 Diabetic Peripheral Neuropathy is the most common complication of diabetes, and commonly leads to numbness, loss of sensation, and pain in the feet, legs, or hands. It affects the peripheral nervous system (PNS), which consists of the nerves and ganglia outside of the brain and spinal cord, connecting the central nervous system to the rest of the body.
Diabetic Peripheral Neuropathy is the most common complication of diabetes, and commonly leads to numbness, loss of sensation, and pain in the feet, legs, or hands. It affects the peripheral nervous system (PNS), which consists of the nerves and ganglia outside of the brain and spinal cord, connecting the central nervous system to the rest of the body.
What Causes Diabetic Peripheral Neuropathy?
Capillaries (small blood vessels) form the connection between veins and arteries, exchanging oxygen, nutrients, and wastes between the blood and the tissues.
Medical experts are not sure why, but it appears an excess amount of sugar in the blood (high blood sugar) weakens the walls of the capillaries that supply the nerves with oxygen and nutrients. As a result, the damaged nerves send mixed signals that appear as pain, numbness, or tingling. These signals usually begin in the toes and move slowly toward the head.
Diabetes accounts for about half of all causes of peripheral neuropathy cases in the U.S. About 60 to 70 percent of Americans with diabetes have some form of nerve damage.
Other factors that may contribute to diabetic neuropathy include:
- Inherited factors. Certain genetic traits, unrelated to diabetes, seem to make some people more susceptible to nerve disease than others.
- Nerve inflammation. An autoimmune response that occurs when the immune system mistakenly attacks a part of the body as if it were a foreign organism.
Anyone with diabetes can develop neuropathy. However, there are factors that make a person more susceptible to nerve damage:
- Blood sugar. Poor blood sugar control is the greatest risk factor for every complication related to diabetes, including nerve damage. Keeping blood sugar consistently within an acceptable range is the best way to protect the nerves and blood vessels.
- Time. The risk of diabetic neuropathy increases the longer one has diabetes, especially if the blood sugar level isn’t well controlled.
- Kidney disease. Diabetes can cause damage to the kidneys, which may increase the toxins in the blood and contribute to nerve damage.
- Weight. Anyone with diabetes and a body mass index (BMI) greater than 24 has a higher risk of developing diabetic neuropathy.
- Smoking. Smoking narrows and hardens the arteries, resulting in reduced blood flow to the legs and feet. This restricted blood flow makes it harder for wounds to heal and damages the integrity of the peripheral nerves.
What are the Symptoms of Diabetic Peripheral Neuropathy?
Although diabetic peripheral neuropathy can develop almost anywhere in the body, it usually affects the feet and legs. In rare cases, it can affect the arms, abdomen, and back. The symptoms develop slowly over several months or even years.
An early sign of diabetic peripheral neuropathy is usually a slight burning sensation, which often improves if patients control their blood sugar. However, if blood sugar levels remain high, over time a complete lack of feeling and sensation (numbness) develops in the affected area.
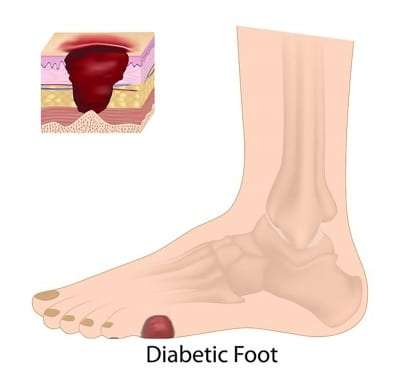
The diminished ability to feel pain in the feet often leads to more injuries. Calluses, blisters, bone and joint problems, infection, and foot ulcers may form from small, repetitive foot injuries. The injuries may be from something as simple as poorly fitting shoes, because of a lack of feeling in the feet. Therefore, it’s important that patients with diabetic peripheral neuropathy frequently inspect their feet.
Without treatment, foot problems resulting from diabetic peripheral neuropathy can become so severe that amputation of the foot and lower leg may be necessary. Furthermore, diabetic peripheral neuropathy can spread to the hands, arms, and other parts of the body.
Symptoms of diabetic neuropathy vary, depending on which nerves are affected. So, patients experience symptoms differently, which are often worse at night and can include:
Tingling
- A tingling feeling of “pins and needles” in the feet.
Pain or Increased Sensitivity
- A burning, stabbing, or shooting pain in the feet.
- Sharp pains or cramps.
- The feet are very sensitive to touch. It may hurt to have the bed covers touching the feet.
