What is Obsessive-Compulsive Disorder (OCD)?
Understanding Obsessive-Compulsive Disorder
As a child, whenever I had a bad thought (which was quite often, thank you to OCD intrusive thoughts!), or did something wrong, I would instinctively say the salvation prayer: “Jesus, come into my heart and save me.” Re-saving myself through the salvation prayer became my way to feel 'cleansed' and purified to ensure I was “okay.” I probably said that prayer 100 times a day throughout my early childhood.
While I once attributed this to my evangelical upbringing, I can now see it for what it was—some of the early signs of my OCD. This compulsion was “invisible,” an internal prayer, making it less noticeable than some of my other OCD symptoms. As I entered my teenage years, my OCD evolved, bringing more harmful compulsions as I continued to internalize and conceal them.
I was not alone in experiencing years of undiagnosed OCD symptoms. On average, individuals with OCD go about 12 years before receiving treatment (Ziegler, 2021). This delay is often due to widespread misconceptions about OCD – (OCDi s not simply being overly neat, hyper organized, or perfectionistic!). The symptoms and compulsions of OCD can be subtle and easily overlooked, which is why I am passionate about demystifying this condition. In this article, we’ll explore some fundamental aspects of OCD:
The essence of OCD.
The nature and varieties of obsessions.
An overview of compulsions and their forms.
The intricate relationship between obsessions and compulsions.
The different types of OCD.
Diagnostic criteria for OCD.
Treatment options for OCD.
My hope is that this exploration will offer insights and support to you, your child, or anyone you’re aiding in their journey with OCD. Let's dive in and unravel the complexities of this condition.
What is OCD?
Obsessive Compulsive Disorder, commonly known as OCD, is characterized by a cycle of obsessions—persistent and distressing thoughts, urges, or images—and compulsions, which are repetitive actions performed in an attempt to alleviate the anxiety caused by these obsessions. The compulsions function to try to reduce the anxiety from the obsessions. For example, excessive fear of germs may lead to constant hand-washing. While these compulsions can provide temporary relief, they often end up exacerbating the anxiety and obsessions over time.
These elements are central to the disorder, each playing a crucial role yet distinctly different in how they impact individuals. In this section, we'll delve into the nature of these elements to unravel the complexities of OCD.
Understanding Obsessions and Compulsions in OCD
In the complex world of Obsessive-Compulsive Disorder (OCD), the interplay of obsessions and compulsions forms the crux of the condition. Obsessions, those intrusive thoughts that often besiege our minds, range from intense fears of contamination to persistent worries about causing harm. They are like uninvited guests that bring distress into our daily lives.
Compulsions, on the other hand, are the actions we take in an attempt to quell the anxiety stirred by these obsessions. However, these compulsive acts – be it relentless cleaning, incessant checking of locks, or a deep-seated need for everything to be just so – often provide only a fleeting sense of relief. Far from resolving the underlying anxiety, they can, in fact, reinforce it.
Each individual's journey with OCD is uniquely their own, with varying manifestations and intensities of obsessions and compulsions. It's this very uniqueness that makes understanding and effectively treating OCD a deeply personal and intricate process. This section aims to delve into the nuanced relationship between obsessions and compulsions, illuminating the diverse ways in which they manifest and affect those living with OCD. By embracing a deeper understanding of these core elements, we can begin to unravel the complexities of this multifaceted condition.
What exactly are obsessions and compulsions?
To understand OCD, you need to understand obsessions and compulsions. Both what they are but also how they relate to one another. Obsessions and compulsions lay at the heart of the OCD diagnosis.
What are OCD obsessions?
Obsessions are those persistent, unwelcome guests in the mind, manifesting as thoughts, images, or urges that keep intruding uninvited. These obsessions are often accompanied by a torrent of anxiety, fear, or disgust, deeply conflicting with a person's values and beliefs. As someone who navigates these waters myself, I know how these thoughts can feel irrational yet overwhelmingly real at the same time.
