Click here to proceed to your no-fee CE(CME) credit for this activity. To receive credit, you will need to log-in/register with Evolve Medical Education.
Trigeminal dysphoria is a term that describes the constellation of symptoms commonly experienced by many patients. These symptoms are exacerbated following prolonged use of digital devices after long periods of reading or other close work. The symptoms of trigeminal dysphoria include headaches, eyestrain, dry eye sensation, neck, and shoulder pain.1 New research suggests that Computer Vision Syndrome, also called Digital Eye Strain, is a form of visually induced trigeminal dysphoria.2,3,4 While this is a relatively new term, the problems associated with it are not new and have been documented since the 1800s as asthenopia, convergence insufficiency, and fixation disparity, among others.
This continuing education activity explains the mechanism of why patients with trigeminal dysphoria are symptomatic and what to do to resolve their symptoms. We discuss the huge rise in digital devices over the past few years and how this digitally evolving environment has such an impact on our vision. We also review the research happening between neurology and optometry.
I come from a long line of eye care providers, and never did I think as an optometrist that I'd be involved with neurology. However, I believe we will continue to coexist with that field to solve patients' headaches and related problems.
-Jeffrey P. Krall, OD
1. Digre KB. More than meets the eye: The eye and migraine—what you need to know. J Neuro-Ophthalmol. 2018; 38: 237-243.
2. Ackerman R, Krall J, Vance Thompson V, et al. A new treatment for computer vision syndrome. eyeBrain Medical Inc. Data on File.
3. Karpecki PM. The dry eye misalignment. Review of Optometry. Updated Aug. 15, 2018. Accessed May 20, 1019.
4. Thompson V. Eye pain and strain that masquerade as dry eye. Cataract & Refractive Surgery Today. February 2019. Accessed May 20, 2019.
I’m a general neurologist, but about 80% of my practice consists of patients with headache. When I initially met with Jeffrey Krall, OD, I was at a point where I was running through all my tools, and I was still struggling with this group of headache patients whose symptoms I couldn’t resolve.
These patients had been through the gamut of recommended medications for treatment of migraine1 and were still symptomatic. We were out of options, which is very frustrating for a practitioner. This is what led us to undertake the Chronic Daily Headache Study in 2013.
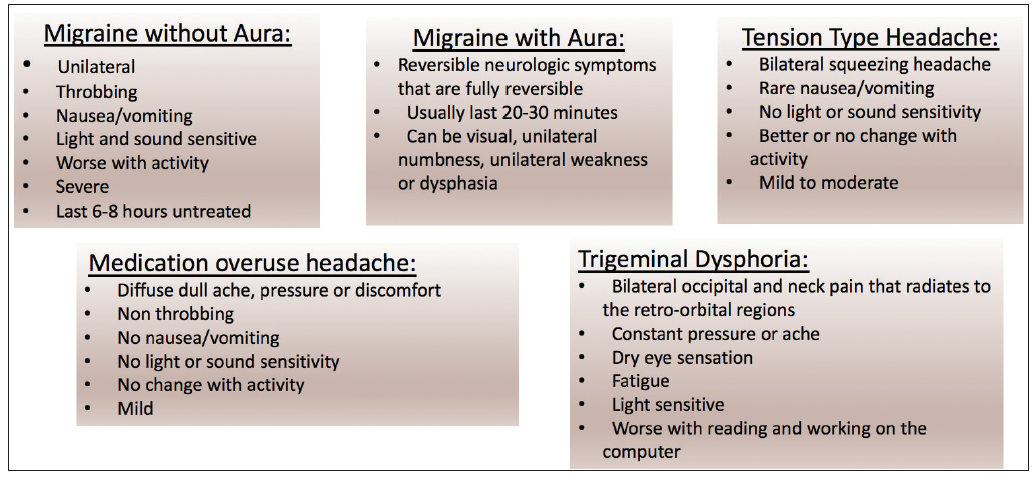
TYPES OF HEADACHES
