***LISTEN TO THE PODCAST HERE***
Definition and Pathogenesis
Acute cholangitis is defined as a bacterial infection of the biliary tract and can also be termed “ascending cholangitis” as the bacteria typically ascend from the gastrointestinal tract. The most common causes for the bacterial invasion are:
- Obstruction
- Stones can be a nidus for bacterial colonization
- Benign stenosis
- Malignancy
- Instrumentation (ERCP, stent)
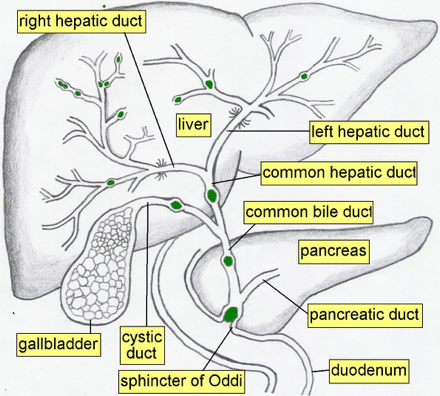
There are several anatomical areas in the biliary tree that serve as protective barriers from bacterial translocation from within the gastrointestinal tract.
- Sphincter of Oddi
- Physically blocks entry into the biliary tree
- Bile Flow
- Constantly flowing back against the ascend travel of the bacteria
- Bile acid also has bacteriostatic activity
- Biliary Mucous Secretion
- Prevents bacterial adherence to biliary tree lining
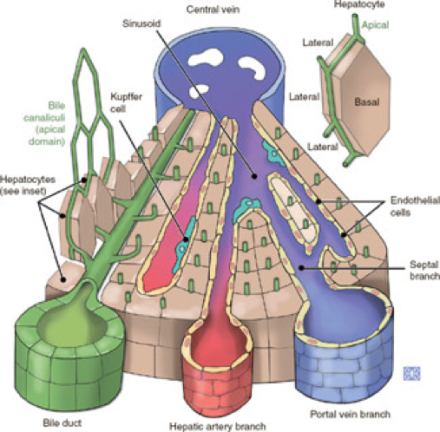
When obstruction occurs, the intrabiliary pressures rise and cause increased permeability of the biliary ductules and allows easier translocation of intestinal bacteria not only into the biliary tree, but also into systemic circulation.
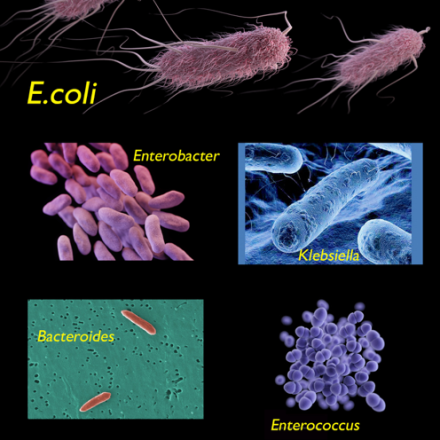
The most common pathogens isolated from bile cultures in acute cholangitis are:
- Gram Negative
- E. coli
- Klebsiella
- Enterobacter
- Gram Positive
- Enterococcus spp.
- Bacteroides spp.
Clinical Manifestations
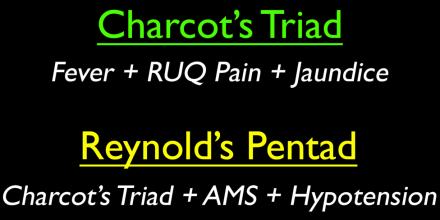
The first physician to describe acute cholangitis was Dr. Jean-Martin Charcot and has the eponomyous Charcot’s Triad named after him for right upper quadrant pain, fever, and jaundice. Fever and abdominal pain is more common (80%), than is jaundice (60%) and only 50-75% of patients have the classic triad. Dr. Benedict Reynolds, an American surgeon in the 1950s, added altered mental status and hypotension to Charcot’s Triad to describe supperative cholangitis, which now bears his name as Reynold’s Pentad and is associated with significant mortality and morbidity.
Laboratory Testing
- Complete Blood Cell Count with Differential
- Leukocytosis with neutrophil predominance
- Liver Function Tests
- Elevation in cholestatic markers
- Alkaline phosphatase (ALP)
- Gamma-glutamyl transpeptidase (GGT)
- Conjugated hyperbilirubinemia
- Blood cultures
- Elevation in cholestatic markers
Diagnosis
2013 Tokyo Guidelines for acute cholangitis breakdown into:
- Suspected
- Fever and/or rigors
- Inflammatory response
- Leukocytosis, elevated ESR or CRP
- Either:
- Jaundice
- Abnormal LFTs
- Confirmed
- Imaging showing:
- Biliary dilation without etiology
- Visualization of etiology (stone, stricture, stent)
- Imaging showing:
Imaging
Patients with suspected cholangitis, transabdominal ultrasound should be performed to evaluate for ductal dilatation, stones, and/or thickened bile duct.
