At A Glance
- Current at-home methods of treating MGD are limited in their effectiveness and lead to unsatisfactory outcomes.
- Two new in-office treatment modalities, intense pulsed light and thermal pulsation, better address MGD especially when combined and provide patients with more effective relief.
- With a customized treatment plan and proper patient education in place, we can improve tear film quality and slow the worsening of MGD over time.
Meibomian gland dysfunction (MGD) is the most common cause of dry eye disease (DED) and is one of the most common disorders encountered at an eye clinic, affecting up to 70% of the general population.1 Current methods of treating MGD involve heat in the form of warm compresses, self-administered lid massage, and manual expression. However, these conventional treatment methods remain limited in their effectiveness and, therefore, result in unsatisfactory outcomes.2 Recently, in-office treatment modalities have emerged that better address this complex disorder and provide our patients with more effective relief. These modalities include intense pulsed light (IPL) and thermal pulsation (Figure 1).

Figure 1. Dr. Kataria performing thermal pulsation using LipiFlow (A) and Dr. Madan performing IPL (B).
THE NEW CONTENDERS
The current body of evidence suggests that IPL and thermal pulsation, separately, can each result in decreased dry eye symptoms, improved meibomian gland function, reduced inflammation, and increased tear break-up time. Both treatments are included in the Tear Film & Ocular Surface Society (TFOS) Dry Eye Workshop II (DEWS II) Report as viable treatment options for MGD.3 However, there is increasing evidence in the literature and in clinical settings that IPL and thermal pulsation can more effectively improve MGD when combined, compared with either treatment alone. This article will examine how these two treatment modalities fit into our current dry eye treatment algorithm and when to use one or both.
How Does IPL Work?
IPL delivers nonlaser light therapy that increases the temperature of the eyelid, promotes secretion of meibum from the meibomian glands, ablates Demodex, and interrupts the inflammatory cascade that contributes to MGD. When the root cause of MGD is identified as inflammation, IPL can be an especially powerful tool to help treat this condition. IPL closes off abnormal telangiectatic vessels along the lid margins, which leak proinflammatory mediators and potentiate inflammation.
Studies have also confirmed that IPL treatments can improve meibomian gland macrostructure and microstructure, observed on confocal microscopy, which leads to overall improvement in gland function.4 Furthermore, various studies have shown that IPL can improve the composition of tear proteins and lipids by decreasing inflammatory interleukins in tears, IL-17A and IL-6, as well as matrix metalloproteinase-9. It also improves the osmolarity of tears.1,5 Compared with routine eyelid hygiene for MGD, IPL treatment is more time-efficient and has better efficacy, lasting more than 6 months.2
How Does Thermal Pulsation Work?
Although treating ocular surface inflammation is important, clearing the obstructed meibum in the meibomian glands is also crucial to the success of DED treatment. This is where thermal pulsation comes in. Thermal pulsation combines sustained heat and pressure to physically melt and evacuate meibum from the meibomian glands.
Interestingly, Blackie et al found that one treatment with the TearScience LipiFlow Thermal Pulsation System (Johnson & Johnson Vision Care) is just as efficacious as applying warm compresses twice per day for 3 months; moreover, the results from using the LipiFlow system have been found to be sustained for up to 1 year.7 The TearCare System (Sight Sciences) and the Systane iLux MGD Thermal Pulsation System (Alcon) are two noninferior alternatives to LipiFlow.8,9 Evacuating the meibomian glands decreases a patient’s risk for atrophy and dropout, and studies support that thermal pulsation is gentle and more effective than manual meibomian gland expression. It carries no risk for scarring the meibomian glands and is more comfortable for patients.2 The treatment is generally well tolerated, and unlike IPL, thermal pulsation often does not need to be repeated several times before results are evident.
HEAT OR LIGHT?
We find that patients who exhibit signs of facial or ocular rosacea benefit more from IPL than thermal pulsation because IPL’s multiple mechanisms of action interrupt the vicious inflammatory cycle by coagulating the abnormal vasculature and reducing the overall inflammatory load.10 Patients who have significant eyelid telangiectasias or Demodex infestation in the absence of rosacea also benefit more from IPL treatments (Figure 2). In recent years, IPL has also been used to treat chalazia.
