Pleurisy is an inflammation of the lining of your lungs (pleura) that causes sharp chest pains. The pain is usually worse when you breathe or cough. Viral or bacterial infections, autoimmune diseases and lung conditions are common causes of pleurisy. Some causes of chest pain are life-threatening. If you’re having chest pains, go to the nearest ER.
Pleurisy (“PLUR-uh-see”) happens when the lining (tissue layer) around your lungs or the lining on the inside wall of your chest swells up. This makes the two layers rub against each other, causing sharp pains. Pleurisy is also called pleuritis.
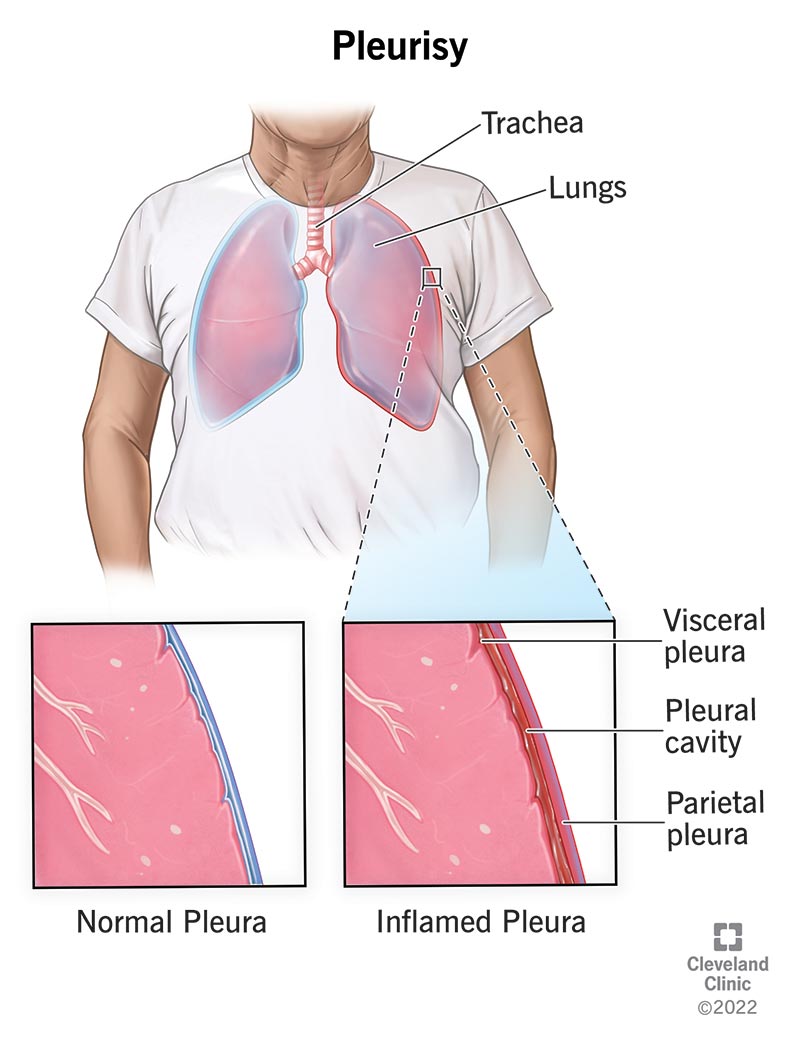
Your lungs and the inside of your chest are each lined with a thin layer called pleura. The space between them (pleural space) is filled with fluid that allows them to slide smoothly along each other when you breathe, like oil in a machine. When one or both layers become swollen (inflamed), they rub painfully against each other instead.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Pleurisy causes chest pain that’s sharp and stabbing. There are lots of different conditions that can cause chest pain, and many of them need immediate medical attention. The only way to know for sure if you have pleurisy is to get checked by your healthcare provider.
You can get pleurisy when inflammation from your lungs — caused by a virus, bacteria or other illness — moves into your pleurae, causing them to swell up and rub against each other. This can also happen if there’s a blockage (like a tumor) or damage to your lung.
Anyone can get pleurisy, but you’re at a higher risk if you:
Pleurisy can be mild or very serious. It depends on what’s causing it and whether you have additional complications.
The main symptom of pleurisy is chest pain (pleuritic pain) that feels sharp, stabbing or knife-like, coming from one specific place. It’s worse when you breathe deeply or cough and sometimes spreads to your shoulder or back. You’ll probably find yourself breathing carefully to avoid the pain.
You might also have:
If you’re otherwise healthy, you’re most likely to get pleurisy from a virus (like the flu), bacteria or other infection in your lungs. Infections can cause inflammation in your pleurae, which gives you chest pain.
You can also get pleurisy from:
While the viruses and bacteria that can cause pleurisy are contagious, pleurisy itself is not.
Being sick with a virus can make you more likely to get pleurisy. However, pleurisy isn’t a common symptom of COVID-19.
To diagnose pleurisy, your healthcare provider will listen to your lungs and ask you about your health history. They’ll ask you questions about your pain, like where it hurts, what it feels like and if anything makes it worse. They may want you to get imaging or other tests done.
Your healthcare provider uses tests to diagnose pleurisy and figure out the underlying cause. Possible tests include:
Chest X-rays can’t show pleurisy directly, but they can give your provider clues about what might be causing your symptoms, like fluid around the lungs (pleural effusion) or an infection (pneumonia).
Treatment for pleurisy depends on what’s causing it. Your healthcare provider will work with you to treat the underlying cause. They can also help you manage your pain in the meantime.
Your treatment options might include:
You can’t know if an injury or illness will lead to pleurisy, but you can reduce your risk by:
Your outlook for pleurisy depends on what’s causing it. If your pleurisy is caused by infection, it should go away as you get better. If it’s caused by an ongoing illness like cancer or an autoimmune disease, you may always have some risk of pleurisy coming back.
Very rarely, pleurisy has life-threatening complications.
If pleurisy is caused by a virus, it can go away on its own as you get over being sick. More serious underlying causes (such as cancer or other illnesses) need to be treated before pleurisy will get better.
You may have other conditions along with pleurisy, including:
Yes. If you have an illness that puts you at risk for pleural inflammation, you might get pleurisy more than once.
If you have a health condition that puts you at risk for pleurisy, talk to your healthcare provider about your concerns. Together, you can make a plan to reduce your risk. Be sure to ask what you can do at home and when you should get help for your pain.
Chest pain is a symptom of many conditions, some of them life-threatening. If you’re having unexplained chest pain, go to the nearest ER.
If you have pleurisy, you may want to ask your healthcare provider:
A note from Cleveland Clinic
The sharp, stabbing pains of pleurisy can be unbearable. You don’t have to just put up with the pain. While you treat the underlying cause of pleurisy, work with your provider to find pain relief that works for you.
Chest pain can have serious causes other than pleurisy. If you’re having unexplained chest pain, go to your nearest ER.
Last reviewed by a Cleveland Clinic medical professional on 08/16/2022.
Learn more about our editorial process.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy