First introduced in 1910, hysterosalpingography (HSG) has more recently been eclipsed by the development of newer methods of imaging the female genital tract. Techniques such as endovaginal ultrasound and cross-sectional imaging, including computed tomography (CT) and magnetic resonance imaging (MRI), have now become standard for evaluating abnormalities of the female pelvis. Thus the use of HSG has shifted from the diagnosis of female pelvic disease to the evaluation of infertility. Despite the popularity of the newer imaging modalities, with the increasing rate of infertility (7.3 million women or 12% of the reproductive age population) in the United States, the number of HSGs performed per year has gradually increased.
Techniques
Indications
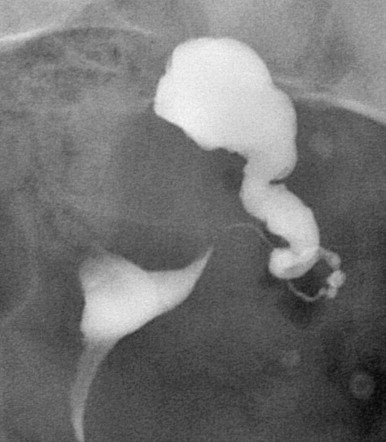
In evaluation for infertility, HSG is typically used to study the internal luminal morphology of the endocervical canal, uterine cavity, and fallopian tubes and their associated abnormalities, such as congenital anomalies, neoplasia, and inflammatory changes ( Figure 7-1 ). Within the uterus these include distortion of the endocervical canal secondary to myomas and identification of endoluminal masses such as polyps, myomas, and hyperplasia. Changes secondary to diethylstilbestrol (DES) exposure in utero can also be identified; however, this cohort of patients has now passed childbearing age. In addition to confirming tubal patency, HSG is useful in the diagnosis of various causes of tubal occlusion. These are most commonly the sequelae of pelvic inflammatory disease but also can be caused by obstructing polyps and endometriomas. Finally, HSG is used to confirm operative sterilization and to plan for reversal ( Figures 7-2 and 7-3 ). With the use of oil-soluble contrast media and selective tubal catheterization, HSG also has a potential therapeutic role in increasing the probability of pregnancy ( Box 7-1 ) .

Indications for Hysterosalpingography
- ▪
Confirmation of tubal patency in infertile patients
- ▪
Confirmation or assessment for reversal of sterilization procedures
- ▪
Filling defects within the endometrial canal
Contraindications
Although the contraindications for HSG are few, there are some instances where it cannot be performed safely ( Table 7-1 ). Active pelvic infection is considered an absolute contraindication because the retrograde injection of contrast material may cause further spread of the infection. Active vaginal bleeding is also an absolute contraindication because of the possibility of flushing clots into the peritoneal cavity, a condition that could lead to infection or endometriosis. Recent uterine or tubal surgery and uterine curettage are relative contraindications given the increased risk of intravasation. In these circumstances, HSG should not be performed for approximately 6 weeks to allow for adequate healing.
| Absolute | Relative |
|---|---|
| Active pelvic infection | Contrast media allergy |
| Active vaginal bleeding | Recent surgery |
| Pregnancy |
As expected, normal intrauterine pregnancy is an absolute contraindication. Many examiners use the “10-day rule,” which states that an HSG should not be performed if it has been longer than 10 to 12 days between the onset of menses and day of procedure; if the patient has prolonged cycles (>28 days), this time may be extended up to 13 to 15 days. If there is any question of pregnancy, a pregnancy test should be obtained before the examination.
Finally, when there is a history of contrast agent allergy, the risks versus benefits of the procedure should be weighed. To our knowledge, there have been no known deaths from a contrast allergy during HSG; however, delayed reactions such as urticaria and hypotension have been reported. In the case of a previous allergy to iodinated contrast media, the patient may be premedicated to help prevent allergic reaction. The American College of Radiology guidelines are 50 mg of prednisone orally 13 hours, 7 hours, and 1 hour before contrast administration, in addition to 50 mg of diphenhydramine orally 1 hour before the study. The use of low osmolar contrast agents significantly decreases the risk of reactions to the administration of contrast agents. Alternatively, one could consider using an alternative noniodine-containing contrast medium, such as gadolinium.
