the trial NCT00335153 population: 78% of the total population match the current HY/OFF criteria (HY3+/OFFII+), compared with 26% in previous studies (HY3+/OFFIII+) [20,21,22]. In addition, scenario analyses estimated that LCIG was cost effective at a £30,000 WTP threshold for a wider population of HY3+/OFFI+, defined as having OFF-time >0%.
Previous analyses have estimated an increase in both costs and QALYs for LCIG compared with SoC. However, there is some variation in the magnitude due to various input sources. The cost-effectiveness analysis of LCIG vs SoC from the UK NHS perspective published in 2011 resulted in an ICER of £36,024/QALY for LCIG with a QALY gain of 1.10, while an adaptation published in 2018 for Scottish and Welsh settings resulted in an ICER of £52,110/QALY with a QALY gain of 1.26 [20, 21]. However, it should be noted that these analyses considered a more severe starting population of HY ≥ 3/OFF > 8 h compared with the current analysis (base case: HY ≥ 3/OFF > 4 h). Furthermore, by virtue of the use of the most recent Adelphi 2019 dataset [50], the health-state costs in the current analysis are generally higher compared with the two previous studies referenced. [20, 21]. In addition to using the most recent Adelphi dataset for costs and utilities, other influential inputs have been updated based on feedback from health technology assessment bodies; the methodology for estimating the OFF-stage transition probabilities was updated to account for missing data, and the LCIG treatment discontinuation rate was re-calculated to account for mortality. Overall, the current analysis is data driven and conservative where possible, for example, the percentage of patients receiving apomorphine treatment, in addition to oral SoC treatments, was estimated based on the overall cohort (including less severe HY and OFF stages) in the UK Adelphi dataset but this percentage may be higher for the severe cohort. A summary table of all previous cost-effectiveness analyses is provided in the ESM [13, 20,21,22,23, 43].
The costs and utilities associated with disease health states used in the model were informed by a novel analysis using the large, real-world, Adelphi-DSP 2019 dataset. This was considered the best available source available, and because of a paucity of data in the more severe health states, a regression analysis was considered the most appropriate method to inform these states. This is an established methodology to obtain information owing to a lack of data [67].
The cost-effectiveness analysis, however, has some limitations:
-
The assumption that SoC treatment has no benefit has been highlighted as a limitation by health technology assessment bodies. However, as the patient cohort considered are patients with severe disease who are left with no options other than LCIG, in line with the clinical pathway in England [13], these patients are therefore unlikely to accrue benefit from oral treatment. Based on this, the assumption that they follow natural disease progression was made and considered reasonable.
-
The assumption that OFF-time progression benefits associated with LCIG treatment are sustained long term has been noted as a source of uncertainty. However, long-term studies have demonstrated improvements in OFF-time after the initial 12 months, up to at least 5 years after baseline [34,35,36, 40,41,42]. In order to identify the impact of different scenarios of long-term efficacy of LCIG (from year 5 onwards), the model was tested for two more conservative scenarios:
-
1.
The effectiveness of LCIG and SoC are equal after 5 years: this scenario results in an ICER of £31,801/QALY (where the incremental QALY gain is 1.3 and the incremental cost is £41,305).
-
2.
A gradual waning in the effectiveness of LCIG after 5 years eventually leads to parity with SoC by the end of the time horizon: this scenario results in an ICER of £25,390/QALY (where the incremental QALY gain is 1.37 and the incremental cost is £34,678).
Although in both scenarios the QALYs gained are less than those gained in the base case, the ICER remains relatively insensitive. Given the sensitivity of results to assumptions regarding the long-term efficacy of LCIG after the initial 12-month period (Fig. 3), the relative insensitivity of results to long-term efficacy after 5 years suggest that result sensitivity is based more on the short-term outcomes. This is consistent with the fact that this model includes, and is sensitive to, constant treatment discontinuation (Fig. 3); meaning that a large proportion (~ 30%) of patients discontinue treatment before 5 years, and are unaffected by assumptions regarding LCIG efficacy after 5 years. In addition, the scenario assuming same effectiveness of LCIG as SoC after year 5 is an unlikely ‘worst-case’ scenario.