Common Types of OCD Obsessions:
Contamination: Fears of germs or dirt, leading to excessive cleaning or avoidance behaviors.
Safety: Worries about safety or harm, often leading to repetitive checking behaviors (like ensuring doors are locked).
Symmetry and Order: A deep need for perfect order or alignment, causing distress if not met.
Intrusive Thoughts: Distressing thoughts of a violent or sexual nature, often deeply unsettling.
Hoarding: Challenges in parting with possessions, leading to clutter and accumulation.
Religious or Moral Obsessions: Troubling thoughts around these themes, leading to guilt or fear.
Fear of Illness: Constant worry about having a serious health condition.
Fear of Losing Control: Anxiety about losing self-control in various situations.
Sexual Obsessions: Unwanted sexual thoughts, images, or obsessive fears about one’s sexual orientation.
Superstitious Obsessions: Fears tied to luck, numbers, or colors.
Common Types of Intrusive Images in OCD:
Violent Imagery: Graphic images of harming oneself or others, often disturbing and unwanted.
Sexual Imagery: Unwanted and explicit sexual images that may conflict with one’s values or orientation.
Religious Blasphemy: Disturbing images related to religious sacrilege or profanity.
Distressing Scenarios: Vivid images of disastrous events, accidents, or tragedies.
Contamination Scenes: Imagery of being contaminated by germs, dirt, or toxins.
Intrusive Memories: Recurrent, distressing images from past events or traumas.
Doomsday Visions: Apocalyptic or catastrophic scenarios causing intense fear or dread.
Distorted Self-Images: Negative, exaggerated images of oneself, often related to body image or self-worth.
Compulsive Reenactments: Visualizing oneself performing compulsive acts repeatedly.
Common Types of Intrusive Urges in OCD:
Compulsive Cleaning: Overwhelming urges to clean or wash to counteract contamination fears.
Checking Urges: Impulses to check locks, appliances, or personal items repeatedly for safety.
Ordering and Arranging: Strong desires to arrange objects in a specific, often symmetrical, pattern.
Hoarding Urges: Compulsions to collect or keep items, often with no practical need or value.
Self-Harm Impulses: Urges to harm oneself, often without any intention to act on them.
Reassurance-Seeking: Persistent urges to seek validation or reassurance from others.
Avoidance Urges: Strong desires to avoid situations, places, or people that trigger OCD fears.
Repetitive Rituals: Urges to perform specific rituals or routines to alleviate anxiety or prevent a feared event.
Silent Repetitions: Compulsions to repeat words, numbers, or phrases mentally.
It's important to remember that these examples are just a snapshot of the vast and varied landscape of OCD experiences. The specific content of these thoughts, urges, and images can differ significantly from person to person. Moreover, each person's experience with OCD is unique, and many people will experience various combinations of these obsessions.
What is a compulsion?
Compulsions are often experienced as irresistible urges to perform certain behaviors or actions. Imagine being driven by an internal force that convinces you that these actions, however repetitive or time-consuming, are necessary to fend off something terrible happening! This is the daily reality for many with OCD.
A compulsion is like a temporary solution to the relentless pressure of an obsession. For instance, if a fear of contamination plagues someone, their compulsion might be to wash their hands obsessively, shower, change their clothes, or obsessively clean. This action, albeit briefly, 'neutralizes' the distress caused by the obsession. It's a short-lived respite in a continual cycle of anxiety and relief.
What does it mean to “Neutralize” an Obsession in OCD?
Neutralizing an obsession" in OCD involves performing specific actions or mental rituals to counteract distressing obsessive thoughts. This process means engaging in compulsions that the person believes will mitigate the anxiety linked to the obsession. For instance, an individual with an obsession about causing accidental harm may repeatedly check appliances or locks to 'neutralize' their fear. While these actions might offer momentary relief, they can perpetuate the cycle of anxiety and compulsive behavior, as the temporary relief reinforces the need for the compulsion.
