This article is an answer to the Case – Dyspnea and Orthopnea after CABG
Radiologic Findings
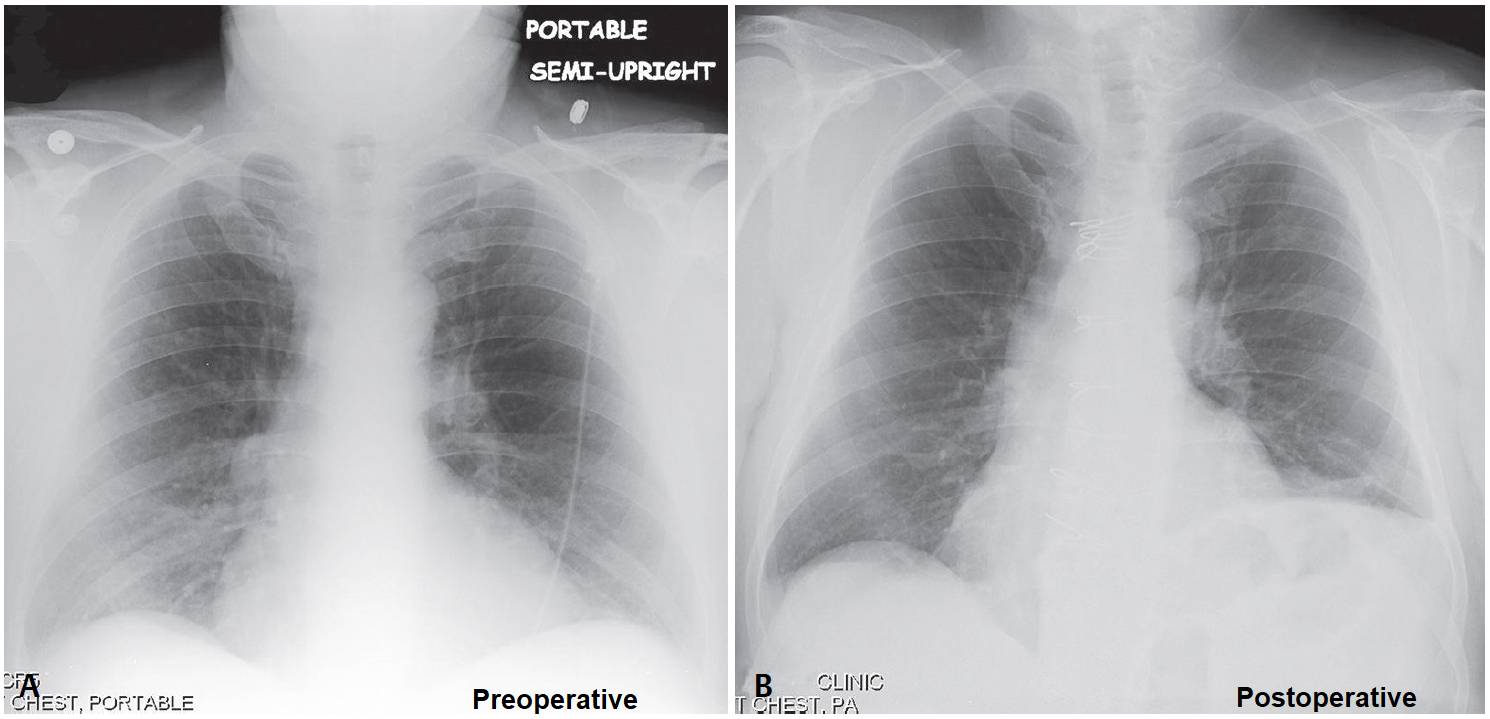
Preoperative frontal chest X-ray shows mild cardiomegaly and a normal relationship of the right and left diaphragms. No underlying lung disease is present.
Follow-up postoperative frontal chest radiograph demonstrate marked elevation of the left diaphragm relative to the right. Note the median sternotomy. Subsequent fluoroscopic “sniff test” revealed paradoxical motion of the left diaphragm.
Diagnosis
Paralyzed Left Diaphragm
Differential Diagnosis
- Eventration of the Diaphragm
- Congenitally thin muscular portion of diaphragm; appearance increases with age
- 5R:1L
- Anteromedial on right; usually involves entire left diaphragm
- Elevation of the Diaphragm
- Subpulmonic Effusion
- Atelectasis
- Hypoplastic Lung
- Abdominal Disease (e.g., subphrenic abscess; liver mass; ascites)
- Idiopathic
- Diaphragmatic Hernia
Etiology of Diaphragmatic Paralysis
Unilateral diaphragmatic paralysis is most often the result of neoplasia (e.g., lymphoma, advanced lung cancer). Other possible causes include non-iatrogenic and iatrogenic trauma, cervical spondylosis, herpes zoster infection, and infrequently sepsis.
Bilateral diaphragmatic paralysis is usually a sequela of motor neuron disease (e.g., amyotrophic lateral sclerosis), demyelinating disease (e.g., multiple sclerosis), and myopathies (e.g., muscular dystrophy).
The incidence of diaphragmatic paresis-paralysis after coronary artery bypass grafting (CABG) ranges from 10% to 60%. Postulated causes include pleurotomy with harvest of the internal mammary artery for grafts (e.g., chest wall and parenchymal trauma, reduced blood flow to ipsilateral intercostal muscles), mechanical injury to the phrenic nerve (i.e., phrenic nerves crosses the internal mammary artery anteriorly (54% of patients) and posteriorly (14% of patients), and the use of cardioplegic solutions.