-
1.
-
Because of the nature of aPD, there are limited data available. Thus, there is uncertainty in the model as a result of limited data. For health-state costs in particular, there are very few observations in the Adelphi-DSP 2019 dataset for the more severe OFF-time states (≥ OFF II). Furthermore, the health-state costs are a key model driver (Fig. 3). In particular, the model is driven by the cost of professional care, which poses a significant burden in PD (in line with previous findings [64]), and is the largest proportion of the mean cost per patient in this analysis (89% of the total cost in the SoC arm, Table 3). If health-state costs are overestimated, given the effectiveness of LCIG modelled in this analysis, and the sensitivity of the results to health-state costs (Fig. 3), the ICER will be significantly underestimated (because of an increased cost saving for patients using LCIG in terms of health-state costs), and vice-versa. In an effort to mitigate against this uncertainty, regression analyses were performed, as already described. However, the limitation here is that some parameters estimated in the regressions were not significant. Because of few datapoints for the more severe states, the regression was highly dependent on the observed costs in these states, which also resulted in uncertainty and wide confidence intervals. In order to increase the number of data points, additional analyses were conducted on the combined UK Adelphi-DSP 2019 and 2012 dataset, as well as the 2019 EU5 and G7 datasets. These analyses did not impact the significance of the estimated parameters, but resulted in different estimates, and additionally, were less sensitive to changes in OFF states. Researchers have begun attempting to address the issue of estimating health-state costs in the more severe PD health states [68]; however, this is still an area that future analyses may wish to focus on as robust evidence is not yet available.
As the nature of disease progression in patients with PD varies considerably based on individual characteristics and treatment history, future analyses may wish to consider developing an individual patient-based simulation, allowing for individual patient histories to be recorded. Despite many advantages associated with this, to date, no PD models have been published using this approach because of greater data requirements. Populating these models may become feasible if more data become available.
5 Conclusions
The ICER of LCIG compared to SoC among patients with aPD was estimated to be within the WTP thresholds and deemed cost effective in the base case based on NICE criteria. The analysis estimated that LCIG treatment resulted in a substantial quality-of-life gain compared with SoC, and increased costs per patient, but with lower costs associated with disease severity.
The cost-effectiveness estimates are based on the best-available evidence. An increased evidence base on advanced PD may support future work. In particular, the availability of robust long-term outcome data, and data regarding the costs associated with more severe health states, in PD will reduce uncertainties associated with the analysis.
In England, LCIG is currently the only treatment option for patients with complex aPD who have not responded to, or are unsuitable for, apomorphine and DBS. The current economic analysis was conducted for a wider population than considered in previous LCIG cost-effectiveness studies. These findings may support the undertaking of further investigations of the benefits of earlier access to LCIG, in particular, for a less severe population than the current practice.
References
Michael J Fox Foundation for Parkinson’s Research. Parkinson's disease symptoms. https://www.michaeljfox.org/understanding-parkinsons/living-with-pd/topic.php?symptoms&navid=symptoms. Accessed 3 Feb 2022.
Martinez-Martin P, Rodrigurez-Blazquez C, Kurtis M, et al. The impact of non-motor symptoms on health-related quality of life of patients with Parkinson’s disease. Mov Disord. 2011;26(3):399–406.
Pfeiffer RF. Non-motor symptoms in Parkinson’s disease. Parkinsonism Relat Disord. 2016;22:S119–22.
Pringsheim T, Jette N, Frolkis A, et al. The prevalence of Parkinson’s disease: a systematic review and meta-analysis. Mov Disord. 2014;29(13):1583–90.
de Lau LM, Breteler MM. Epidemiology of Parkinson’s disease. Lancet Neurol. 2006;5(6):525–35.
