A 49-year-old woman was involved in a motor vehicle accident, during which the front airbag deployed. She had been wearing contact lenses at the time and developed corneal inflammation in the right eye as a result of the trauma. The woman was under the care of another eye care provider who had previously treated her for herpes simplex keratitis without resolution. She was eventually referred to our tertiary care clinic for evaluation of a persistent corneal ulcer.
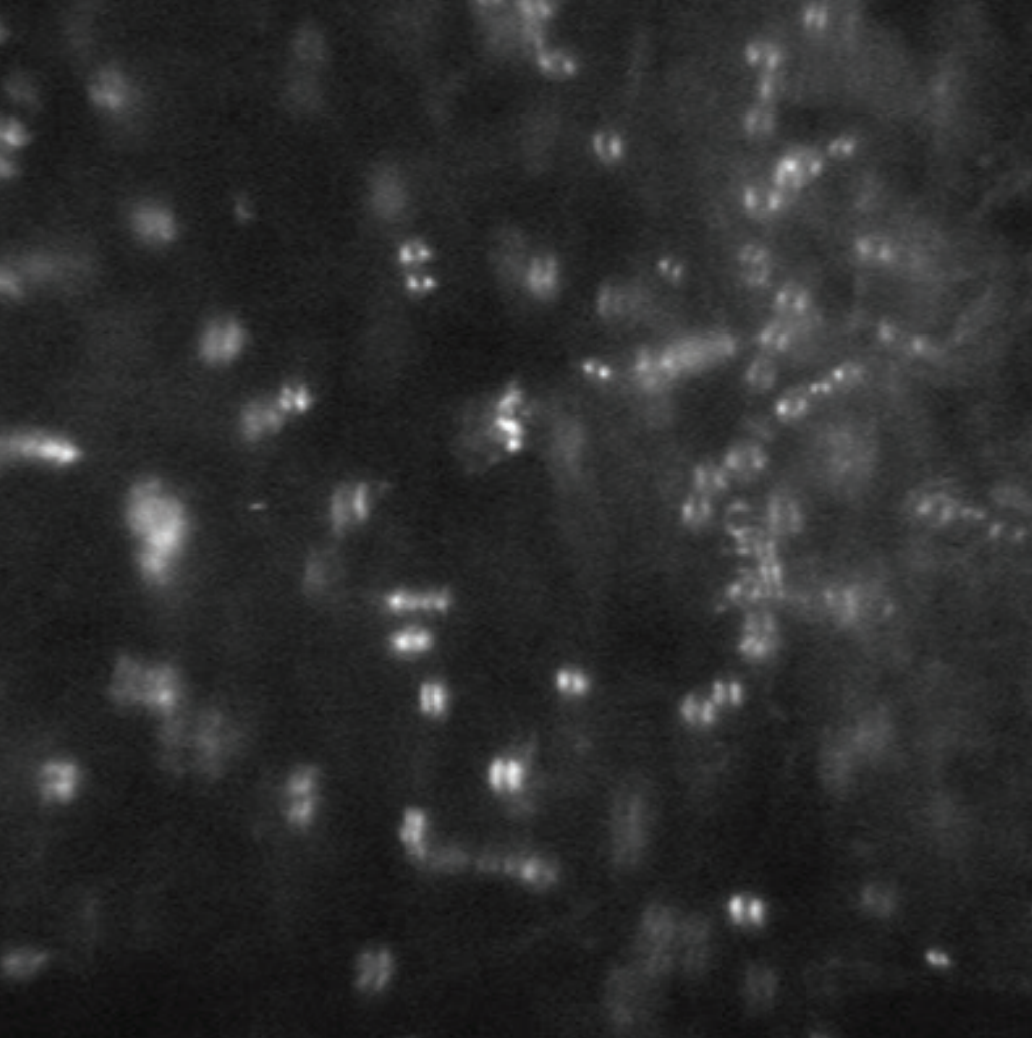
At her initial visit, there was a large corneal epithelial defect from a corneal scrape the day prior and modest stromal haze with a faint infiltrate. Due to her high pain level, she underwent confocal imaging (Inset), which revealed double-walled cysts consistent with Acanthamoeba keratitis. The patient was started on polyhexamethylene biguamide and chlorhexidine, maintained on a prophylactic topical antibiotic, and referred to a cornea specialist for further management.
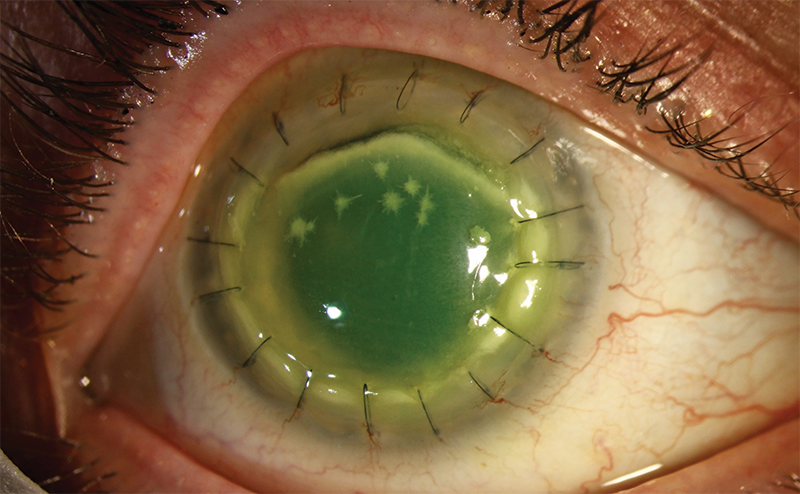
In the following months, the disease burden lessened but left corneal scarring. The patient underwent penetrating keratoplasty and received antiamoebic therapy, prophylactic antibiotics, and topical corticosteroids to prevent rejection. Unfortunately, she developed crystal-like whitish deposits and infiltration of the graft shortly thereafter (Main Figure). Repeat confocal imaging revealed the return of double-walled cysts. Given the crystalline deposits, there was also concern for a secondary microbial infection despite the generally white and quiet appearance of the eye.
Infectious crystalline keratopathy (ICK) is a rare clinical entity in which fern-like or needle-like whitish deposits can be seen in the anterior or middle stroma.1 These crystalline infiltrates are often indolent, meaning they are not associated with significant inflammation. Histopathology has shown that the causative microorganisms typically reside within interlamellar stromal spaces and often form a protective biofilm. This makes them more difficult to culture and treat effectively.
Risk factors for ICK include prior corneal surgery (most often penetrating keratoplasty) and local immunosuppression such as corticosteroid eye drops. ICK has also been described in herpes simplex or Acanthamoeba infection, anesthetic abuse, contact lens use, and history of LASIK surgery. In cases associated with Acanthamoeba, cultures or biopsies sometimes identify additional bacterial pathogens, suggesting a symbiotic relationship.2
Treatment is often challenging and should be undertaken by a cornea specialist, given the frequent need for surgical intervention, the complex disease course, and the often poor prognosis.
- 1. Porter AJ, Lee GA, Jun AS. Infectious crystalline keratopathy. Surv Ophthalmol. 2018;63(4):480-499.
- 2. Tu EY, Joslin CE, Nijm LM, Feder RS, Jain S, Shoff ME. Polymicrobial keratitis: Acanthamoeba and infectious crystalline keratopathy. Am J Ophthalmol. 2009;148(1):13-19.e2.