Compulsions can be overt or covert. Overt compulsions are visible rituals, like handwashing, checking, or arranging objects meticulously. Covert compulsions, however, are internal and less apparent. They may involve mental rituals, like silently repeating phrases, counting, or reviewing memories. This internal nature of some compulsions can make OCD harder to recognize and understand, both by the individual suffering and those around them.
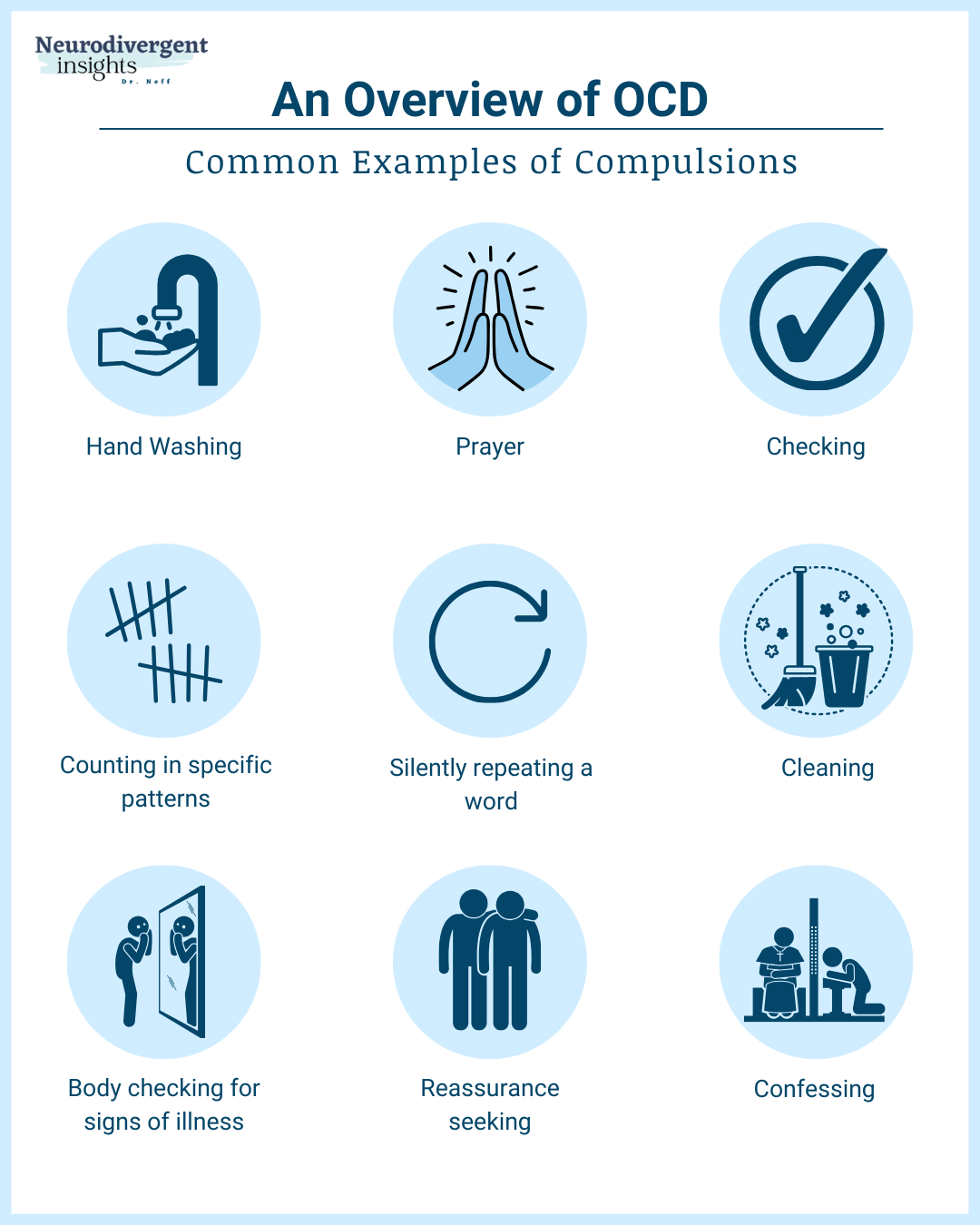
Examples of Compulsions in OCD:
Checking and Rechecking: Repeatedly verifying if doors are locked or appliances are turned off.
Counting: Feeling compelled to count objects or perform actions a specific number of times.
Handwashing: Excessive cleaning and handwashing, driven by fears of contamination.
Arranging and Ordering: Needing things to be in a specific order or symmetry.
Repeating Words or Phrases: Silently or aloud, often to counteract negative thoughts or fears.
And then there are the internal mental compulsions - the ones that aren't as visible:
Repeated mental rituals, like counting or reciting certain phrases, or prayers to ward off anxiety.
Checking and rechecking memories or information to ensure accuracy.
Thinking 'good' thoughts to neutralize 'bad' thoughts.
Compulsions, whether external or internal, significantly impact a person's daily life and functioning. They are more than just habits or quirks; they are intense responses to deeply rooted anxieties. Understanding the nature and variety of compulsions is key to empathizing with and providing support to those with OCD. It's about recognizing the struggle behind these actions and offering a hand of understanding and care.
The Dynamics of Obsessions and Compulsions
Now that we understand what obsessions are and what compulsions are, let’s bring it all together to understand how the OCD vicious cycle can take root. Understanding the intricate dynamics between obsessions and compulsions is crucial for comprehending the nature of Obsessive-Compulsive Disorder (OCD). This cycle starts with obsessions, which are intrusive, distressing thoughts or images that repeatedly invade the mind, often without warning. These obsessions can range from fears of contamination or harm to worries about symmetry or perfection, and then this kicks off the following cycle:
Intrusion of the Obsession: It begins with an unwelcome obsessive thought or image, creating significant anxiety or distress. For example, a person might have a sudden fear of having left the stove on, potentially causing a fire.
Anxiety and Distress: This obsession triggers a heightened state of anxiety. The person becomes consumed with worry, and the distressing thought dominates their mental space.
Compulsion as a Response: In an effort to alleviate this anxiety, the person then engages in a compulsion. Compulsions are repetitive behaviors or mental acts that the individual feels driven to perform. For instance, in response to the fear of the stove being left on, the individual might repeatedly check the stove.
Temporary Relief: Initially, performing the compulsion brings temporary relief from the anxiety. The act of checking reassures the person, albeit briefly, that the feared event (such as a fire) is prevented.
Reinforcement of the Obsession: However, over time, this relief reinforces the belief that the compulsion is necessary to prevent the feared event, thereby strengthening the power of the obsession. This creates a self-perpetuating cycle where the person feels compelled to perform the ritual again and again.
Cycle Continuation and Escalation: Each time the cycle repeats, the compulsions often become more time-consuming and elaborate, further entrenching the pattern and making the obsessions more intense.
Understanding this cycle is pivotal for diagnosing and treating OCD effectively. Breaking this cycle typically involves therapeutic interventions that target the obsessions (through cognitive strategies) and the compulsions (through behavioral techniques like Exposure and Response Prevention). By addressing these elements, individuals with OCD can learn to manage their symptoms and reduce the impact of the disorder on their lives.
Different Kinds of OCD
Obsessive-Compulsive Disorder (OCD) comes in many flavors. It’s one of the reasons OCD is considered a “heterogenous” because it can manifest in various forms, each with its unique characteristics and symptoms. While the different subtypes of OCD can be broadly grouped into four categories - contamination and cleaning, doubts and harm, symmetry and ordering, and intrusive thoughts and mental rituals - there are many specific presentations within these categories. Here's a look at some of the common types:
Contamination and Cleaning:
Contamination OCD: Fear of germs, dirt, leading to excessive cleaning.
Health Anxiety OCD: Obsessive concern about illness, leading to health-related behaviors.
Doubts and Harm:
Harm OCD: Intrusive thoughts about harming oneself or others, leading to checking behaviors.
Hyper responsibility OCD: Excessive responsibility for preventing harm, involving reassurance-seeking and checking.
Symmetry and Ordering:
Symmetry and Orderliness OCD: Need for order and symmetry in the environment.
Just Right OCD: A compulsion for things to feel 'just right.'
Unacceptable and Taboo Intrusive Thoughts (And Mental Rituals):
Religious or Scrupulosity OCD: Excessive concerns about religious or moral matters.
Sexual Orientation OCD: Intrusive thoughts or doubts about one's sexual orientation.
Relationship OCD: Obsessive doubts about romantic relationships.
Existential OCD: Preoccupation with philosophical questions.
Pure-O: Characterized by obsessions without visible compulsions, often involving internal mental rituals.
How is Obsessive-Compulsive Disorder Diagnosed?
Obsessive-compulsive disorder (OCD) is typically diagnosed through a combination of methods, including a comprehensive assessment of symptoms, a review of the individual's medical history, and a physical examination.
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) and the International Classification of Diseases, 11th Revision (ICD-11) criteria are often used as guidelines for diagnosing OCD. This involves an evaluation of the individual's obsessions and compulsions, which are recurrent and persistent thoughts, urges, or images that are intrusive and cause distress, as well as repetitive behaviors or mental acts that the individual feels driven to perform in response to an obsession.
In addition to meeting the criteria outlined in the DSM-5, a mental health professional may also use interviews, questionnaires, and observation to further assess the person’s symptoms and their impact on their daily life. It is also important for the individual to undergo a thorough assessment to rule out any other potential medical or mental health conditions that may be causing similar symptoms.
Overall, a diagnosis of OCD is typically made by a qualified mental health professional, such as a psychiatrist or psychologist, who has experience in diagnosing and treating OCD.
Understanding the DSM-5 Criteria for OCD Diagnosis
Navigating the diagnosis of Obsessive-Compulsive Disorder (OCD) requires an understanding of the specific criteria outlined in the DSM-5. These criteria are not mere checkboxes for professionals; they also provide valuable guidance for individuals and families seeking clarity and understanding. Let's examine these criteria in detail:
Criteria A: Presence of Obsessions, Compulsions, or Both: This criterion focuses on the experience of either obsessions (persistent, intrusive thoughts, urges, or images that can be overwhelming) or compulsions (repetitive behaviors or mental acts in response to obsessions, often adhering to strict rules).
Criteria B: Time-Consuming or Significantly Distressing: Obsessions or compulsions must be substantial enough to be time-consuming, such as taking up more than an hour each day, or they must cause significant distress or impair social, occupational, or other important areas of life. This criterion assesses the impact of these symptoms on a person's daily life.
Criteria C: Not Attributable to Another Mental Condition (or Neurodivergence): The symptoms should not be better explained by another mental disorder, such as an anxiety disorder, hoarding disorder, body dysmorphic disorder, ADHD, autism, or obsessive-compulsive personality disorder. In the latter cases, traits are more consistent with an individual's overall personality than distinct obsessions and compulsions.
Criteria D: Not Due to the Effects of a Substance: Symptoms must not be caused directly by substances like medication or drugs. This ensures the symptoms are intrinsic to OCD and not side effects of substance use.
It's important to remember that many compulsions can become internalized, making understanding the individual's subjective experience crucial. Diagnosing OCD goes beyond ticking boxes; it involves a deep understanding of how these experiences affect the person's life. This requires a nuanced and empathetic approach from a professional who can navigate these complexities with sensitivity and care.
The Misdiagnosis of OCD
The journey to a correct diagnosis of Obsessive-Compulsive Disorder (OCD) is often riddled with misunderstandings and misdiagnoses. The challenge lies not just in the visible symptoms but in the internal turmoil of fear and anxiety that characterizes OCD.
Recent research sheds light on this journey, revealing that, on average, individuals experience a significant gap—approximately 12 years—between the onset of symptoms and receiving a diagnosis. Moreover, it often takes an additional 1.5 years from the time of diagnosis to the commencement of therapy.