GBD 2016 Parkinson’s Disease Collaborators. Global, regional, and national burden of Parkinson’s disease, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018;17(11):939–53.
Parkinson's UK. The incidence and prevalence of Parkinson's in the United Kingdom. 2018. https://www.parkinsons.org.uk/sites/default/files/2018-01/CS2960%20Incidence%20and%20prevalence%20report%20branding%20summary%20report.pdf. Accessed 3 Feb 2022.
von Campenhausen S, Winter Y, Silva A, et al. Costs of illness and care in Parkinson’s disease: an evaluation in six countries. Eur Neuropsychopharmacol. 2011;21(2):180–91.
Findley L, Aujla M, Bain P, et al. Direct economic impact of Parkinson’s disease: a research survey in the United Kingdom. Mov Disord. 2003;8(10):1139–45.
Deuschl G, Beghi E, Fazekas F, et al. The burden of neurological diseases in Europe: an analysis for the Global Burden of Disease Study 2017. Lancet Public Health. 2020;5(10):e551–67.
Weir S, Samnaliev M, Kuo T, et al. Short- and long-term cost and utilization of health care resources in Parkinson’s disease in the UK. Move Disord. 2018;33(6):974–81.
Poewe W, Seppi K, Tanner C, et al. Parkinson disease. Nat Rev Dis Primers. 2017;3(1):17013.
NICE. Guideline, Parkinson’s disease in adults (NG71). 2017. https://www.nice.org.uk/guidance/NG71. Accessed 3 Feb 2022.
Fox SH, Katzenschlager R, Lim S, et al. International Parkinson and movement disorder society evidence-based medicine review: update on treatments for the motor symptoms of Parkinson’s disease. Move Disord. 2018;33(8):1248–66.
Mercuri NB, Bernardi G. The “magic” of L-dopa: why is it the gold standard Parkinson’s disease therapy? Trends Pharmacol Sci. 2005;26(7):341–4.
Chaudhuri KR, Yates L, Martinez-Martin P. The non-motor symptom complex of Parkinson’s disease: a comprehensive assessment is essential. Curr Neurol Neurosci Rep. 2005;5(4):275–83.
Giugni JC, Okun MS. Treatment of advanced Parkinson’s disease. Curr Opin Neurol. 2014;27(4):450–60.
Antonini A, Stoessl A, Kleinman L, et al. Developing consensus among movement disorder specialists on clinical indicators for identification and management of advanced Parkinson’s disease: a multi-country Delphi-panel approach. Curr Med Res Opin. 2018;34(12):2063–73.
Fasano A, Fung V, Lopiano L, et al. Characterizing advanced Parkinson’s disease: OBSERVE-PD observational study results of 2615 patients. BMC Neurol. 2019;19(1):50.
Kalabina S, Belsey J, Pivonka D, et al. Cost-utility analysis of levodopa carbidopa intestinal gel (Duodopa) in the treatment of advanced Parkinson’s disease in patients in Scotland and Wales. J Med Econ. 2019;22(3):215–25.
Lowin J, Bergman A, Chaudhuri K, et al. A cost-effectiveness analysis of levodopa/carbidopa intestinal gel compared to standard care in late stage Parkinson’s disease in the UK. J Med Econ. 2011;14(5):584–93.
Lowin J, Sail K, Baj R, et al. The cost-effectiveness of levodopa/carbidopa intestinal gel compared to standard care in advanced Parkinson’s disease. J Med Econ. 2017;20(11):1207–15.
Walter E, Odin P. Cost-effectiveness of continuous subcutaneous apomorphine in the treatment of Parkinson’s disease in the UK and Germany. J Med Econ. 2015;18(2):155–65.
Van Boven JF, Novak A, Driessen M, et al. Economic evaluation of ropinirole prolonged release for treatment of Parkinson’s disease in the Netherlands. Drugs Aging. 2014;31(3):193–201.