Equipment
Injection Devices
Although many different HSG injection devices have been developed, there are three main types in use today. The choice of which device to use is primarily based on the individual examiner’s preference. The three most popular injection devices are the metal cannula, the cervical vacuum cup, and the balloon catheter ( Figure 7-4 ).
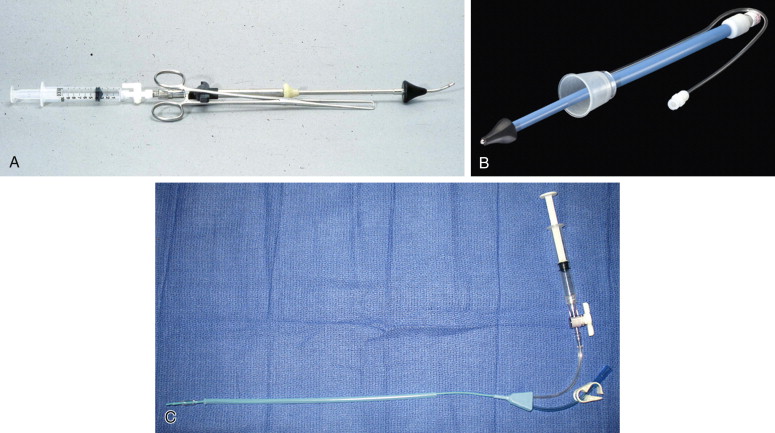
The metal cannula is the historic preference for many radiologists and gynecologists. It is a rigid cannula with a plastic acorn tip, of varying sizes, to occlude the cervical os. A tenaculum is used to stabilize the cervix with countertraction while the cannula is inserted into the os. This technique has the advantage of giving one the ability to manipulate the uterus, which allows repositioning for optimal visualization of an anteverted or retroverted uterus. The use of the tenaculum, however, can cause pain, bleeding, and cervical laceration. For this reason, the cervical vacuum cup and balloon catheter techniques were developed, each of which offers various advantages and disadvantages over the metal cannula.
The cervical vacuum cup is a plastic device composed of a cervical adaptor with two injection tubes (one for injection and one for vacuum). It uses suction to adhere to the cervix and hold the central cannula in the cervical os during injection. The catheter comes in three cup sizes: 25-, 27-, and 30-mm diameters. This device has the advantage of decreased pain and ease of use; however, it does not allow easy manipulation of the uterus during the study.
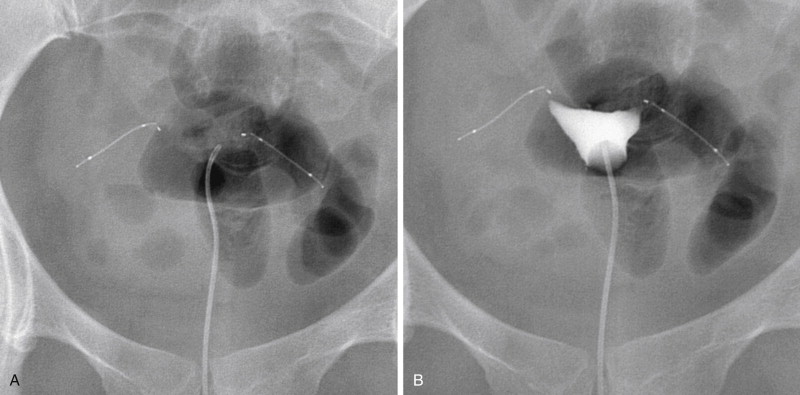
The balloon catheter is currently the most popular injection device; it is composed of a soft, flexible cannula, available in 5- and 7-French sizes. The catheter is placed through the cervical os. Catheterization is facilitated by passing the catheter through a short, rigid plastic sheath. The balloon is then slowly inflated in the lower uterine segment to prevent inadvertent removal of the cannula during the examination. By using a flexible catheter instead of the rigid cannula, patient discomfort is reduced. One potential drawback, however, is that the inflated balloon can obscure the lower uterine segment. By inflating the balloon in the cervical canal, visualization of the lower uterine segment can be improved; however, this may increase pain or the frequency of vasovagal reaction. An alternative technique is to inflate the balloon in the uterus, inject contrast material until the fallopian tubes are visualized, then deflate the balloon, and inject additional contrast to better visualize the lower uterine segment and endocervical canal as the catheter is removed. Similar to the cervical vacuum cup, the balloon catheter does not allow the examiner to apply traction to the uterus for optimal visualization. Oblique images will help with this technical limitation.
