Proton pump inhibitors (PPI) in gastroesophageal reflux disease (GERD) treatment
Proton pump inhibitors (PPIs) are cornerstone medications in managing gastroesophageal reflux disease (GERD), owing to their proven effectiveness in alleviating symptoms like heartburn and regurgitation, and in healing erosive esophagitis (EE).
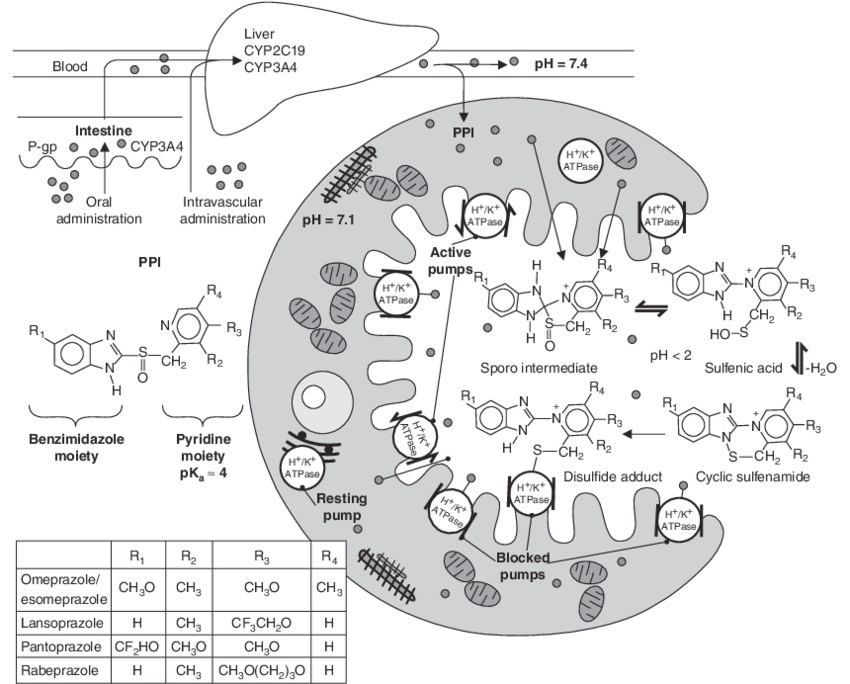
General chemical structure and mechanism of action of proton pump inhibitors (PPIs). ATPase = adenosine triphosphatase; CYP = cytochrome P450; P-gp = P-glycoprotein; pKa = negative logarithm of the acid ionisation constant.
Superiority of PPIs Over H2RAs
- Rapid Relief and Healing: A significant body of research, including meta-analyses, underscores the superiority of PPIs over H2 receptor antagonists (H2RAs) in achieving faster and more complete relief from GERD symptoms and in healing EE.
- Healing Rates: Studies indicate a healing rate of 12% per week for PPIs compared to 6% per week for H2RAs.
GERD Treatment Duration and Efficacy
- Optimal Treatment Window: Most GERD treatment studies are limited to 8–12 weeks, as symptom relief and healing rates tend to peak within this timeframe.
- Symptom Relief in Different Conditions: Approximately 70%–80% of patients with EE achieve complete symptom relief with PPIs, whereas in nonerosive reflux disease (NERD) patients, relief rates are about 50%–60%.
Comparative Efficacy of Different PPIs
- Minimal Differences Among PPIs: Meta-analyses have shown little variance in GERD symptom relief and healing rates among the seven available PPIs.
- Acid-Suppression Potency: The acid-suppression effectiveness varies across different PPIs, with esomeprazole and rabeprazole being the most potent relative to omeprazole.
Optimal Timing for PPI Administration
- Before Meals for Better Control: Enteric-coated PPIs are most effective in controlling intragastric pH when taken 30–60 minutes before meals.
- Special Cases: Dexlansoprazole’s dual delayed release formulation and the omeprazole-sodium bicarbonate combination offer flexibility in dosing times, including bedtime for the latter.
Considerations for Switching PPIs
- Incomplete Response: Switching between PPIs may benefit patients who do not fully respond to their initial PPI treatment.
- Genetic Factors: Variations in metabolism due to genetic differences in the CYP2C19 enzyme can affect PPI efficacy, although routine genetic testing is not currently recommended.