Clinical Findings
Symptoms depend on whether the diaphragmatic paralysis is unilateral or bilateral, and on the presence of pre-existent lung disease. Patients with unilateral diaphragmatic paralysis are often asymptomatic at rest but experience dyspnea with exertion, or dyspnea at rest if they have underlying pre-existent lung disease (e.g., emphysema, pulmonary fibrosis).
Patients with bilateral diaphragmatic paralysis may present with respiratory failure or dyspnea exacerbated by recumbency. Paradoxical abdominal wall retraction during inspiration may be observed. On PFTs, vital capacity (VC) normally decreases approximately 10% with recumbency.
In unilateral diaphragmatic paralysis the VC decreases to 20–30% or more of the predicted value, and with bilateral diaphragmatic paralysis there is a 50% decrease in VC. Diaphragmatic electromyography (EMG) has a limited role in unilateral diaphragmatic paralysis but may reveal a pattern consistent with underlying myopathy or neuropathy.
Assessment of transdiaphragmatic pressure differentials (i.e., thin-walled balloon placed transnasally into the distal esophagus to measure pleural pressure changes and a second intra-gastric balloon placed to measure intra-abdominal pressure) can distinguish diaphragmatic paralysis from other causes of respiratory failure.
Imaging Findings
Chest Radiography
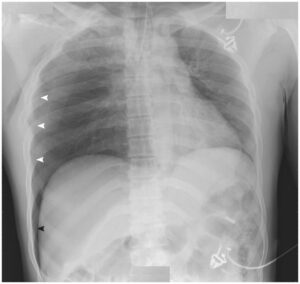
Unilateral Diaphragmatic Paralysis
- Unilateral diaphragmatic elevation strongly suggests diagnosis
- Comparison with serial or remote chest exams helpful in documenting chronicity
- Lung volume diminished on affected side
- Ipsilateral basilar atelectatic changes
Bilateral Diaphragmatic Paralysis
- Often unrecognized or misinterpreted as low lung volumes or hypoventilation
Fluoroscopic “Sniff Test”
- Real-time fluoroscopic study performed to assess diaphragmatic excursion during tidal volume (normal inspiration and expiration) and with exaggerated inspiratory maneuvers designed to isolate diaphragm from accessory respiratory muscles (i.e., through rapid sniffing)
- During inspiration and expiration, normal diaphragm moves down and up, respectively, 2–8 cm
- Rapid repetitive “sniffing” (i.e., as if the patient has a bad runny nose without the benefit of a handkerchief or tissue)
- Accentuates the difference in a paretic or paralyzed diaphragm, which will exhibit paradoxical motion (i.e., during inspiration, affected diaphragm moves up; and during expiration, affected diaphragm moves down)
- Must be performed with patient supine or at least semi-recumbent; upright positioning alone has a high false negative rate
Ultrasonography
- Paretic-paralyzed diaphragm exhibits no active caudal excursion with inspiration
- Paradoxical movement with employment of rapid sniffing
MDCT
- Indicated in patients with suspected neoplasia or lymphadenopathy affecting or invading the phrenic nerve
Management
- Most patients: asymptomatic, transient; do not require treatment
- Surgical diaphragmatic plication may benefit symptomatic patients with unilateral diaphragmatic paralysis
- Bilateral diaphragmatic paralysis depends on the etiology and severity
- Phrenic nerves intact without myopathy: diaphragmatic pacing (phrenic nerve is electrically stimulated to contract the diaphragm)
- Phrenic nerves not intact: non-invasive positive-pressure ventilation
Prognosis
- Good in unilateral diaphragmatic paralysis, especially in the absence of underlying neurologic or pulmonary disease
- Poor in patients with advanced lung disease, bilateral diaphragmatic paralysis, and chronic demyelinating conditions
- Most patients with post–cardiac surgery diaphragmatic paresis-paralysis improve with conservative measures; rarely complicated by hypoventilatory respiratory failure
- Diaphragm function may recover if nerve is not permanently injured; phrenic nerve regeneration occurs at an estimated rate of 1 mm/day
- Bilateral diaphragmatic paralysis: may be complicated by increased CO2 retention, leading to eventual hypercapnic respiratory failure
Pearls
- “Sniff test”—insensitive with ipsilateral large or subpulmonic pleural effusions.
- Diaphragmatic excursion is paradoxical with diaphragmatic paralysis but not with diaphragmatic eventration.
References
- Gierada DS, Slone RM, Fleishman MJ. Imaging evaluation of the diaphragm. Chest Surg Clin N Am 1998;8(2): 237–280
- Kumar N, Folger WN, Bolton CF. Dyspnea as the predominant manifestation of bilateral phrenic neuropathy. Mayo Clin Proc 2004;79(12):1563–1565
- Qureshi A. Diaphragm paralysis. Semin Respir Crit Care Med 2009;30(3):315–320
- Ulkü R, Onat S, Balci A, Eren N. Phrenic nerve injury after blunt trauma. Int Surg 2005;90(2):93–95
- Verhey PT, Gosselin MV, Primack SL, Kraemer AC. Differentiating diaphragmatic paralysis and eventration. Acad Radiol 2007;14(4):420–425