There are several types of headaches (Figure 1). The patients enrolled in the study were experiencing migraine-type headaches. Migraines (without aura) tend to be one-sided, cause throbbing, nausea, vomiting, light and sound sensitivity, and become worse with activity.2
Only about 20% of patients have migraine with aura and those headaches are generally reversible in about 20 to 30 minutes, even though they can last up to a couple of hours. These patients can have numbness or tingling on one side of their body. In rare cases, patients can have weakness or one-sided paralysis.2
Tension headaches are common and most of your patients have likely described that kind of “squeezing all over” headache. They tend not to be as severe and do not include nausea or sensitivity to light or sound.2
Medication overuse headaches can occur in patients who use any sort of pain medication, whether it’s acetaminophen, morphine or anything in between. Patients who use those more than 3 days a week can develop medication overuse headaches, which I used to diagnose frequently in my patients before we conducted the trigeminal nerve study. There’s a great deal of crossover in how patients feel with medication overuse headaches and trigeminal dysphoria. It’s a dull, nondescript headache, without nausea or sound sensitivity.2,3
Trigeminal dysphoria is a term that describes the constellation of symptoms commonly experienced by patients following the prolonged use of digital devices or after long periods of reading or other close work. It typically produces a dull type of an ache. I’ve seen patients describe the pain as coming from the front to the back and from the back to the front. They tend to have significant neck pain and feeling of dry eyes. These patients become fatigued when they’re reading and working on the computer and are typically light sensitive. In contrast to a migraine headache (light sensitive during the headache), patients with trigeminal dysphoria tend to be light sensitive all the time. They don’t like the sunlight or bright headlights at night. They tend to turn down the brightness on their computer and cell phone screens.2,3,4
THE TRIGEMINAL NERVE FUNCTION
The trigeminal nerve is the fifth cranial nerve. Its primary function is to provide sensory and motor innervation to the face. The three sensory branches of the trigeminal nerve emanate from the ganglia to form the three branches of the trigeminal nerve. The different branches are namely the ophthalmic (V1), maxillary (V2), and mandibular (V3) nerves (Figure 2).3,5
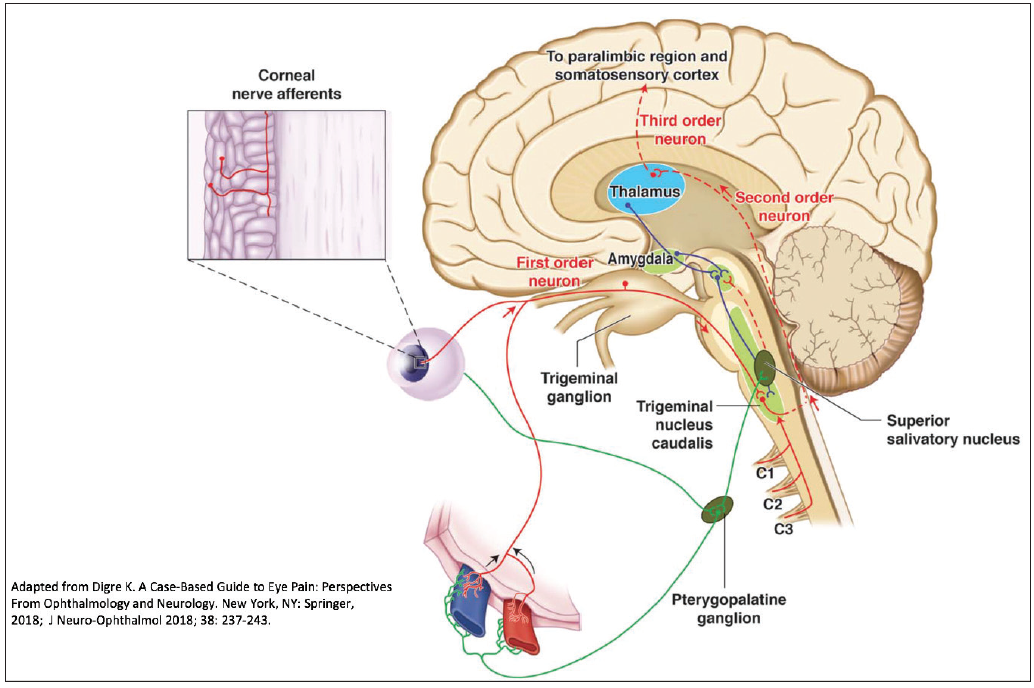
Figure 2. The pathophysiology of migraine as a sensory processing disorder receives peripheral pain input from the dura and from the ocular sensory system—both by way of the first division of the trigeminal nerve.