Multiple recent studies have compared the metal cannula with the newer injection devices for ease of use, fluoroscopic time, and patient discomfort. The use of the cervical vacuum cup has been reported to decrease procedure and fluoroscopic time, pain, and volume of contrast agent compared with the metal cannula. Similar studies comparing the use of metal cannulas with balloon catheters reported that the use of the latter also results in decreased fluoroscopic time, pain, and amount of contrast agent used. When the cervical vacuum cup was compared with the balloon catheter, patients better tolerated the use of the balloon catheter over the cervical cup; however, the use of the cervical cup resulted in reduced radiation.
Contrast Media
There are two main classes of contrast media that can be used for HSG: water soluble and oil soluble. Oil-soluble agents have fallen out of favor in part because of the theoretical risk of clinically significant oil droplet emboli migrating to the lungs and, more importantly, the brain (right to left shunting). Although rarely reported with earlier, more viscous oily agents such as Lipiodol (Guerbet, Villepinte, France), we are unaware of such complications with the currently available less viscous oily agent Ethiodol (Guerbet).
Virtually any water-soluble contrast agent containing approximately 300 to 350 mg I/mL can be used. These include meglumine diatrizoate, iopamidol, and iohexol. Occasionally a small amount of oil is administered via the uterine catheter after the HSG as a potential aid to fertility.
Technique Description
HSG is often performed as a joint effort between the Division of Reproductive Endocrinology, Department of Obstetrics and Gynecology, and the Department of Radiology. It is recommended that patients take a nonsteroidal antiinflammatory analgesic 1 hour before the procedure because pain and pelvic cramping are the main side effects of HSG. Before starting the procedure, the patient is asked to empty her bladder. The patient then lies supine on the fluoroscopic table in the lithotomy position. A sterile double-bladed metal speculum is inserted into the vagina. Alternatively a plastic speculum may be used and offers the advantage of being radiolucent. Once the cervix is exposed, povidone–iodine is used to prep the cervix. Any excess povidone–iodine should be wiped away because it can act as an irritant.
A scout radiograph is typically not necessary because clinically significant pelvic calcifications or other densities will be visualized with fluoroscopy before contrast administration. Contrast medium is then slowly injected while imaging under intermittent fluoroscopy. At least three to five spot radiographic films are recommended. An anteroposterior spot radiograph is obtained during early uterine filling to detect small endometrial lesions that might be obscured by larger amounts of contrast media. Next a spot radiograph documenting complete filling of the uterus and early filling of the fallopian tubes before peritoneal spill is taken. Finally a spot radiograph demonstrating free bilateral peritoneal spill is taken to document tubal patency. Bilateral oblique spot radiographs may also be obtained for improved assessment of uterine pathology and for optimal visualization of the fallopian tubes. As described earlier, when using the balloon catheter, a postdeflation radiograph should be obtained to better evaluate the lower uterine segment and endocervical canal. With any injection device, if endometrial or endocervical pathology is suspected, postdrainage films should be obtained.
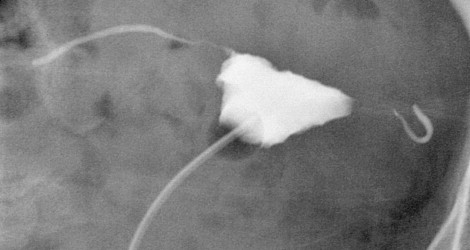
Once there is evidence of free intraperitoneal spill, contrast administration is discontinued. Typical volumes of administered contrast media range from 5 to 10 mL, but it is not unusual to instill 20 to 50 mL if the uterine cavity is enlarged secondary to myomas or previous pregnancies. It is important to use adequate volumes of contrast media to definitively visualize free intraperitoneal extension of contrast media ( Figure 7-5 ). Conversely, administration of an excessive amount of contrast media into a hydrosalpinx increases the risk of tuboovarian abscess; thus care is necessary. If at any time during the examination there is evidence of venous, lymphatic, or interstitial myometrial intravasation, contrast medium administration is immediately discontinued secondary to the increased risk of infection and pain ( Figure 7-6 ).