This substantial delay is a result of several factors: the intricate nature of OCD, the potential for symptoms to be misinterpreted, the disorder's symptom overlap with other mental health conditions, and a prevalent lack of awareness about OCD among both the general public and healthcare professionals. Such factors highlight the pressing need for enhanced education and awareness to facilitate timely and accurate diagnosis and, thus, more effective treatment for those affected by OCD.
Cultural and societal factors can also play a role in how OCD is recognized and understood. From my experience, both personal and professional, I've seen how these misunderstandings can lead to a delay in receiving the right care. Here are some key reasons why misdiagnosis is common:
Lack of Awareness: Many healthcare professionals may not have the specialized training needed to recognize OCD symptoms, often leading to misdiagnosis.
Similar Symptoms: The symptoms of OCD can closely resemble those of other mental health conditions like anxiety disorders, depression, and bipolar disorder. This similarity can lead to confusion in diagnosis. Furthermore, differentiating OCD from Autism or OCD from ADHD can be particularly challenging due to overlapping characteristics.
Stigma and Shame: The stigma surrounding OCD may cause individuals to delay seeking help, further complicating timely and accurate diagnosis.
Co-Occurrence: OCD frequently coexists with other mental health conditions and neurodivergent traits, adding complexity to identifying and diagnosing it accurately.
Pure Obsessionality (Pure-O): This subtype of OCD is characterized primarily by obsessive thoughts without overt compulsive behaviors. Often misidentified as anxiety, Pure-O's subtler manifestation can lead to it being overlooked or misdiagnosed within the broader OCD spectrum.
Contextualizing Symptoms: Sometimes, OCD symptoms might be contextually misinterpreted as personality traits or behavioral issues. This misinterpretation can stem from a complex interplay of the patient's presentation and the clinician's understanding, highlighting the need for comprehensive training and awareness in mental health.
Diversity of OCD Manifestations: OCD's diverse subtypes, such as contamination fears, hoarding behaviors, and intrusive thoughts, present a wide spectrum of symptoms. The breadth of these manifestations requires a deep and nuanced understanding, which can be challenging to achieve within the constraints of general practice.
Resource and Time Constraints: The healthcare system often operates under significant time and resource limitations. These constraints can impact the depth of assessments and evaluations for OCD, sometimes leading to missed or delayed diagnoses.
Focus on Observable Behaviors: There can be a tendency to focus on more visible symptoms, such as compulsive rituals, potentially overshadowing the less apparent but equally distressing obsessions that characterize OCD. This highlights the need for a holistic approach to assessment and diagnosis.
Cultural and Societal Factors: Cultural beliefs and societal attitudes toward mental health may influence the recognition and diagnosis of OCD, leading to misdiagnosis in some cases.
These factors illustrate the complexities involved in accurately diagnosing OCD. They point to the necessity for ongoing education, adequate resource allocation, and systemic changes within the healthcare field to better support both clinicians and patients in the journey toward accurate diagnosis and effective treatment.
How is Obsessive-Compulsive Disorder Treated?
There are a handful of treatments for OCD; both pharmaceutical approaches and psychotherapeutic approaches are highly effective in reducing OCD distress.
Treatment for OCD
The treatment of Obsessive-Compulsive Disorder (OCD) encompasses various therapeutic strategies, each aimed at empowering individuals to manage their symptoms effectively. A cornerstone of this therapeutic journey is Exposure and Response Prevention (ERP) therapy. ERP is a specialized form of cognitive-behavioral therapy that involves gradually and systematically exposing individuals to situations that trigger their OCD obsessions while not engaging in the compulsion. The goal is to learn to tolerate the anxiety without giving in to compulsive behaviors, thereby breaking the self-perpetuating cycle of obsessions and compulsions. About 80% of people with OCD respond well to ERP (Foa, 2010).