Good references cases by Ultrasound Cases here (http://www.ultrasoundcases.info/case-list.aspx?cat=157).
ERCP is the definitive test of choice for cholangitis as it is both diagnostic and therapeutic and should be performed within 24-48 hours of diagnosis. This allows for biliary decompression (sphincterotomy and aspiration) and stone removal.
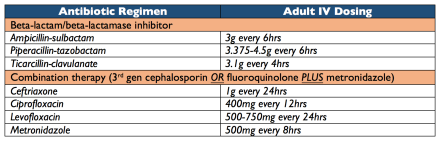
Antibiotic Management
80% of patients improve with conservative therapy of IV antibiotics while awaiting ERCP.
Alternative Drainage Procedures
If ERCP is unavailable, unsuccessful, or contraindicated, there are 2 modalities available:
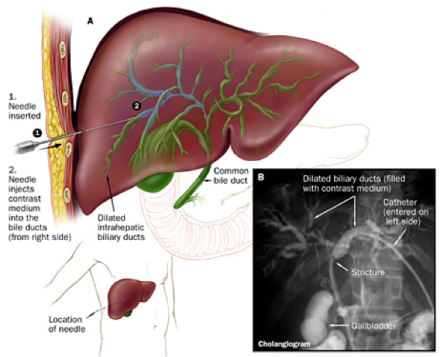
- Percutaneous Transhepatic Cholangiography (PTC)
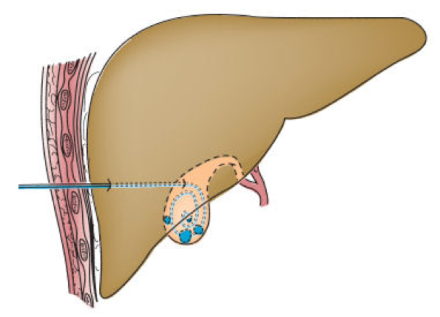
- Percutaneous Cholecystomy Tube
Prognosis and Prevention of Recurrence
Mortality associated with cholangitis have significantly improved over the last 40 years with technological, surgical, and minimally invasive techniques and have been quoted in the literature as <10% for uncomplicated and 20-30% for severe/complicated cholangitis. If the cause is due to stones, cholecystectomy should be performed once the patient is over their acute illness to prevent recurrence. If due to stricture or malignant compression, stent placement is recommended with surgical repair and decompression.
Journal of American Medicine
Article on cholangitis in 1917
References
- Sung JY, Costerton JW, Shaffer EA. Defense system in the biliary tract against bacterial infection. Digestive Diseases and Sciences. 1992;37(5):689-96. [pubmed]
- Kimura Y, Takada T, Kawarada Y. Definitions, pathophysiology, and epidemiology of acute cholangitis and cholecystitis: Tokyo Guidelines. Journal of Hepato-biliary-Pancreatic Surgery. 2007;14(1):15-26. [pubmed]
- Ohdan H, Oshiro H, Yamamoto Y. Bacteriological investigation of bile in patients with cholelithiasis. Surgery Today. 1993;23(5):390-5. [pubmed]
- van den Hazel SJ, Speelman P, Tytgat GN, Dankert J, van Leeuwen DJ. Role of antibiotics in the treatment and prevention of acute and recurrent cholangitis. Clinical Infectious Diseases : an official publication of the Infectious Diseases Society of America. 1994;19(2):279-86. [pubmed]
- Saik RP, Greenburg AG, Farris JM, Peskin GW. Spectrum of cholangitis. American Journal of Surgery. 1975;130(2):143-50. [pubmed]
- Mosler P. Diagnosis and management of acute cholangitis. Current Gastroenterology Reports. 2011;13(2):166-72. [pubmed]
- DenBesten L, Doty JE. Pathogenesis and management of choledocholithiasis. The Surgical Clinics of North America. 1981;61(4):893-907. [pubmed]
- Kiriyama S, Takada T, Strasberg SM. TG13 guidelines for diagnosis and severity grading of acute cholangitis (with videos). Journal of Hepato-biliary-pancreatic Sciences. 2013;20(1):24-34. [pubmed]
- Hui CK, Lai KC, Yuen MF, Ng M, Lai CL, Lam SK. Acute cholangitis–predictive factors for emergency ERCP. Alimentary Pharmacology & Therapeutics. 2001;15(10):1633-7. [pubmed]
- Salek J, Livote E, Sideridis K, Bank S. Analysis of risk factors predictive of early mortality and urgent ERCP in acute cholangitis. Journal of Clinical Gastroenterology. 2009;43(2):171-5. [pubmed]

Pingback: Ep-PAINE-nym | PAINE Podcast and Medical Blog