Eggington S, Valldeoriola F, Chaudhuri K, et al. The cost-effectiveness of deep brain stimulation in combination with best medical therapy, versus best medical therapy alone, in advanced Parkinson’s disease. J Neurol. 2014;261(1):106–16.
Pietzsch JB, Garner AM, Marks WJ Jr. Cost-effectiveness of deep brain stimulation for advanced Parkinson’s disease in the United States. Neuromodulation. 2016;19(7):689–97.
Hoehn MM, Yahr MD. Parkinsonism: onset, progression and mortality. Neurology. 1967;17(5):427–42.
Worth PF. When the going gets tough: how to select patients with Parkinson’s disease for advanced therapies. Pract Neurol. 2013;13(3):140–52.
Britannia Pharmaceuticals Ltd. APO-go PFS 5mg/ml solution for infusion in pre-filled syringe, summary of product characteristics 2020. https://www.medicines.org.uk/emc/medicine/15992#gref. Accessed 3 Feb 2022.
Leta V, van Wamelen D, Sauerbier A, et al. Opicapone and levodopa-carbidopa intestinal gel infusion: the way forward towards cost savings for healthcare systems? J Parkinsons Dis. 2020;10(4):1535–9.
NHS. England announces annual investment decisions for certain specialised services 2015. 2015. https://www.england.nhs.uk/2015/07/annual-investment- decisions/. Accessed 3 Feb 2022.
NHS England. Clinical commissioning policy: levodopa-carbidopa intestinal gel (LCIG). D04/P/e DuoDopa for Parkinsons disease. 2015. https://www.england.nhs.uk/commissioning/wp-content/uploads/sites/12/2015/07/d04-p-e.pdf. Accessed 3 Feb 2022.
Olanow CW, Kieburtz K, Odin P, et al. Continuous intrajejunal infusion of levodopa-carbidopa intestinal gel for patients with advanced Parkinson’s disease: a randomised, controlled, double-blind, double-dummy study. Lancet Neurol. 2014;13(2):141–9.
Fernandez HH, Boyd J, Fung V, et al. Long-term safety and efficacy of levodopa-carbidopa intestinal gel in advanced Parkinson’s disease. Mov Disord. 2018;33(6):928–36.
Antonini A, Poewe W, Chaudhuri K, et al. Levodopa-carbidopa intestinal gel in advanced Parkinson’s: final results of the GLORIA registry. Parkinsonism Relat Disord. 2017;45:13–20.
Fernandez HH, Standaert D, Hauser R, et al. Levodopa-carbidopa intestinal gel in advanced Parkinson’s disease: final 12-month, open-label results. Mov Disord. 2015;30(4):500–9.
Puente V, Fabregues O, Oliveras C, et al. Eighteen month study of continuous intraduodenal levodopa infusion in patients with advanced Parkinson’s disease: impact on control of fluctuations and quality of life. Parkinsonism Relat Disord. 2010;16(3):218–21.
Santos-García D, Sanjurjo L, Macias M, et al. Long-term exposure to duodenal levodopa/carbidopa infusion therapy improves quality of life in relation especially to mobility, activities of daily living, and emotional well-being. Acta Neurol Scand. 2012;125(3):187–91.
Honig H, Antonini A, Martinez-Martin P, et al. Intrajejunal levodopa infusion in Parkinson’s disease: a pilot multicenter study of effects on nonmotor symptoms and quality of life. Mov Disord. 2009;24(10):1468–74.
Slevin JT, Fernandez H, Zadikoff C, et al. Long-term safety and maintenance of efficacy of levodopa-carbidopa intestinal gel: an open-label extension of the double-blind pivotal study in advanced Parkinson’s disease patients. J Parkinsons Dis. 2015;5:165–74.