Another promising therapy is Eye Movement Desensitization and Reprocessing (EMDR). Originally developed for treating trauma, EMDR has shown potential in addressing the distressing memories and experiences often associated with OCD. By processing these experiences in a safe therapeutic setting, individuals can reduce the intensity of their OCD symptoms.
In the multifaceted approach to treating Obsessive-Compulsive Disorder (OCD), medication often plays a crucial role alongside therapies. Selective Serotonin Reuptake Inhibitors (SSRIs), in particular, are frequently prescribed to alleviate the anxiety and intrusive thoughts characteristic of OCD. For individuals with severe OCD, medication may be necessary before the person can effectively engage in therapy-based treatments. These medications act like emotional armor, enabling them to more effectively engage in treatments such as Exposure and Response Prevention (ERP) and Eye Movement Desensitization and Reprocessing (EMDR). Research has shown that a combined approach (medication and therapy) is highly effective in reducing OCD symptoms.
Treatment for OCD is highly individualized. What works for one person might not be as effective for another. Therefore, working closely with healthcare providers is crucial to finding the most suitable combination of therapies and medications. With the right treatment plan, many individuals with OCD find significant relief from their symptoms and improvement in their quality of life.
OCD Resources
There are several books that have recently come out on OCD that may be helpful if you enjoy the process of self-learning.
OCD Daniel: My child and I really appreciated this book. A great and normalizing book for children and teens to read.
The Self-Compassion Workbook for OCD: I haven’t personally read this one yet, but I’ve heard it talked about positively among several neurodivergent-affirming clinicians I know.
What to Do When Your Brain Gets Stuck: A Kid's Guide to Overcoming OCD : I tried a whole host of kid/parenting OCD books when one of my children was struggling with severe OCD; this was the one I found to be the most helpful out of the bunch.
Understanding Anxiety: A Strength-Based Perspective: This 90-minute training is part of the Neurodivergent Insights Master class series. While not explicit to OCD, this talk on anxiety provides an in-depth understanding of the role of avoidance in perpetuating anxiety; these concepts are also relevant to OCD. Moreover, Dr. Dalton unpacks Autistic anxiety vs. neurotypical anxiety, which deepens our understanding of how things like OCD and anxiety can intersect with autism.
Misdiagnosis Monday E-Books: If you’re curious to learn more about ADHD and OCD and Autism and OCD, I have two Misdiagnosis Monday ebooks available on the topic.
Affiliate Disclaimer: Please note that some of the links in this resource section are affiliate links. This means that if you click on these links and make a purchase, I may receive a small commission at no extra cost to you. I only recommend products and services that I believe in and think will be valuable to my readers. Your support helps me continue to provide valuable content on this blog.
Summary and Conclusion
In navigating the intricate world of Obsessive-Compulsive Disorder (OCD), I've realized through my own journey and in helping others that OCD is far more than a collection of rituals or habits. It's a deeply ingrained part of our mental landscape, demanding not just understanding but also genuine empathy and care tailored to each unique experience.
OCD, with its persistent, intrusive thoughts (obsessions) and the repetitive actions (compulsions) that follow, can profoundly affect our daily lives. Yet, there is hope. Treatments like Exposure and Response Prevention (ERP) therapy, along with medication, have been beacons of light for many. They offer pathways to manage the symptoms and to reclaim a sense of well-being.
In wrapping up, I want to emphasize that while OCD is undeniably challenging, it's a condition that we can navigate successfully. With the right awareness, treatment, and a community that understands and supports us, living a fulfilling life with OCD is absolutely attainable. We learn not just to cope but to thrive, finding strength and resilience in our journey with OCD.
References
Foa E. B. (2010). Cognitive behavioral therapy of obsessive-compulsive disorder. Dialogues in clinical neuroscience, 12(2), 199–207.
Ziegler, S., Bednasch, K., Baldofski, S., & Rummel-Kluge, C. (2021). Long durations from symptom onset to diagnosis and from diagnosis to treatment in obsessive-compulsive disorder: A retrospective self-report study. PloS one, 16(12), e0261169.