Long-Term PPI Therapy and Management Strategies
- Maintenance Therapy: Patients with severe EE or Barrett’s esophagus require ongoing PPI therapy to maintain healing and prevent relapse.
- On-Demand Therapy: For patients without EE or Barrett’s esophagus, on-demand PPI therapy may be a viable option to manage symptoms as they occur.
- Intermittent and On-Demand Efficacy: On-demand or intermittent PPI therapy can be effective for patients with NERD or non-complicated GERD, with some studies suggesting comparable outcomes to continuous therapy.
The role of proton pump inhibitors (PPI) in treating extraesophageal GERD symptoms
The application of Proton Pump Inhibitors (PPIs) for treating extraesophageal manifestations of gastroesophageal reflux disease (GERD), such as laryngopharyngeal reflux (LPR) and respiratory symptoms, has been extensively studied. While PPI therapy is a common initial approach, its efficacy in conditions like LPR, asthma, and chronic cough associated with GERD remains controversial based on recent research and meta-analyses.
PPIs and Laryngopharyngeal Reflux (LPR)
- Mixed Evidence: The benefit of PPIs in treating LPR symptoms has been inconsistent across studies. While two meta-analyses reported no significant benefit, two others identified some level of improvement in patients treated with PPIs.
- Recent Findings:
- A meta-analysis of 10 randomized controlled trials (RCTs) on PPI treatment for LPR showed a relative risk (RR) of improvement at 1.31, indicating a modest benefit of PPI therapy.
- Greater efficacy was observed in studies excluding dietary management from the treatment regimen, suggesting PPIs might have a more pronounced effect in the absence of other concurrent LPR treatments.
- Challenges in Clinical Application: Significant variability in diagnostic criteria, outcomes, and treatment durations across studies complicates the formulation of a standard recommendation for PPI use in LPR management.
Cost-effectiveness of PPI Therapy for LPR
- Reconsidering Empiric PPI Use: Initial testing with pH-impedance and esophageal manometry, rather than starting empiric PPI therapy, has been shown to reduce overall treatment costs for LPR.
- Twice-Daily vs. Once-Daily Dosing: Algorithms favoring initial twice-daily PPI dosing over once-daily dosing were associated with lower overall therapy costs in LPR management.
PPI Therapy in Asthma Patients
- Limited Benefit: Two RCTs, one involving adults and the other children, found no significant improvement in asthma symptoms with twice-daily PPI use.
- Subgroup Analysis: A specific RCT noted improved asthma symptoms in patients with GERD who had nocturnal respiratory symptoms, highlighting the potential role of PPIs in a subset of asthma patients.
PPI Use and Chronic Cough
- Questionable Efficacy: Recent studies and systematic reviews largely conclude that PPI therapy does not effectively treat chronic cough in most patients, challenging the notion of GERD as a primary cause of chronic cough responsive to PPI treatment.
Optimizing proton pump inhibitor (PPI) therapy for GERD management
Proton Pump Inhibitors (PPIs) are a cornerstone in the management of gastroesophageal reflux disease (GERD). However, achieving optimal symptom control often requires more than just prescribing these medications; it necessitates ensuring patient compliance, correct dosing schedules, and sometimes adjusting the therapy based on individual response. This article highlights key strategies for optimizing PPI therapy based on insights from various studies.
Ensuring Compliance and Correct Timing
- Timing of Doses: For effective management of GERD, it’s critical that PPIs are taken 30–60 minutes before meals. This is particularly true for once-daily dosing before the first meal and for twice-daily dosing before both the first meal and dinner.
- Compliance with Therapy: Studies have shown that patients with better symptom control are more likely to take their PPIs consistently (84% of days) compared to those with poor control (55% of days).
Benefits of Twice-Daily Dosing
- Superior Acid Control: Data from randomized trials with gastric pH monitoring indicate that twice-daily PPI therapy maintains gastric pH above 4 more effectively over a 24-hour period than once-daily double-dose therapy.
Impact of Optimized PPI Use
- Improvement in Refractory Cases: In a study of veterans with heartburn refractory to PPI treatment, about 11.4% experienced a ≥50% improvement in GERD symptoms with optimized omeprazole dosing, taken 30 minutes before breakfast and dinner.