De Fabregues O, Dot J, Abu-Suboh M, et al. Long-term safety and effectiveness of levodopa-carbidopa intestinal gel infusion. Brain Behav. 2017;7(8):e00758.
Antonini A, Odin P, Pahwa R, et al. The long-term impact of levodopa/carbidopa intestinal gel on ‘off’-time in patients with advanced Parkinson’s disease: a systematic review. Adv Ther. 2021;38(6):2854–90.
Kristiansen IS, Bingefors K, Nyholm D, et al. Short-term cost and health consequences of duodenal levodopa infusion in advanced Parkinson’s disease in Sweden. Appl Health Econ Health Policy. 2009;7(3):167–80.
NICE Decision Support Unit. Technical support documents. http://nicedsu.org.uk/technical-support-documents/. Accessed 3 Feb 2022.
National Institute for Health and Care Excellence. PMG9: guide to the methods of technology appraisal. 2013. https://www.nice.org.uk/process/pmg9/chapter/foreword. Accessed 15 Dec 2021.
Johnson SJ, Diener M, Kaltenboeck A, et al. An economic model of Parkinson’s disease: implications for slowing progression in the United States. Mov Disord. 2013;28(3):319–26.
Palmer CS, Schmier J, Snyder E, et al. Patient preferences and utilities for ‘off-time’ outcomes in the treatment of Parkinson’s disease. Qual LIfe Res. 2000;9(7):819–27.
Palmer CS, Nuijten M, Schmier J, et al. Cost effectiveness of treatment of Parkinson’s disease with entacapone in the United States. Pharmacoeconomics. 2002;20(9):617–28.
Office for National Statistics. National life tables, UK: 2016 to 2018. 2019. https://www.ons.gov.uk/releases/nationallifetablesuk2016to2018. Accessed 20 Sept 2020.
AbbVie data on file. Adelphi Real-World Parkinson's Disease Specific Programme. 2019.
Anderson P, Benford M, Harris N, et al. Real-world physician and patient behaviour across countries: disease-specific programmes: a means to understand. Curr Med Res Opin. 2008;24(11):3063–72.
Monthly Index of Medical Specialities (MIMS). 2020; http://www.mims.co.uk/. Accessed 3 Feb 2022.
NHS. NHS trusts and NHS foundation trusts. National schedule of reference costs: year 2017-2018. 2018. https://improvement.nhs.uk/resources/reference-costs/. Accessed 3 Feb 2022.
Curtis L, Burns A. Unit costs of health and social care 2018. Project report. Kent: University of Kent; 2018
AbbVie data on file. Adelphi Real-World Parkinson's Disease Specific Programme. 2012.
Dolan P. Modeling valuations for EuroQol health states. Med Care. 1997;35(11):1095–108.
AbbVie. Long-term study of duodopa (levodopa/carbidopa) in advanced Parkinson's: health outcomes & net economic impact (DAPHNE). 2011. https://clinicaltrials.gov/ct2/show/NCT00141518. Accessed 3 Feb 2022.
Antonini A, Yegin A, Preda C, et al. Global long-term study on motor and non-motor symptoms and safety of levodopa-carbidopa intestinal gel in routine care of advanced Parkinson’s disease patients; 12-month interim outcomes. Parkinsonism Relat Disord. 2015;21(3):231–5.
Findley LJ, Wood E, Lowin J, et al. The economic burden of advanced Parkinson’s disease: an analysis of a UK patient dataset. J Med Econ. 2011;14(1):130–9.
Thach A, Jones E, Pappert E, et al. Real-world assessment of “OFF” episode-related healthcare resource utilization among patients with Parkinson’s disease in the United States. J Med Econ. 2021;24(1):540–9.
Shih TM, Sail K, Jalundhwala Y, et al. The effect of functional status impairment on nursing home admission risk among patients with advanced Parkinson’s disease. J Med Econ. 2020;23(3):297–307.