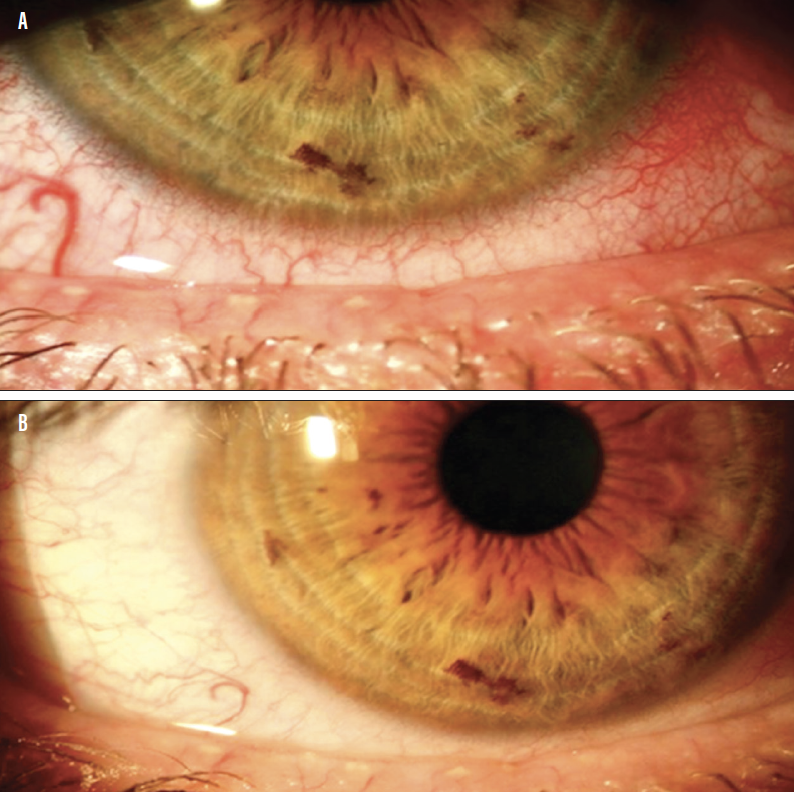
Figure 2. This patient underwent four treatments with IPL, followed by one thermal pulsation treatment with iLux 3 months later. Notice the improvement in eyelid telangiectasias and conjunctival hyperemia posttreatment. Before (A) and after treatment (B).
However, IPL is still not for everyone. It is important to note that IPL can only be performed on individuals with Fitzpatrick skin types I to IV; therefore, it is not suitable for those with darker skin tones. Furthermore, IPL cannot be prescribed to patients who are taking photosensitive medications and/or those with certain skin or autoimmune conditions.
Thermal pulsation, on the other hand, is indicated when there is meibum stasis or risk of meibomian gland atrophy. Thermal pulsation can be performed on a wide variety of patients, depending on the device used. For example, although IPL is not indicated in darker skin tones, thermal pulsation is an effective alternative for treating MGD. IPL or thermal pulsation can also be good options for patients who are looking for natural, non-pharmocotherapy treatments, or who have compliance and dexterity issues that can limit the use of eye drops or at-home care. When needed, both treatment modalities can easily be combined with pharmacology and home-based treatments in a multimodality approach to treating DED.
WHEN TO COMBINE TREATMENTS
Each treatment provides unique advantages, and different approaches can be used synergistically to address multiple components of a patient’s disease state. For example, thermal pulsation does not address telangiectasias, which contribute to inflammation, but IPL does; conversely, IPL does not directly address meibomian gland evacuation, whereas thermal pulsation can (Figure 3).2
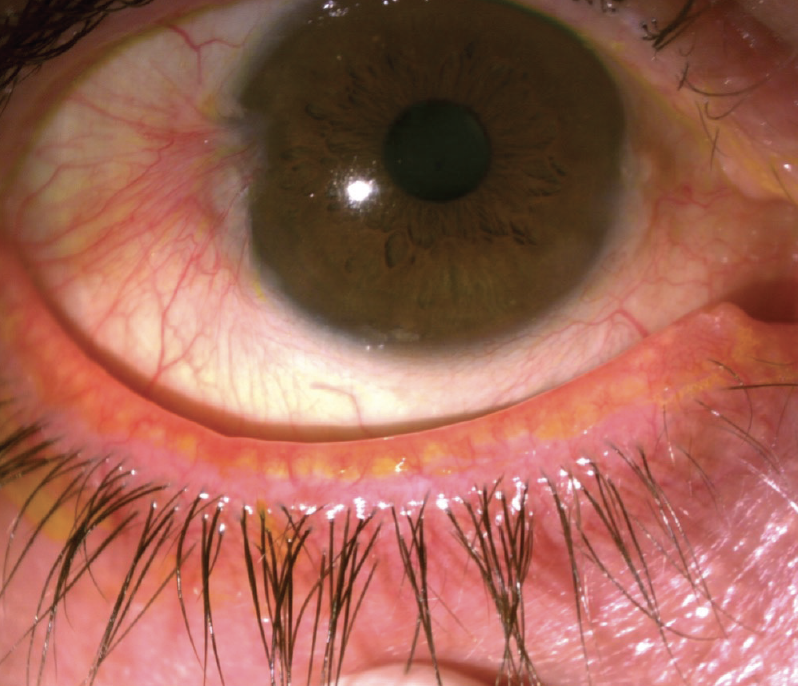
Figure 3. Indications for combining IPL and thermal pulsation treatment include clogged meibomian glands and eyelid telangiectasias, as shown here.
