Coming to Grips with Plantar Fasciitis

One of the major causes of chronic heel pain, plantar fasciitis is a common foot condition that is typically associated with sporting activities. While it is undeniably painful, it is eminently treatable. Dr Gowreeson Thevendran, Consultant Orthopaedic Surgeon, Island Orthopaedics, explains why.
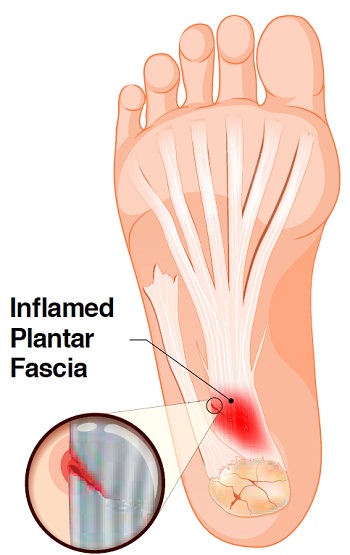
WHAT IS PLANTAR FASCIITIS?
The plantar fascia is a band of deep tissue that runs from your heel bone to your toes. It supports the arch of your foot and also acts as a shock absorber. A tear or injury to this tissue caused by overuse or repetitive loading may trigger inflammation, resulting in the condition known as plantar fasciitis.
Plantar fasciitis is usually associated with frequent and long distance running, jumping exercises or high- ntensity interval training. It causes a severe stabbing pain in the bottom of the foot beside the heel.
“It is estimated that about 10 percent of people will have this condition at some point in their life,” said Dr Gowreeson.
WHAT ARE ITS SYMPTOMS?
The symptoms associated with plantar fasciitis usually involve the sole. Pain is typically felt around the heel, though some pain may be felt in the middle of the foot. The pain intensifies over time. It usually affects only one foot though it can sometimes affect both feet simultaneously.
Symptoms typically include:
• a dull, sharp or burning pain at the bottom at the heel
• severe pain in the heel and tenderness at the sole of the foot
• difficulty walking, especially on rising from bed or after sitting or lying down for a prolonged period of time
• intensified pain after stress on the plantar fascia ligament
Pain is usually felt not during but just after exercising, when the soft tissues start to tighten up.
WHAT CAUSES PLANTAR FASCIITIS?
The cause of this ailment is not entirely clear. However, being overweight is a risk factor, since excess weight puts massive pressure on the plantar fascia ligaments and impedes healing. During late pregnancy, pregnant women are more prone to plantar fasciitis due to the added weight they are carrying.
For obvious reasons, endurance runners are at a higher-than-normal risk of developing plantar fasciitis, as are people whose jobs require them to stand for long periods of time. People between the ages of 40 and 70 are also at higher risk, with women more likely to be affected than men. This may be due to hormonal differences between the genders.
People with flatfoot syndrome typically have tight plantar fascial bands which are more likely to tear or get inflamed. Hence plantar fasciitis patients with flatfeet are advised to wear customised orthotics with a supportive arch to reduce the likelihood of a recurrence.
HOW IS IT TREATED?
Dr Gowreeson has this message of hope for people living with plantar fasciitis: “Plantar fasciitis is not a lifelong sentence. The pains will disappear, and you will get to enjoy a pain-free lifestyle as soon as your treatment begins.”
He emphasised that plantar fasciitis is a self-limiting condition, which usually heals within a time range of 6 to 18 months without treatment. However, the suffering can be significantly minimised with treatment.
“You can gain up to 90 percent recovery within six months of consistent non-operative treatment,” advised Dr Gowreeson.
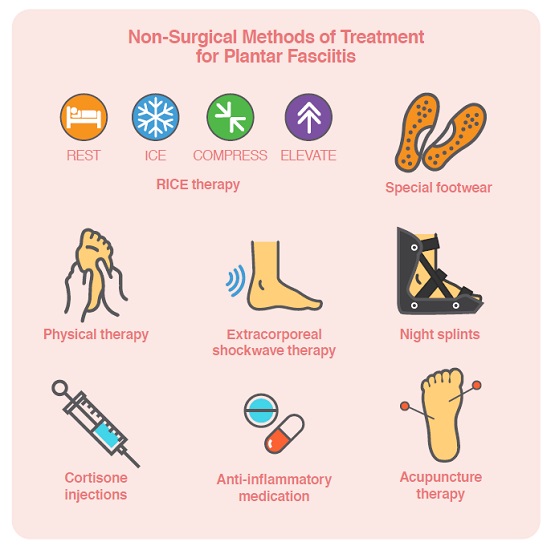
First-time sufferers of plantar fasciitis are typically advised to follow the 4-step ‘RICE’ method of rest, ice, compression and elevation. For repeat cases, special supportive footwear, shoe inserts or customised orthotics are often prescribed, sometimes with night splints or braces that are worn overnight to stretch the plantar fascia and Achilles tendon. Medication, physical therapy and Extracorporeal Shockwave Therapy (EST) are also used to treat very painful or chronic cases.
SURGICAL TREATMENT
Dr Gowreeson shared that 3 to 5 percent of all patients may end up requiring surgery, usually after prolonged and failed conservative therapy and worsening symptoms. Surgery helps to reverse the underlying biomechanical problem – the tight calf muscles and the tight plantar fascia.
“Surgical release can be done through small keyholes and the patient is walking from Day 1 with a supportive sandal,” shared Dr Gowreeson. “There is usually significant relief within the first four weeks even in this recalcitrant group of patients.
MOVING FORWARD, PAIN-FREE
You heard it from Dr Gowreeson – plantar fasciitis can be successfully treated, with surgery as a last resort for a handful of patients. If you suspect that you may be experiencing the painful symptoms of this common condition, seek treatment, reclaim your quality of life, and move on.
Article contributed by Dr Gowreeson Thevendran, an accredited doctor of Mount Alvernia Hospital.
Consultant Orthopaedic Surgeon
Island Orthopaedics
Mount Alvernia Hospital Medical Centre A #01-01/02
Tel: 6356 0588
This article is taken from our My Alvernia Magazine Issue #42/43. Click here to read the issue on our website or on Magzter.


