To reduce the risk of infection, you should have a shower on the morning of surgery. Remove all make up, body piercings, jewellery and nail varnish including acrylic nails.
Fasting guidelines
You will need to fast for 6 hours for solid foods before your operation. Solid foods include milk and milk products. You are allowed clear fluids up to 2 hours before your operation. Clear fluids include water, cordial e.g. MiWadi, isotonic sports drinks, black tea or black coffee. Drinks that are fizzy, contain ‘bits’ or are cloudy are not suitable. If you are a diabetic, it is best to just drink water.
If your caesarean section is planned for the morning:
You should not eat solid foods after 2am. You can drink clear fluids up until 6am. Take the Omeprazole tablet with a sip of water at or before 6am.
If your caesarean section is planned for the afternoon:
You are strongly advised to eat a light breakfast at or before 6am so that you will not be fasting for too long. A light breakfast would be tea, toast, cereal and/or fruit. No solid foods are allowed from 6am onwards but you can continue to drink clear fluids until 10am. Take the tablet Omeprazole with a sip of water at or before 10am.
What to bring to the hospital?
Please bring some chewing gum with you to use AFTER your operation. Chewing gum has been shown to improve gut function after an operation.
For you: dressing gown, slippers, disposable underwear, sanitary towels, bath towel, pyjamas, general toiletries.
For baby: nappies, cotton wool, bath towel, baby-grows, vests, cardigans, baby hats and water-based baby wipes.
In a separate bag specific for theatre – two cotton hats or one knitted hat and a nappy. If you wear contact lens please bring a case to place the lens.
Please do not bring: a large amount of money, valuables such as a laptop or jewellery. The hospital will not be responsible for any valuables that are lost during your stay.
What happens in the hospital on the day of surgery?
You should attend the admissions office in the main reception at the time given to you. You will be admitted to a ward area where a midwife will prepare you for theatre. Unfortunately, it is not possible to give you an exact time for surgery as we are unable to predict how busy the Delivery Suite and the operating theatre will be on the day.
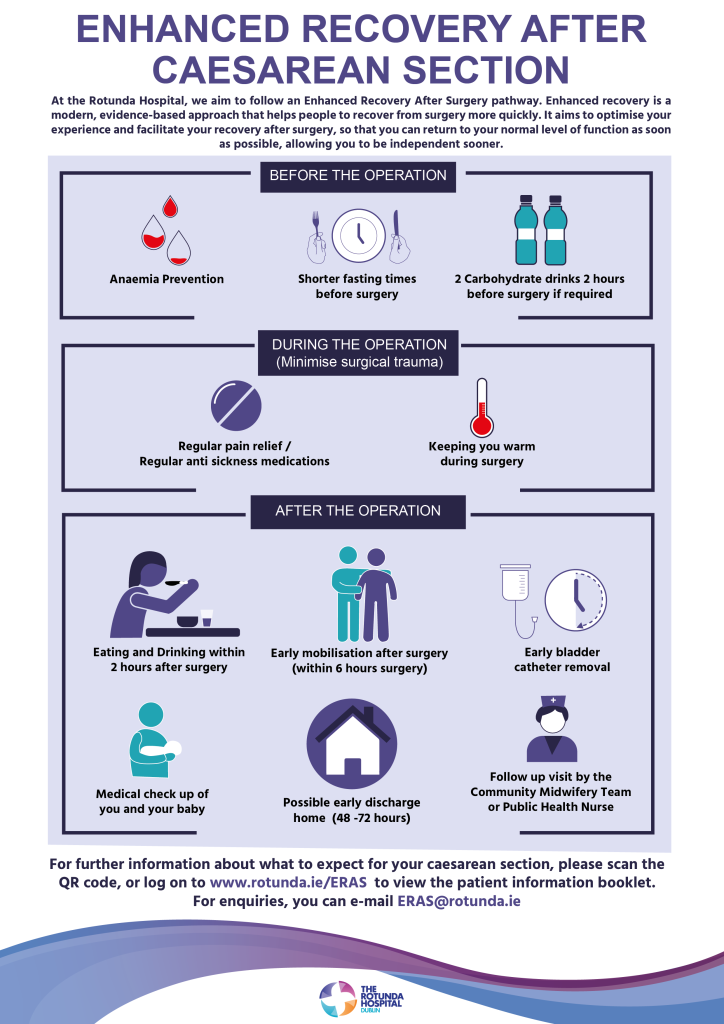
If your operation is delayed for any reason for more than 2 hours, you may be offered a carbohydrate drink. The staff looking after you on the ward will let you know if you can have this drink and provide you with it.
The midwife will ask you questions regarding allergies and your general health. Please let the midwife know if you are allergic to any medications, to fish or dairy products or if you have a latex allergy. If you have an allergy, you will be given an allergy band for your wrist to highlight the allergy.
The midwife will perform a full set of observations including listening to your baby’s heart beat. Occasionally an ultrasound scan may be done to confirm what way your baby is lying in the womb. You will be asked to put on a theatre gown and to wear surgical stockings which help to prevent a blood clot in your leg. A blood sample will be taken to check your blood group. The midwife will check that you have signed the consent form for surgery. You will get an identification armband with your name, date of birth, and hospital number. When it is time for surgery, you will walk to theatre with a member of staff from the ward and your partner.