Dahodwala N, Pettit A, Jahnke J, et al. Use of a medication-based algorithm to identify advanced Parkinson’s disease in administrative claims data: associations with claims-based indicators of disease severity. Clin Parkinsonism Relat Disord. 2020;3:100046.
Titova N, Martinez-Martin P, Katunina E, et al. Advanced Parkinson’s or “complex phase” Parkinson’s disease? Re-evaluation is needed J Neural Transm (Vienna). 2017;124(12):1529–37.
Santos-García D, de Deus Fonticoba T, Castro E, et al. 5-2-1 Criteria: a simple screening tool for identifying advanced PD patients who need an optimization of Parkinson’s treatment. Parkinson Dis. 2020;2020:7537924.
Antonini APO, Odin P, Jalundhwala YJ, et al. Assessing the validity and reliability of MANAGE-PD tool to identify patients with Parkinson’s disease inadequately controlled on oral medications: results from an international survey of general neurologists and movement disorder specialists [abstract]. Move Disord. 2019;34(Suppl. 2).
Aldred J, Anca-Herschkovitsch M, Antonini A, et al. Application of the “5-2-1” screening criteria in advanced Parkinson’s disease: interim analysis of DUOGLOBE. Neurodegener Dis Manag. 2020;10(5):309–23.
Härkänen T, Maljanen T, Lindfors O, et al. Confounding and missing data in cost-effectiveness analysis: comparing different methods. Health Econ Rev. 2013;3(1):8.
Kruse C, Kretschmer S, Lipinski A, et al. Resource utilization of patients with Parkinson’s Disease in the late stages of the disease in Germany: data from the CLaSP Study. Pharmacoeconomics. 2021;39:601–15.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was supported and funded by AbbVie Inc. AbbVie participated in the study design, research, data collection, analysis and interpretation of data, writing, reviewing, and approving the publication.
Conflicts of interest/Competing interests
K. Ray Chaudhuri has received educational funding from UCB, and honoraria for sponsored symposiums from UCB, AbbVie, Britannia, US Worldmeds, Otsuka, Medtronic, and Zambon and acted as a consultant for AbbVie, UCB, Britannia, Medtronic and Mundipharma. A. Simon Pickard is a partner in Second City Outcomes Research LLC and Maths in Health BV, and received funds as a paid consultant from AbbVie. Ali Alobaidi, Yash J. Jalundhwala, Prasanna L. Kandukuri, Yanjun Bao, Julia Sus, and Christian Ridley are employees of AbbVie and may own stocks/shares in the company. Glynn Jones was an employee of AbbVie at the time of the study. Julia Oddsdottir and Weiwei Xu are employees of IQVIA, which received funding to conduct the study. Seyavash Najle-Rahim and Matthew Madin-Warburton were employees of IQVIA at the time of the study. Anette Schrag was supported by research funding or support from University College London, National Institute of Health, National Institute for Health Research University College London Hospital Biomedical Research Centre, the International Parkinson and Movement Disorder Society, the European Commission, Parkinson's UK, GE Healthcare, and the Economic and Social Research Council; honoraria for consultancies from Biogen, AbbVie, Roche, BIAL and GE Healthcare; license fee payments from the University College London for the MSA-QoL, PSP-QoL and PQolCarers; and royalties from Oxford University Press.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
The authors confirm that the data supporting the findings of this study are available within the article and/or its supplementary materials.
Code availability
Not applicable.
Authors’ contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Julia Oddsdottir and Prasanna L. Kandukuri. All authors commented on all drafts of the manuscript. All authors read and approved the final version for submission.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Chaudhuri, K.R., Pickard, A.S., Alobaidi, A. et al. The Cost Effectiveness of Levodopa-Carbidopa Intestinal Gel in the Treatment of Advanced Parkinson’s Disease in England. PharmacoEconomics 40, 559–574 (2022). https://doi.org/10.1007/s40273-022-01132-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-022-01132-y