- Paresthesia (abnormal sensations such as tingling or pricking sensations).
- Patients may feel like they are wearing socks or gloves when they are not.
- The feet hurt at night.
- The feet and hands may get very cold or very hot.
Numbness or Weakness
- Numbness or reduced ability to feel pain or temperature changes.
- The feet may feel numb or even “dead.”
- Patients may not feel pain in their feet, even when there are blisters or other foot injuries.
- Cannot feel feet when walking.
- The feet and leg muscles are weak.
- Patients may feel unsteady when standing or walking.
- Patients may not feel heat or cold sensations in their feet or hands.
Other
- Loss of reflexes, especially in the ankle.
- Loss of balance and coordination.
- The feeling that the feet muscles and bones have changed shape.
- The presence of open sores (ulcers) on the feet and legs that heal very slowly.
- Serious foot problems, infections, deformities, and bone and joint pain.
- Problems can progress to affect internal organs, such as the digestive tract and heart.
How is Diabetic Peripheral Neuropathy Diagnosed?
Diabetic peripheral neuropathy can be difficult to diagnose since the disease can affect different parts of the body with symptoms resembling other medical conditions. Therefore, a thorough neurological and physical exam, as well as a complete medical history, are important to diagnosing diabetic peripheral neuropathy.
During the physical exam, the doctor is likely to check muscle strength and tone, reflexes, and the sensitivity to touch, temperature, and vibration. A complete foot exam that includes inspecting the skin of the feet, as well as foot muscles, bones, and blood flow.
Other tests the doctor may conduct include:
- Filament test. Sensitivity to touch may be tested using a soft nylon fiber (looks like a stiff piece of nylon fishing line or a hairbrush bristle) called a monofilament. The test checks for numbness in the feet.
- Nerve conduction study (NCS). A test to check the flow of electrical current through a nerve, and how quickly the nerves in the arms and legs conduct electrical signals.
- Electromyography (EMG). Often performed along with nerve conduction studies, an EMG measures the electrical discharges produced by the muscles. The test determines how the muscles respond to electrical impulses and how the nerves and muscles work together.
- Quantitative sensory testing (QST). This noninvasive test is used to assess how the nerves respond to vibration and changes in temperature. The vibration test often uses a tuning fork touching the foot to see if the patient can feel it moving.
The American Diabetes Association recommends that all people with diabetes have a comprehensive foot exam, by a doctor or by a foot specialist (podiatrist), at least once a year. Furthermore, feet should be checked for sores, cracked skin, calluses, blisters, and bone and joint abnormalities at every office visit. The doctor may also order lab tests to rule out other potential causes of peripheral neuropathy (such as a vitamin B12 deficiency).
How is Diabetic Peripheral Neuropathy Treated?
There is no known cure for diabetic peripheral neuropathy. The goal of treatment is to slow progression of the disease, relieve pain and discomfort, manage complications, and restore function.
Maintaining normal blood sugar levels is the first line of treatment. Consistently keeping blood sugar within a target range helps prevent or delay the progression of diabetic neuropathy, and may even improve some of the symptoms patients are experiencing.
There are several medications that can relieve nerve pain. The medications don’t work for everyone, though, and careful consideration of the side effects must be weighed against the benefits.
Pain-relieving medications include:
- Anti-seizure medications. Common medications that treat seizure disorders can be helpful in treating nerve pain. The side effects include drowsiness, dizziness, and swelling.
- Antidepressants. Medications that interfere with chemical processes in the brain responsible for the sensation of pain may help provide relief for mild to moderate symptoms. However, they also have many side-effects, such as dry mouth, sweating, weight gain, constipation, and dizziness.
Although these medications (such as Cymbalta, Lyrica, and Tramadol) can effectively treat nerve pain, they do not prevent the progression of the disease.
There are also several alternative therapies, such as capsaicin cream (made from chili peppers), physical therapy, and acupuncture, that may help with pain relief. The use of alternative therapies is usually in conjunction with medications, but can sometimes be effective on their own.
Alternative treatments that may help include:
- Capsaicin. When applied to the skin, capsaicin cream can reduce pain sensations in some people. A multicenter study found that topical 0.075% capsaicin cream can be effective in relieving pain associated with diabetic neuropathy. Side effects may include a burning feeling and skin irritation; however, the study found capsaicin safe and effective.
- Nutrient and vitamin supplements. Certain nutritional supplements can help treat and prevent neuropathies. Alpha-lipoic acid, a powerful antioxidant, found in some foods and occurring naturally in the body may help relieve the symptoms of peripheral neuropathy.