- Efficacy in NERD Patients: Approximately 35% of patients with nonerosive reflux disease (NERD) and typical GERD symptoms responded to correctly dosed daily esomeprazole.
Educational Interventions and Dosing Adjustments
- Education on Proper Dosing: Educating patients on the proper dosing of PPIs, including the timing relative to meals, can improve symptoms and GERD-related quality of life.
- Adjusting the Dose: For some patients with persistent typical GERD symptoms, strategies such as doubling the PPI dose or switching to a different PPI have been effective.
Safety and management of long-term PPI usage for GERD
Proton Pump Inhibitors (PPIs) are widely recognized as the most effective treatment for gastroesophageal reflux disease (GERD), yet their long-term use has been a subject of debate due to potential associations with various adverse health conditions.
Advising Patients on Long-Term PPI Usage
- Effectiveness vs. Risks: PPIs are highly effective for GERD treatment. Despite studies suggesting a link between long-term PPI use and various adverse conditions (e.g., intestinal infections, pneumonia, osteoporosis-related fractures, chronic kidney disease, and more), these findings are not definitive and often contain flaws.
- Balancing Benefits and Risks: High-quality research primarily associates long-term PPI use with an increased risk of intestinal infections only. The potential for a slight increase in risk for other conditions cannot be entirely ruled out, but the benefits of PPIs in treating GERD are generally considered to outweigh these theoretical risks.
Managing Side Effects and Monitoring
- Switching PPIs for Minor Side Effects: Patients experiencing side effects such as headaches, abdominal pain, or gastrointestinal symptoms may consider switching to a different PPI formulation.
- Bone Health: There is no recommendation for increased intake of calcium or vitamin D or for routine bone mineral density monitoring in GERD patients on PPIs without additional risk factors for bone disease.
- Vitamin B12 Levels: Similarly, raising intake or monitoring serum B12 levels is not routinely advised for patients without specific risk factors for vitamin B12 deficiency.
- Kidney Function: Routine monitoring of serum creatinine levels is not recommended for patients without other kidney disease risk factors.
Special Considerations
- GERD and Clopidogrel Use: For patients with severe esophagitis (LA grade C or D) or uncontrolled GERD symptoms on clopidogrel, the benefits of PPIs are considered to outweigh the speculative cardiovascular risks.
- Renal Insufficiency: PPI treatment in patients with renal insufficiency should proceed with careful monitoring or consultation with a nephrologist.
Conclusions
- PPIs remain the treatment of choice for GERD due to their superior efficacy in symptom relief and mucosal healing. While the choice among different PPIs can be guided by their acid-suppression potency, timing of administration plays a crucial role in maximizing their effectiveness. For long-term management, both continuous and on-demand PPI therapies have their places, depending on the patient’s specific condition and response to treatment. Tailoring PPI therapy to individual needs, while considering the potential for on-demand management, provides a nuanced approach to managing GERD effectively.
- The role of PPI therapy in managing extraesophageal symptoms of GERD, such as LPR, asthma, and chronic cough, is complex and nuanced. The variability in study outcomes underscores the need for personalized treatment strategies and highlights the importance of comprehensive diagnostic assessments before initiating PPI therapy. Clinicians must balance the potential benefits of PPIs against their limitations and costs, adopting a patient-centered approach to manage extraesophageal GERD symptoms effectively.
- Optimizing PPI therapy involves a multifaceted approach that includes verifying patient compliance, ensuring proper timing of doses, and making necessary adjustments based on individual response. While the majority of patients with GERD can achieve symptom control with standard PPI therapy, a significant subset may require tailored interventions. Educating patients about the correct use of PPIs and considering dose adjustments or therapy switches can enhance the effectiveness of GERD management, leading to improved patient outcomes with minimal additional costs.
- While the debate on the safety of long-term PPI use continues, current evidence and gastroenterological consensus emphasize that the substantial benefits of PPIs in managing GERD outweigh potential risks for most patients. Personalized patient care, involving informed discussions about the benefits and theoretical risks, along with judicious management of side effects and condition-specific monitoring, remains the cornerstone of effective GERD treatment with PPI therapy.