The ophthalmic branch of the trigeminal nerve sets the bar for the irritability of the trigeminal nerve. It can become irritated by many common triggers: too much caffeine, too little caffeine, excess alcohol consumption, weather change, hormonal change, sleep schedule change, not eating on time, etc.3
With migraine headaches, we believe the nerve is simply too sensitive in some individuals.3 We don’t know why, possibly genetic. This variance in nerve levels is likely genetic, which explains why some people can get them and other people do not.2,3
The trigeminal nucleus caudalis is the longest nucleus in the brainstem. It goes through the brainstem and into the cervical spine at the C1 and C2 vertebrae, which is partly why patients with migraines and with trigeminal dysphoria have neck pain.6 We believe the entire trigeminal nucleus caudalis becomes irritated and overstimulated. As this irritation continues, it can affect the entire brain, which is called central sensitization. That’s when a patient has difficulty concentrating, plus nausea, vomiting, light and sound sensitivity, etc.2,6
Also worth noting is that that the trigeminal nerve innervates both the cornea and the meninges, which is the source of migraine pain. There are no pain receptors located in the brain, so the pain is generated from the meninges.6 When reading, our eyes must constantly transfer images from our peripheral tracking system to our central vision. If there’s an imbalance between these two systems, the extraocular muscles are forced to make constant binocular readjustments of eye position, which lead to overstimulation and nerve irritation that results in painful impulses that are transmitted to the eyes, head, and neck.2,3,6
RELIEF FOR PATIENTS
With the research conducted at our headache center, plus the work by Dr. Krall and others, we believe we have found a solution to this problem of overworking the brain and overstimulating the trigeminal nerve, which causes eye fatigue, neck pain, light sensitivity, etc., that occurs after prolonged close work and especially after extended use of digital devices. Contoured prism lenses compensate for the eye misalignment and relieve these symptoms.4,7,8
To help patients understand the technology, I begin by explaining that he or she has a misalignment between their eyes and the central and peripheral vision. There’s quite a large area that has to be compensated for between where your eyes want to focus and where they actually do focus. If one eye is open, you can see an image. If the other eye is open, you can see an image. But when both eyes are open, they must be perfectly aligned. If they’re not, like when watching a 3D movie without the 3D glasses, the brain doesn’t like that, so it tries to keep those images in focus together (Figure 3). Because the proprioceptive fibers are in the first branch of the cranial nerve fiber, the trigeminal nerve, it’s constantly overstimulating that nerve, which likely stimulates the headache pain.6 This occurs especially when looking at digital devices including computer screens, tablets and smart phones.4,9
This overstimulation worsens severe headaches, but it likely triggers trigeminal dysphoria. Therefore, we suggest the best way to prevent trigeminal dysphoria is to keep the nerve calm by ensuring those images are perfectly aligned instead of the brain trying to keep those together through the proprioception. We have found that using contoured prism technology can help keep the nerve calm in certain patients.4,7,8
1. Loder E, Burch R, Rizzoli P. The 2012 AHS/AAN Guidelines for prevention of episodic migraine: A summary and comparison with other recent clinical practice guidelines. Headache. 2012;52:930-945.
2. Rizzoli P, Mullally WJ. Headache. Am J Med. 2018;131, 17–24.
3. Digre KB. More than meets the eye: the eye and migraine—what you need to know. J Neuro-Ophthalmol. 2018; 38: 237-243.
4. Ackerman R, Krall J, Vance Thompson V, et al. A new treatment for computer vision syndrome. eyeBrain Medical Inc. Data on File.
5. Huff T, Daly DT. Neuroanatomy, cranial nerve 5 (Trigeminal). StatPearls [Internet]. Last Update: April 8, 2019. Accessed May 15, 2019. https://www.ncbi.nlm.nih.gov/books/NBK482283/.
6. Weir C. Proprioception in extraocular muscles. J Neuro-Ophthalmol. 2006;26:123-127.
7. del Mar Segui M. A reliable and valid questionnaire was developed to measure computer vision syndrome at the workplace. J Clin Epidemiology. 2015;68: 662-673.
8. Teitelbaum B, Pang Y, Krall J. Effectiveness of base in prism for presbyopes with convergence insufficiency. Optom Vis Sci. 2009;86(2):153-156.
9. Thompson V. Eye pain and strain that masquerade as dry eye. Cataract & Refractive Surgery Today. February 2019. Accessed May 20, 2019.