The current literature also supports the synergistic effects of IPL and manual meibomian gland expression in combination. Studies that combine manual gland expression with IPL report improvement in MGD, DED symptoms, corneal staining, tear osmolarity, and TBUT; these results can be maintained up to 6 months.11-14 We can conclude that because thermal pulsation is superior to manual gland expression, combining IPL and thermal pulsation will produce even better therapeutic results. In fact, in our own clinical experience, combining IPL with thermal pulsation yields greater symptom relief for a longer period.
TREATMENT PROTOCOL
There is no cookie cutter approach for treating a disease as complex as MGD. If a patient is a candidate for both IPL and thermal pulsation, we will usually start with a series of four IPL treatments spaced 2 to 4 weeks apart, and then perform thermal pulsation after the last IPL. Following this typical course of treatment, some advanced cases may require further treatments, such as additional IPL sessions in patients with severe eyelid inflammation.
Follow-up is required to monitor for repeat treatments, and these schedules will vary based on disease severity. In general, however, follow-up schedules for these treatments do not differ between combined therapies and monotherapy. Ideally, we perform thermal pulsation every 12 months and maintenance IPL (single treatment) every 6 to 12 months.
OBSTACLES AND OPPORTUNITIES
In-office treatments are expensive and often not covered by insurance, making them financially inaccessible to many patients. Offering multiple in-office treatment options increases the cost to the practitioner due to the initial investment and staff training required. However, with evidence supporting the effectiveness of combining treatments, we can elevate our dry eye practices to best help our patients and improve their quality of life.
With a customized treatment plan in place and transparent education of patients on the need for ongoing maintenance of care, we can effectively improve tear film quality and slow the worsening of MGD over time. We look forward to future studies on the long-term effects of combining in-office heat and light treatments.
- 1. Schaumberg DA, Nichols JJ, Papas EB, Tong L, Uchino M, Nichols KK. The international workshop on meibomian gland dysfunction: report of the subcommittee on the epidemiology of, and associated risk factors for, MGD. Invest Ophthalmol Vis Sci. 2011;52(4):1994-2005.
- 2. Suwal A, Hao JL, Zhou DD, Liu XF, Suwal R, Lu CW. Use of intense pulsed light to mitigate meibomian gland dysfunction for dry eye disease. Int J Med Sci. 2020;17(10):1385-1392.
- 3. Jones L, Downie LE, Korb D, et al. TFOS DEWS II management and therapy report. Ocul Surf. 2017;15(3):575-628.
- 4. Yin Y, Liu N, Gong L, Song N. Changes in the meibomian gland after exposure to intense pulsed light in meibomian gland dysfunction (MGD) patients. Curr Eye Res. 2018;48(3):308-313.
- 5. Liu R, Rong B, Tu P, et al. Analysis of cytokine levels in tears and clinical correlations after intense pulsed light treating meibomian gland dysfunction. Am J Ophthalmol. 2017;183:81-90.
- 6. Blackie CA, Solomon JD, Greiner JV, et al. Inner eyelid surface temperature as a function of warm compress methodology. Optom Vis Sci. 2008;85(8):675-683.
- 7. Blackie CA, Coleman CA, Holland EJ. The sustained effect (12 months) of a single-dose vectored thermal pulsation procedure for meibomian gland dysfunction and evaporative dry eye. Clin Ophthalmol. 2016;10:1385-1396.
- 8. Sight Sciences presents additional results of OLYMPIA study of signs and symptoms of dry eye disease using TearCare [press release]. Sight Sciences. September 9, 2020. https://eyewire.news/news/sight-sciences-presents-additional-results-of-olympia-study-of-signs-and-symptoms-of-dry-eye-disease-using-tearcare
- 9. Tauber J, Owen J, Bloomenstein M, et al. Comparison of the iLUX and the LipiFlow for the treatment of meibomian gland dysfunction and symptoms: a randomized clinical trial. Clin Ophthalmol. 2020;14:405-418.
- 10. Kassir R, Kolluru A, Kassir M. Intense pulsed light for the treatment of rosacea and telangiectasias. J Cosmet Laser Ther. 2011;13(5):216-222.
- 11. Shin KY, Lim DH, Moon CH, et al. Intense pulsed light plus meibomian gland expression versus intense pulsed light alone for meibomian gland dysfunction: a randomized crossover study. PLoS One. 2021;16(3):e0246245.
- 12. Dell SJ, Gaster RN, Barbarino SC, Cunningham DN. Prospective evaluation of intense pulsed light and meibomian gland expression efficacy on relieving signs and symptoms of dry eye disease due to meibomian gland dysfunction. Clin Ophthalmol. 2017;11:817-827.
- 13. Rong B, Tang Y, Tu P, et al. Intense pulsed light applied directly on eyelids combined with meibomian gland expression to treat meibomian gland dysfunction. Photomed Laser Surg. 2018;36(6):326-332.
- 14. Rong B, Tang Y, Liu R, et al. Long-term effects of intense pulsed light combined with meibomian gland expression in the treatment of meibomian gland dysfunction. Photomed Laser Surg. 2018;36(10):562-567.