- Transcutaneous Electrical Nerve Stimulation (TENS). A therapy which can help prevent pain signals from reaching the brain, TENS delivers tiny electrical impulses to specific nerve pathways through small electrodes placed on the skin. Although safe and painless, TENS doesn’t work for everyone, or for all types of pain.
- Pulsed Radiofrequency Sympathectomy (PRF). Like TENS, PRF can help prevent pain signals from reaching the brain. One study comparing TENS and PRS found both TENS and PRF lumbar sympathectomy promising in relieving the pain of diabetic peripheral neuropathy. The PRF treatment seems to work better for some patients.
- Acupuncture. One study found traditional Chinese acupuncture improved nerve sensation in diabetic peripheral neuropathy. Another study involving the treatment of peripheral neuropathy showed 77% of patients noted significant improvement in their symptoms with acupuncture. Acupuncture generally doesn’t have side effects, but will likely require more than one session.
- Biofeedback: A study on the psychological assessment and treatment of neuropathic pain conditions (including diabetic peripheral neuropathy) found it is likely that cognitive-behavioral interventions will improve the quality of life in neuropathic pain conditions.
- Hypnosis. Scientists say hypnosis seems to block nerve pain receptors in the brain. Self-hypnosis trains the mind and body to help control the pain of diabetic peripheral neuropathy.
- Relaxation training. Stress can make diabetic peripheral neuropathy pain worse, so learning to relax can be helpful. Techniques like yoga may help ease stress and the level of pain.
- Orthotics. Proper footwear can help relieve excess pressure, reduce shock, help stabilize deformities, and limit the motion of joints.
Usually, peripheral neuropathy can’t be cured, but there are things the patient can do to prevent it from getting worse. Some of the measures that can help reduce the risk of diabetic neuropathy include:
- Control blood pressure. People with diabetes are more likely to have high blood pressure. Both high blood pressure and diabetes significantly increase the risk of complications, because they damage blood vessels and reduce blood flow.
- Healthy food choices. Eat a balanced diet that includes a variety of healthy foods — especially fruits, vegetables, and whole grains. Limit portion sizes to help achieve or maintain a healthy weight.
- Be active. Daily activity helps protect the heart, improve blood flow, and keep blood sugar and blood pressure under control. Non-weight-bearing activities, such as bicycling and swimming, are especially helpful for people with severe neuropathy and decreased sensation in the legs.
- Stop smoking. People who have diabetes and use tobacco in any form are more likely to develop circulation problems in the feet.
- Avoid alcohol. If using insulin, or certain oral diabetes medications that stimulate the pancreas to produce insulin, drinking alcohol can cause dangerously low blood sugar because the liver must work to remove the alcohol from the blood making it more difficult to regulate blood sugar.
Novus Spine & Pain Center
Novus Spine & Pain Center is in Lakeland, Florida, and specializes in treating diabetic peripheral neuropathy pain. By using a comprehensive approach and cutting edge therapies, we work together with patients to restore function and regain an active lifestyle, while minimizing the need for opiates.
To schedule an appointment, please contact us online, request a call back, or call our office at 863-583-4445.
Diabetic Peripheral Neuropathy Resources
Diabetic Peripheral Neuropathy (WebMD)
What Is Diabetic Neuropathy? (WebMD)
Alternative Treatments for Diabetes Nerve Pain (WebMD)
Alpha-Lipoic Acid (WebMD)
Nerve Damage (Diabetic Neuropathies) (Nat’l Institute of Diabetes and Digestive and Kidney Diseases)
Diabetic Neuropathy (Mayo Clinic)
Living with diabetes blog (Mayo Clinic)
Peripheral Neuropathy (Diabetes.org)
Diabetic Neuropathy (Nerve Problems) (Johns Hopkins)
Peripheral Neuropathy (Johns Hopkins)
Two styles of acupuncture for treating painful diabetic neuropathy (PubMed)
Acupuncture for the treatment of chronic painful peripheral diabetic neuropathy (PubMed)
Psychological assessment and treatment of patients with neuropathic pain (SpringerLink)
Treatment of painful diabetic neuropathy with topical capsaicin (PubMed)
Comparison of Transcutaneous Electrical Nerve Stimulation and Pulsed Radiofrequency Sympathectomy for Treating Painful Diabetic Neuropathy (PubMed)
Shoes and Orthotics for Diabetics (American Orthopaedic Foot & Ankle Society)
Updated: June 18, 2020
