Keratitis, or corneal inflammation, can have infectious or noninfectious causes. You should seek treatment immediately if you have eye pain, swelling and watery eyes. Your risk of keratitis increases if you wear contact lenses and don’t clean them properly.
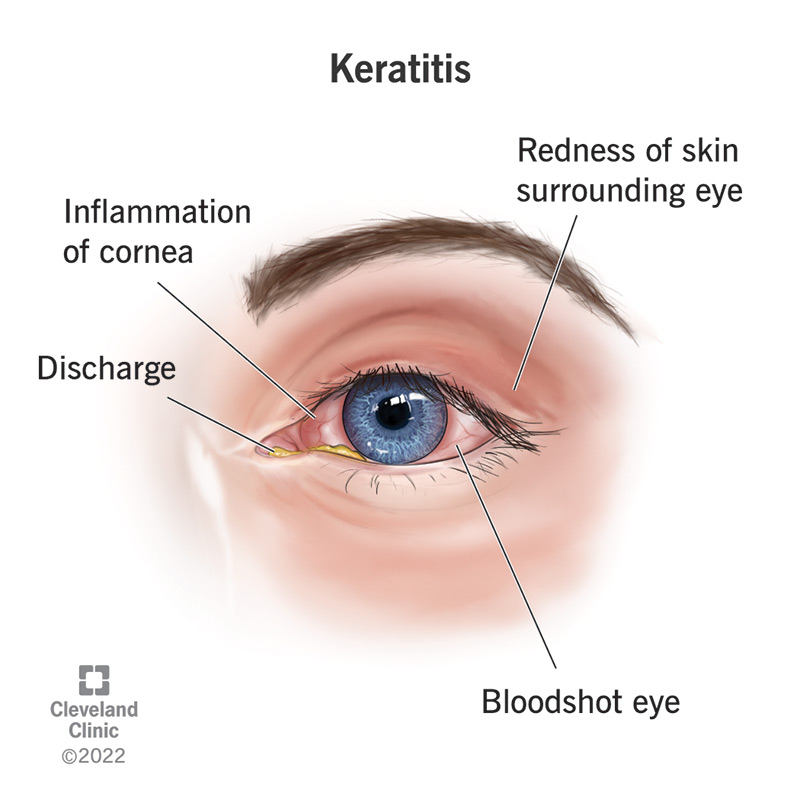
Keratitis is the medical name for inflammation of the cornea, the clear window that covers the iris and the pupil in your eye. Keratitis may cause a corneal ulcer.
Keratitis can be divided into two categories based on cause: infectious keratitis or noninfectious keratitis. Some people call infectious keratitis “microbial” keratitis.
Early signs and symptoms of keratitis include eye pain and redness. If you think you may have keratitis, you should see a healthcare provider immediately. Damage to your eyes from the disease can result in vision loss. Worldwide, keratitis causes most cases of corneal blindness.
Keratitis is a common condition that can be treated. However, outside of the U.S. and other developed countries, infectious keratitis is a significant cause of blindness. Some of the infections that cause keratitis can be transferred from person to person by touching contaminated items, coughs or sneezes.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Signs and symptoms of keratitis include:
There are infectious and noninfectious causes of keratitis.
Causes of infectious keratitis include:
Causes of noninfectious keratitis include:
Anyone can develop keratitis. However, one major risk factor for keratitis is wearing contact lenses. This is related to:
Other risk factors include:
Your eye care provider will first ask you questions about your symptoms and medical history. Then they’ll do some or all of these tests:
If you have a mild case of keratitis, your provider may suggest using lubricant eye drops and letting your eye heal on its own.
However, medication normally treats infectious keratitis. If you have a bacterial infection, you’ll get antibiotic eye drops. If you have a fungal infection, the eye drops will contain antifungal medication. If you have a virus, your provider will prescribe antiviral eye drops.
After a bacterial or viral infection clears up mostly or completely, your provider might suggest steroid eye drops to reduce swelling.
For pain, your provider might give you eye drops that dilate your eye.
If you have advanced keratitis, you may need oral medication to treat infections.
If you don’t respond to medication and keratitis is causing scars on your cornea, you may need a cornea transplant.
You’ll probably start feeling better after one or two days if you’re taking anti-infective medication. Recovery will take longer for more severe cases.
You can reduce your risk of developing keratitis by:
If you have most types of keratitis, treatment cures it. If you have a viral form of keratitis, it may come back.
You may develop glaucoma as a result of infectious keratitis. The outlook for people with fungal keratitis may be worse than the outlook for people with bacterial keratitis.
Without treatment, keratitis causes scarred corneas that can lead to vision loss.
You should always contact your healthcare provider if you have eye pain along with redness, eye watering and blurred vision.
If you received treatment and you aren’t recovering, you should contact your provider.
You may want to ask your provider questions like these:
The difference between uveitis and keratitis has to do with the location of the inflammation. Signs and symptoms are similar, but uveitis affects the uvea.
The uvea is the middle layer of the eye that includes the iris, the choroid and the ciliary body. Keratitis affects your cornea, the protective layer over your iris.
Another eye condition with similar symptoms is pink eye (conjunctivitis). It affects the conjunctiva (tissues lining the eyelid).
You could have keratoconjunctivitis if the inflammation affects both the cornea and the conjunctiva. Children often get a mild form of this condition.
A note from Cleveland Clinic
With keratitis, like other eye conditions, it’s important to get medical help early. Contact a healthcare provider any time you have eye pain, especially if you also have redness, swelling, a problem opening your eye or blurry vision. Keratitis treatment is available.
Last reviewed by a Cleveland Clinic medical professional on 12/05/2022.
Learn more about our editorial process.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy